The Skeletal System
Unit Outline
A. Bone Tissue and the Skeletal System
Part 1: The Functions of the Skeletal System
Learning Objectives
At the end of this unit, you should be able to:
- Describe the functions of the skeletal system and the five basic shapes of human bones.
- Describe the structure and histology of the skeletal system.
- Define and identify the following parts of a long bone: diaphysis, epiphysis, metaphysis, articular cartilage, periosteum, medullary cavity, and endosteum.
- Compare the composition and function of compact bone versus spongy bone.
- Define ossification, compare intramembranous ossification with endochondral ossification, describe how a long bone grows in length and width, and specify how various factors might affect the rate of ossification and, by extension, the height of a mature individual.
- Describe four types of bone fractures.
A. Bone Tissue and the Skeletal System
Your skeleton is a structure of living tissue that grows, repairs, and renews itself. The bones within it are dynamic and complex organs that serve a number of important functions, including some necessary to maintain homeostasis.
The skeletal system forms the rigid internal framework of the body. It consists of the bones, cartilages, and ligaments. Bones support the weight of the body, allow for body movements, and protect internal organs. Cartilage provides flexible strength and support for body structures such as the thoracic cage, the external ear, and the trachea and larynx. At joints of the body, cartilage can also unite adjacent bones or provide cushioning between them. Ligaments are the strong connective tissue bands that hold the bones at a moveable joint together and serve to prevent excessive movements of the joint that would result in injury. Providing movement of the skeleton are the muscles of the body, which are firmly attached to the skeleton via connective tissue structures called tendons. As muscles contract, they pull on the bones to produce movements of the body. Thus, without a skeleton, you would not be able to stand, run, or even feed yourself!
Each bone of the body serves a particular function, and therefore, bones vary in size, shape, and strength based on these functions. For example, the bones of the lower back and lower limb are thick and strong to support your body weight. Similarly, the size of a bony landmark that serves as a muscle attachment site on an individual bone is related to the strength of this muscle. Muscles can apply very strong pulling forces to the bones of the skeleton. To resist these forces, bones have enlarged bony landmarks at sites where powerful muscles attach. This means that not only the size of a bone, but also its shape, is related to its function. Bones are also dynamic organs that can modify their strength and thickness in response to changes in muscle strength or body weight. Thus, muscle attachment sites on bones will thicken if you begin a workout program that increases muscle strength. Similarly, the walls of weight-bearing bones will thicken if you gain body weight or begin pounding the pavement as part of a new running regimen. In contrast, a reduction in muscle strength or body weight will cause bones to become thinner. This may happen during a prolonged hospital stay, following limb immobilization in a cast, or going into the weightlessness of outer space. Even a change in diet, such as eating only soft food due to the loss of teeth, will result in a noticeable decrease in the size and thickness of the jaw bones.
You can watch the above Crash Course video on bones by clicking the link or scanning the QR code below!

Part 1: The Functions of the Skeletal System
Bone, or osseous tissue, is a hard, dense connective tissue that forms most of the adult skeleton, the support structure of the body. In the areas of the skeleton where bones move (for example, the rib cage and joints), cartilage, a semi-rigid form of connective tissue, provides flexibility and smooth surfaces for movement. The skeletal system is the body system composed of bones and cartilage and performs the following critical functions for the human body:
- supports the body
- facilitates movement
- protects internal organs
- produces blood cells
- stores and releases minerals and fat
Support, Movement and Protection
The most apparent functions of the skeletal system are the gross functions—those visible by observation. Simply by looking at a person, you can see how the bones support, facilitate movement, and protect the human body.
Just as the steel beams of a building provide a scaffold to support its weight, the bones and cartilage of your skeletal system compose the scaffold that supports the rest of your body. Without the skeletal system, you would be a limp mass of organs, muscle, and skin.
Bones also facilitate movement by serving as points of attachment for your muscles. While some bones only serve as a support for the muscles, others also transmit the forces produced when your muscles contract. From a mechanical point of view, bones act as levers, and joints serve as fulcrums (Figure 10.1). Unless a muscle spans a joint and contracts, a bone is not going to move.

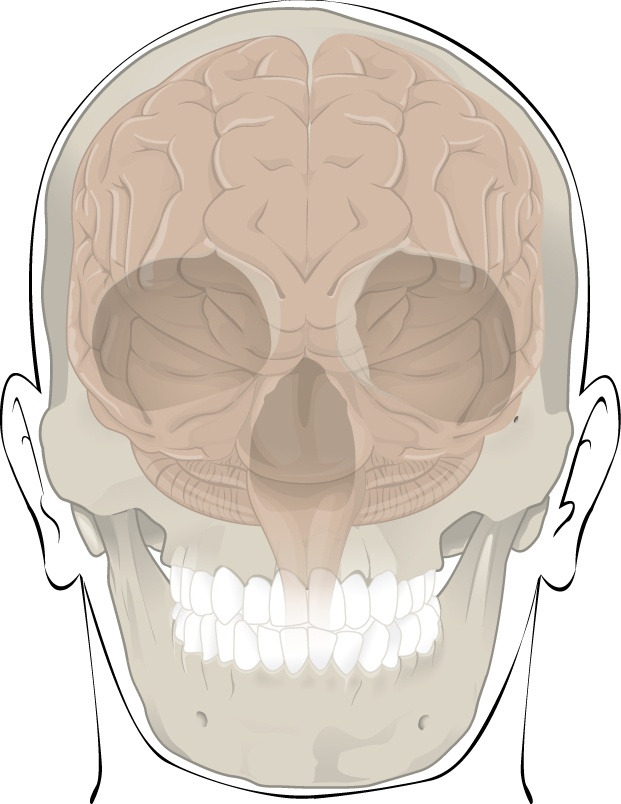
Bones also protect internal organs from injury by covering or surrounding them. For example, your ribs protect your lungs and heart; the bones of your vertebral column (spine) protect your spinal cord; and the bones of your cranium (skull) protect your brain (Figure 10.2).
Mineral Storage, Energy Storage, and Hematopoiesis
On a metabolic level, bone tissue performs several critical functions. For one, the bone matrix (ground substance) acts as a reservoir for a number of minerals important to the functioning of the body, especially calcium, and phosphorus. These minerals, incorporated into bone tissue, can be released back into the bloodstream to maintain levels needed to support physiological processes. Calcium ions, for example, are essential for muscle contractions and controlling the flow of other ions involved in the transmission of nerve impulses.
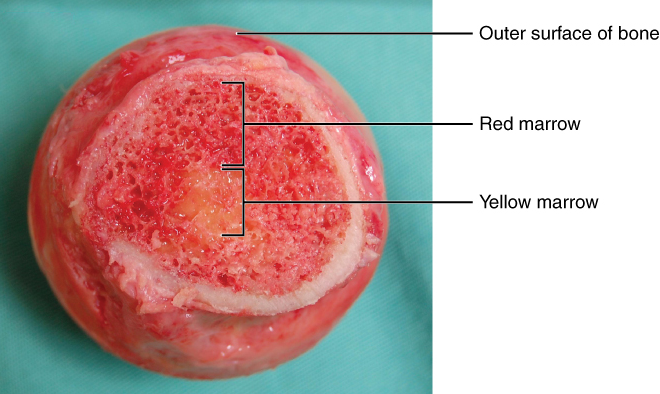
Bone also serves as a site for fat storage and blood cell production. The softer connective tissue that fills the interior of most bone is referred to as bone marrow (Figure 10.3). There are two types of bone marrow: yellow marrow and red marrow. Yellow marrow contains adipose tissue; the triglycerides stored in the adipocytes of the tissue can serve as a source of energy. Red marrow is where hematopoiesis—the production of blood cells—takes place. Red blood cells, white blood cells, and cell fragments called platelets are all produced in the red marrow.
Test Your Knowledge
I. Specify the ways that the skeletal system functions in the human body.
II. Explain how the skeletal “protects” and “supports” the human body.
Part 2: Bone Classification
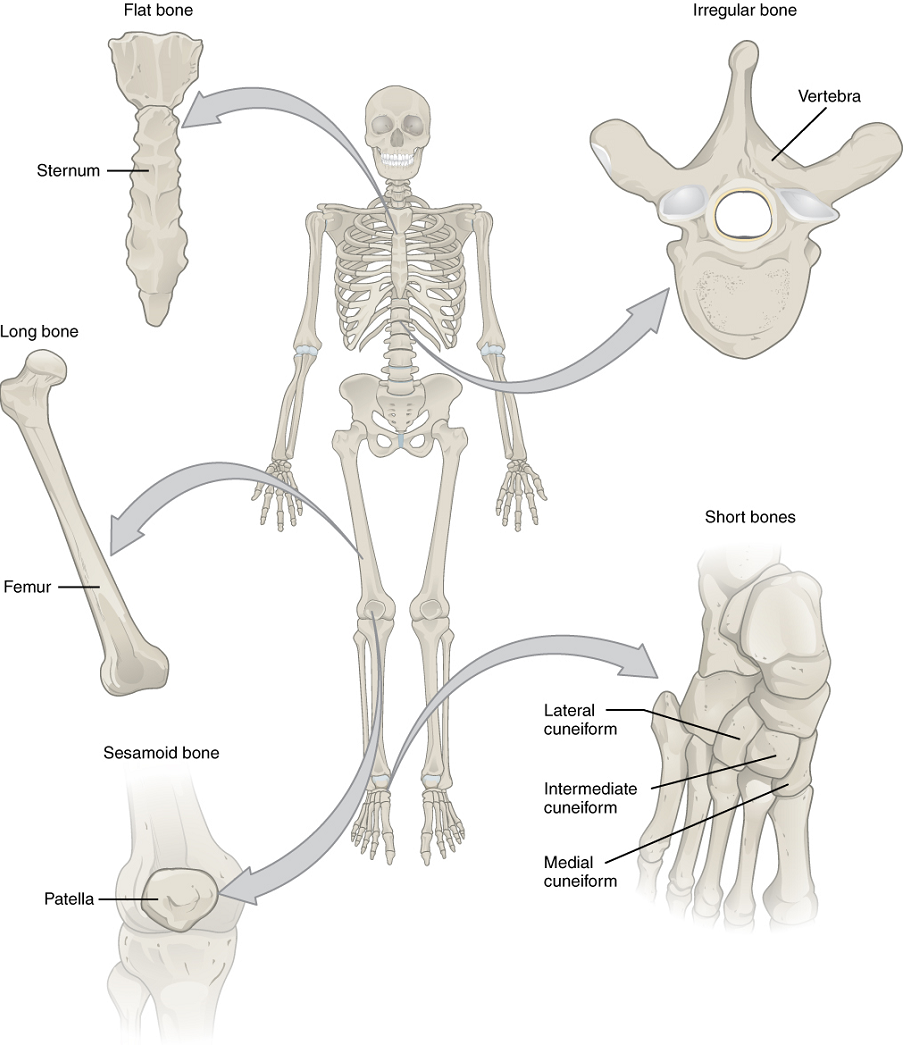
The 206 bones that compose the adult skeleton can be divided into five categories based on their shapes (Figure 10.4). Their shapes and their functions are related such that each categorical shape of bone has a distinct function.
Long Bones: A long bone is cylindrical in shape, with a diameter smaller than its height. Keep in mind, however, that the term describes the shape of a bone, not its size. Long bones are found in the arms (humerus, ulna, and radius) and legs (femur, tibia, and fibula), as well as in the fingers (metacarpals and phalanges) and toes (metatarsals and phalanges). Long bones function as levers; they move when muscles contract.
Short Bones: A short bone is one that is cube-like in shape, being approximately equal in length, width, and thickness. The only short bones in the human skeleton are in the carpals of the wrists and the tarsals of the ankles. Short bones provide stability and support as well as some limited motion.
Flat Bones: The term “flat bone” is somewhat of a misnomer because, although a flat bone is typically thin, it is also often curved. Examples include the cranial bones of the skull, the scapulae (shoulder blades), the sternum (breastbone), and the ribs. Flat bones serve as points of attachment for muscles and often protect internal organs.
Irregular Bones: An irregular bone is one that does not have any easily characterized shape and therefore does not fit any other classification. These bones tend to have more complex shapes, like the vertebrae that support the spinal cord and protect it from compressive forces. Many facial bones, particularly the ones containing sinuses, are classified as irregular bones.
Sesamoid Bones: A sesamoid bone is a small, round bone that, as the name suggests, is shaped like a sesame seed. These bones form in tendons (the sheaths of tissue that connect bones to muscles) where a great deal of pressure is generated in a joint. The sesamoid bones protect tendons by helping them overcome compressive forces. Sesamoid bones vary in number and placement from person to person but are typically found in tendons associated with the feet, hands, and knees. The patellae (singular = patella) are the only sesamoid bones found in common with every person.
Table 10.1 reviews bone classifications with their associated features, functions, and examples.
| Bone classification | Features | Function(s) | Examples |
|---|---|---|---|
| Long | Cylinder-like shape, longer than it is wide | Leverage | Femur, tibia, fibula, metatarsals, humerus, ulna, radius, metacarpals, phalanges |
| Short | Cube-like shape, approximately equal in length, width, and thickness | Provide stability & support while allowing for some motion | Carpals, tarsals |
| Flat | Thin and curved | Points of attachment for muscles; protectors of internal organs | Sternum, ribs, scapulae, cranial bones |
| Irregular | Complex shape | Protect internal organs | Vertebrae, facial bones |
| Sesamoid | Small and round; embedded in tendons | Protect tendons from compressive forces | Patellae |
Test Your Knowledge
Part 3: Bone Structure
Bone tissue (osseous tissue) differs greatly from other tissues in the body. Bone is hard and many of its functions depend on that characteristic hardness. Later discussions in this chapter will show that bone is also dynamic in that its shape adjusts to accommodate stresses. This section will examine the gross anatomy of bone first and then move on to its histology.
Gross Anatomy of Bone
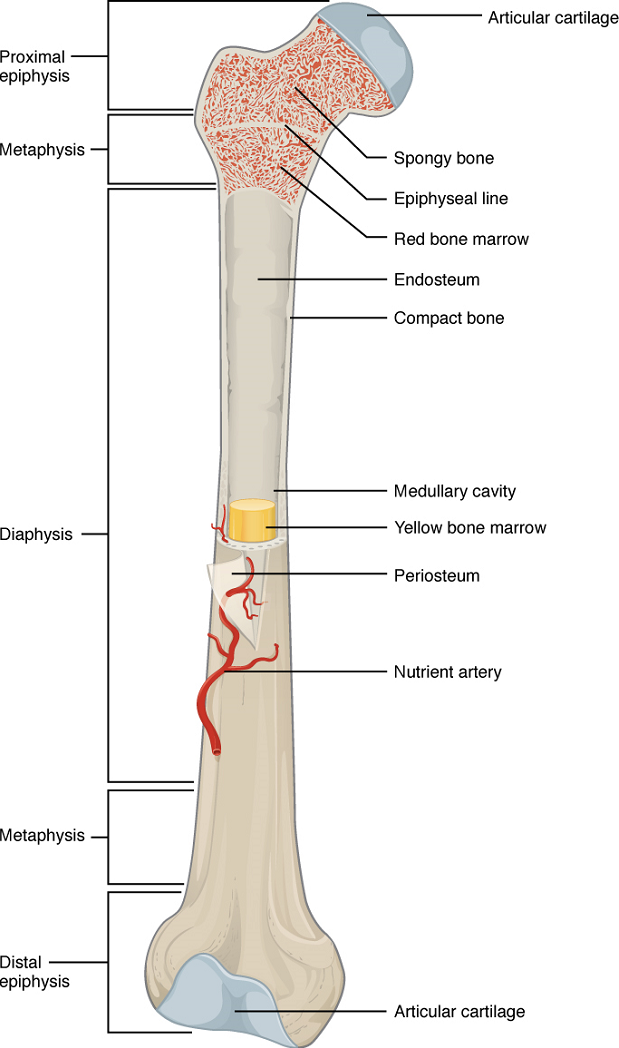
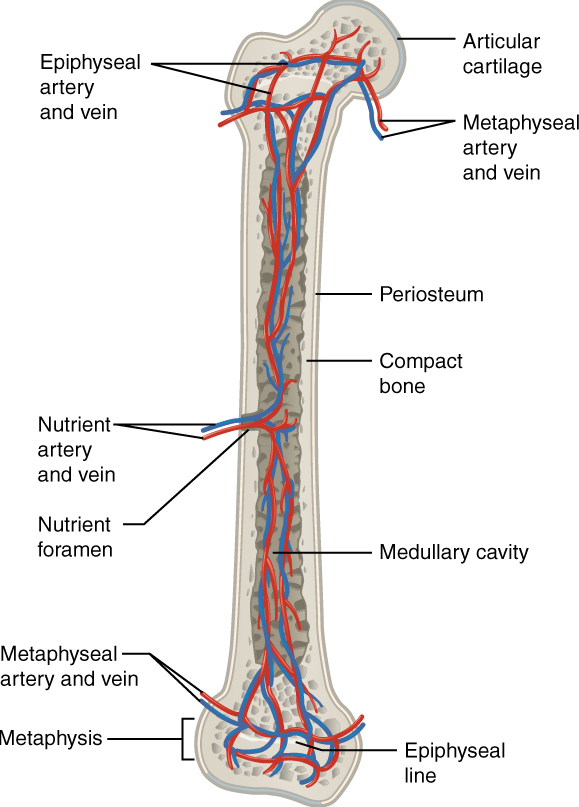
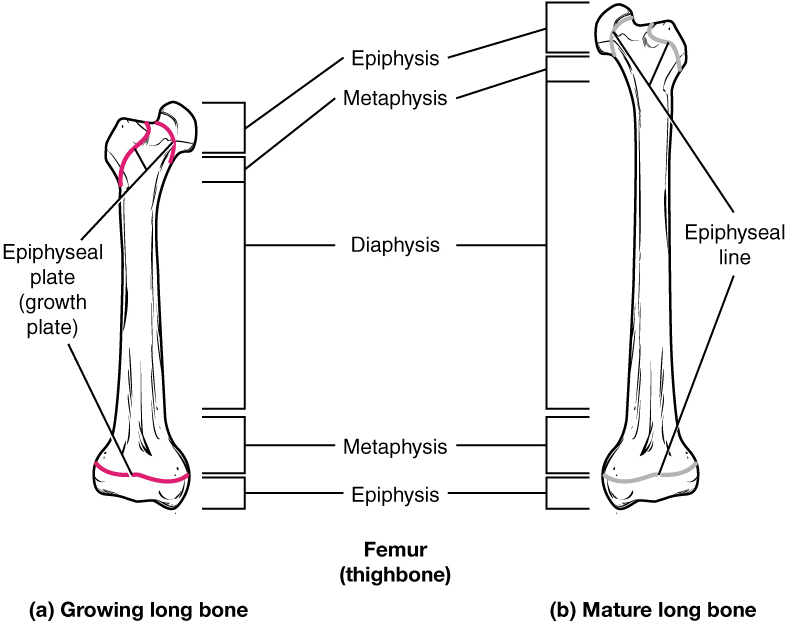
The structure of a long bone allows for the best visualization of all of the parts of a bone (Figure 10.5). A long bone has two parts: the diaphysis and the epiphysis. The diaphysis is the tubular shaft that runs between the proximal and distal ends of the bone. The hollow region in the diaphysis is called the medullary cavity, which is filled with yellow marrow. The walls of the diaphysis are composed of dense and hard compact bone. The wider section at each end of the bone is called the epiphysis (plural = epiphyses), which is filled with spongy bone. Red marrow fills the spaces in the spongy bone.
Each epiphysis meets the diaphysis at the metaphysis, the narrow area that contains the epiphyseal plate (growth plate), a layer of hyaline (transparent) cartilage in a growing bone. When the bone stops growing in early adulthood (approximately 18–21 years), the cartilage is replaced by osseous tissue and the epiphyseal plate becomes an epiphyseal line.
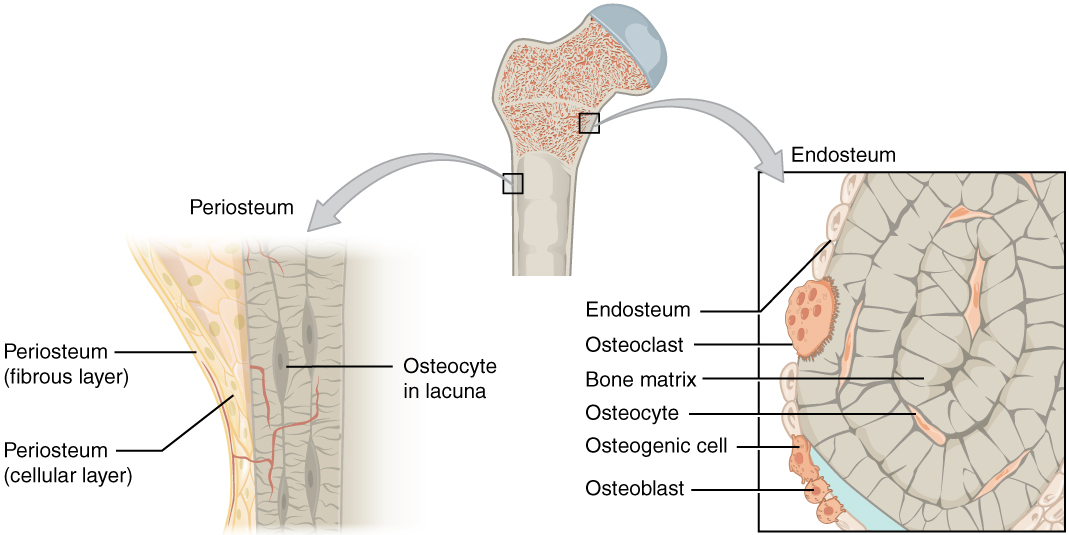
The medullary cavity has a delicate membranous lining called the endosteum (end- = “inside”; oste- = “bone”), where bone growth, repair, and remodeling occur. The outer surface of the bone is covered with a fibrous membrane called the periosteum (peri– = “around” or “surrounding”). The periosteum contains blood vessels, nerves, and lymphatic vessels that nourish compact bone. Tendons and ligaments also attach to bones at the periosteum. The periosteum covers the entire outer surface except where the epiphyses meet other bones to form joints (Figure 10.6). In this region, the epiphyses are covered with articular cartilage, a thin layer of cartilage that reduces friction and acts as a shock absorber.
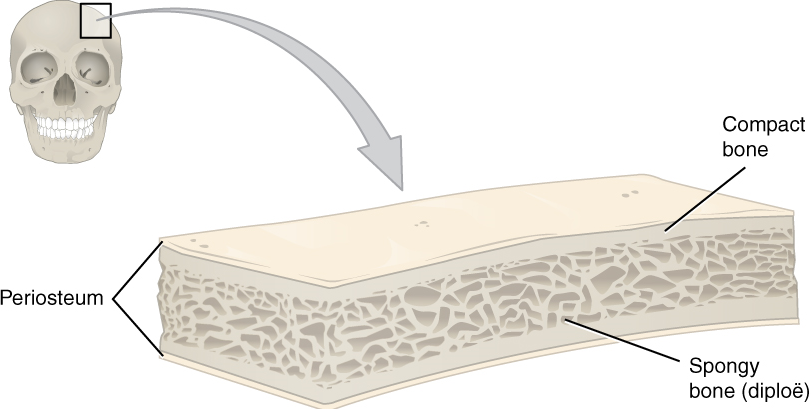
Flat bones, like those of the cranium, consist of a layer of diploë (spongy bone), lined on either side by a layer of compact bone (Figure 10.7). The two layers of compact bone and the interior spongy bone work together to protect the internal organs. If the outer layer of a cranial bone fractures, the brain is still protected by the intact inner layer.
Bone Cells and Tissue
Bone contains a relatively small number of cells entrenched in a matrix of collagen fibers that provide a surface for inorganic salt crystals to adhere. These salt crystals, made of a substance called hydroxyapatite, form when calcium phosphate and calcium carbonate combine with other inorganic salts and solidify (i.e., calcify) on the collagen fibers. The crystals give bones their hardness and strength, while the collagen fibers give them flexibility.
Although bone cells compose a small amount of the bone volume, they are crucial to the function of bones. Four types of cells are found within bone tissue: osteoblasts, osteocytes, osteogenic cells, and osteoclasts (Figure 10.8).
The osteoblast is the bone cell responsible for forming new bone and is found in the growing portions of bone, including the periosteum and endosteum. Osteoblasts, which do not divide, synthesize and secrete the collagen matrix and calcium salts. As the secreted matrix surrounding the osteoblast calcifies, the osteoblast becomes trapped within it; as a result, it changes in structure and becomes an osteocyte, the primary cell of mature bone and the most common type of bone cell. Each osteocyte is located in a space called a lacuna and is surrounded by bone matrix. Osteocytes maintain the mineral concentration of the matrix. Like osteoblasts, osteocytes lack mitotic activity. They can communicate with each other and receive nutrients via long cytoplasmic processes that extend through canaliculi (singular = canaliculus), channels within the bone matrix.
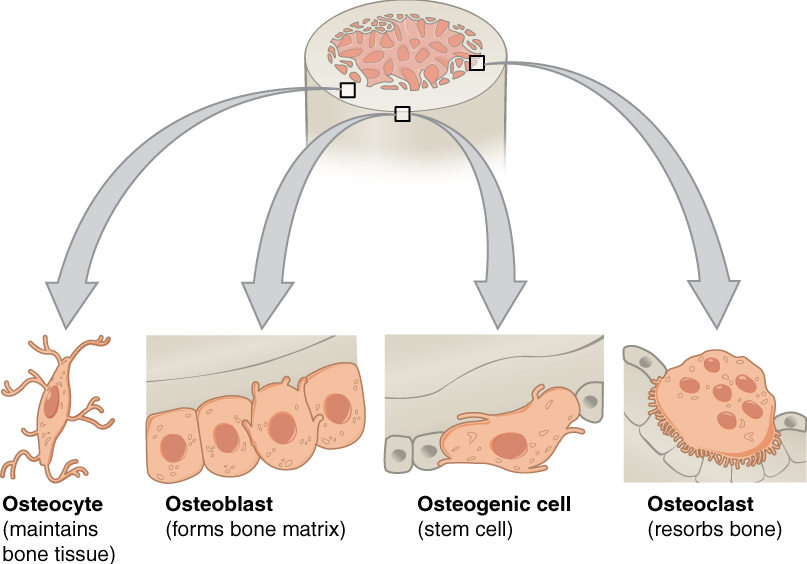
If osteoblasts and osteocytes are incapable of mitosis, then how are they replenished when old ones die? The answer lies in the properties of a third category of bone cells—the osteogenic cell. These cells are undifferentiated with high mitotic activity; and they are the only bone cells that divide. Immature osteogenic cells are found in the deep layers of the periosteum and the marrow. They differentiate and develop into osteoblasts.
The dynamic nature of bone means that new tissue is constantly formed, and old, injured, or unnecessary bone is dissolved for repair or for calcium release. The cell responsible for bone resorption, or breakdown, is the osteoclast. They are found on bone surfaces, are multinucleated, and originate from monocytes and macrophages, two types of white blood cells, rather than from osteogenic cells. Osteoclasts are continually breaking down old bone, while osteoblasts are continually forming new bone. The ongoing balance between osteoblasts and osteoclasts is responsible for the constant but subtle reshaping of bone. Table 10.2 reviews the bone cells, their functions, and locations.
| Cell type | Function | Location |
|---|---|---|
| Osteogenic cells | Develop into osteoblasts | Deep layers of the periosteum and the marrow |
| Osteoblasts | Bone formation | Growing portions of bone, including periosteum and endosteum |
| Osteocytes | Maintain mineral concentration of matrix | Entrapped in matrix (in lacunae) |
| Osteoclasts | Bone resorption | Bone surfaces and at sites of old, injured, or unneeded bone |
Compact and Spongy Bone
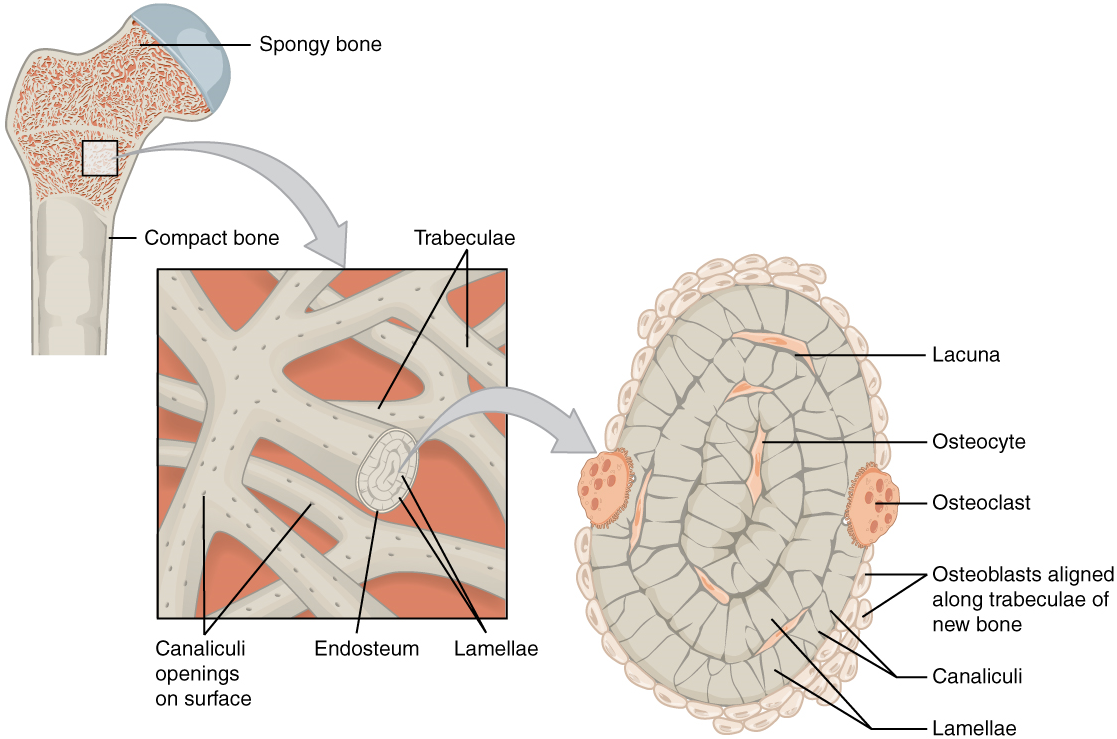
The differences between compact and spongy bone are best explored via their histology. Most bones contain compact and spongy osseous tissue, but their distribution and concentration vary based on the bone’s overall function. Compact bone is dense so that it can withstand compressive forces, while spongy (cancellous) bone has open spaces and supports shifts in weight distribution.
1. Compact Bone: Compact bone is the denser, stronger of the two types of bone tissue (Figure 10.9). It can be found deep to the periosteum and in the diaphyses of long bones, where it provides support and protection.
The microscopic structural unit of compact bone is called an osteon, or Haversian system. Each osteon is composed of concentric rings of calcified matrix called lamellae (singular = lamella). Running down the center of each osteon is the central canal, or Haversian canal, which contains blood vessels, nerves, and lymphatic vessels. These vessels and nerves branch off at right angles through a perforating canal, also known as Volkmann’s canals, to extend to the periosteum and endosteum.
The osteocytes are located inside spaces called lacunae (singular = lacuna), found at the borders of adjacent lamellae. As described earlier, canaliculi connect with the canaliculi of other lacunae and eventually with the central canal. This system allows nutrients to be transported to the osteocytes and wastes to be removed from them.
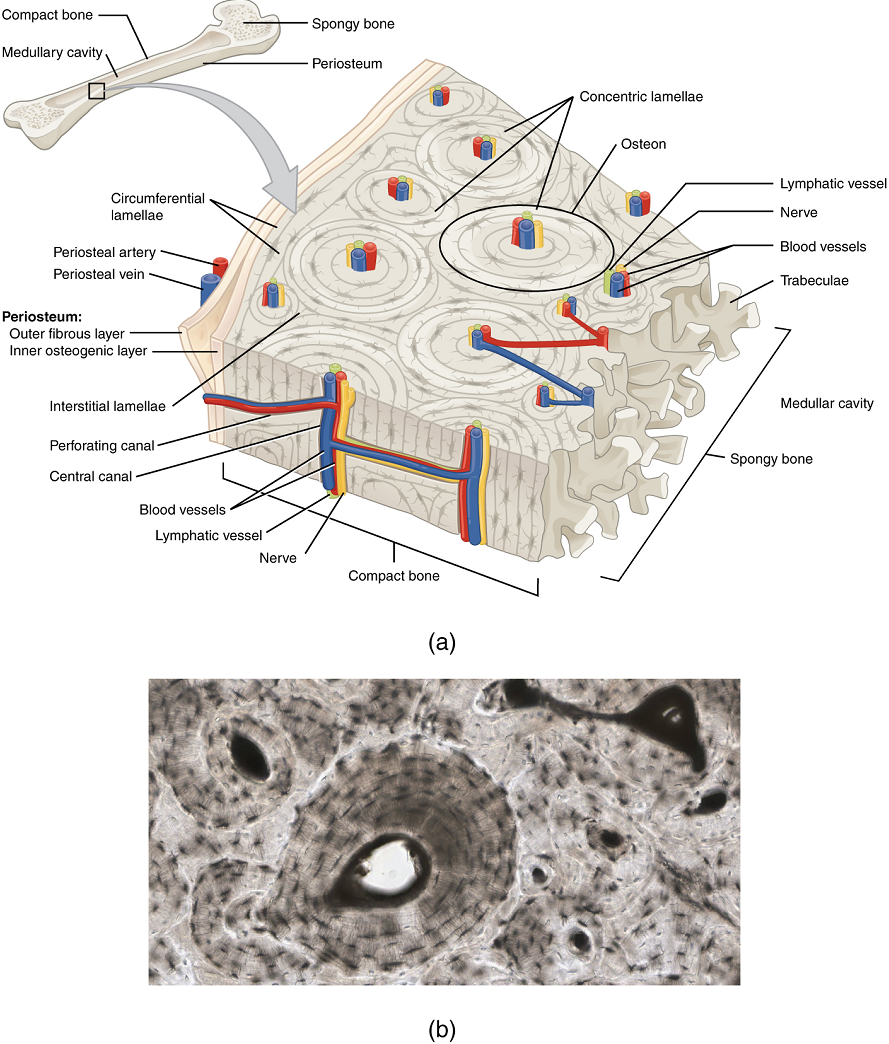
2. Spongy (Cancellous) Bone: Like compact bone, spongy bone, also known as cancellous bone, contains osteocytes housed in lacunae, but they are not arranged in concentric circles. Instead, the lacunae and osteocytes are found in a lattice-like network of matrix spikes called trabeculae (singular = trabecula; Figure 10.10). The trabeculae may appear to be a random network, but each trabecula forms along lines of stress to provide strength to the bone. The spaces of the trabeculated network provide balance to the dense and heavy compact bone by making bones lighter so that muscles can move them more easily. In addition, the spaces in some spongy bones contain red marrow, protected by the trabeculae, where hematopoiesis occurs.
Blood and Nerve Supply
The spongy bone and medullary cavity receive nourishment from arteries that pass through the compact bone. The arteries enter through the nutrient foramen (plural = foramina), a small opening in the diaphysis (Figure 10.11). The osteocytes in spongy bone are nourished by blood vessels of the periosteum that penetrate spongy bone and blood that circulates in the marrow cavities. As the blood passes through the marrow cavities, it is collected by veins, which then pass out of the bone through the foramen.
In addition to the blood vessels, nerves follow the same paths into the bone where they tend to concentrate in the more metabolically active regions of the bone. The nerves sense pain, and it appears they also play roles in regulating blood supplies and in bone growth, hence their concentrations in metabolically active sites of the bone.
Test Your Knowledge
I. Describe the structure and histology of the skeletal system.
- Based on previously covered material and the information in this unit, describe each of the different cell types found in cartilage and bone. For each cell type, identify:
- Where in the body, and from which type of cell, it arose.
- Where it normally resides in the body, as specifically as possible.
- What its main function is, and how (briefly) it serves that function.
- What happens to the cell if the matrix that surrounds it calcifies.
- Compare and contrast the components of cartilage matrix and bone matrix, explaining the differences in the physical characteristics of cartilage and bone.
- From what tissue type do bones and cartilage arise during early development? What other mature tissues arise from the same fetal tissue type?
II. Define and identify the following parts of a long bone: diaphysis, epiphysis, metaphysis, articular cartilage, periosteum, medullary cavity, and endosteum.
- Identify a typical long bone, showing the main external and internal features and identifying all the main tissue types found in a long bone.
III. Compare the composition and function of compact bone versus spongy bone.
- Compare and contrast compact bone and spongy bone, in terms of the following characteristics:
- The tissue type and cell type found in each type of bone.
- The arrangement of tissue and/or cells in each type of bone.
- The location of each within a bone.
- The function of each type of bone.
Part 4: Bone Formation and Development
In the early stages of embryonic development, the embryo’s skeleton consists of fibrous membranes and hyaline cartilage. By the sixth or seventh week of embryonic life, the actual process of bone development, ossification (osteogenesis), begins. There are two osteogenic pathways—intramembranous ossification and endochondral ossification—but bone is the same regardless of the pathway that produces it.
Cartilage Templates
Bone is a replacement tissue; that is, it uses a model tissue on which to lay down its mineral matrix. For skeletal development, the most common template is cartilage. During fetal development, a framework is laid down that determines where bones will form. This framework is a flexible, semi-solid cartilage matrix produced by chondroblasts. As the matrix surrounds and isolates chondroblasts, they mature into cells called chondrocytes. Unlike most connective tissues, cartilage is avascular, meaning that it has no blood vessels supplying nutrients and removing metabolic wastes. All of these functions are carried on by diffusion through the matrix. This is why damaged cartilage does not repair itself as readily as most tissues do.
Throughout fetal development and into childhood growth and development, bone forms on the cartilaginous matrix. By the time a fetus is born, most of the cartilage has been replaced with bone. Some additional cartilage will be replaced throughout childhood, and some cartilage remains in the adult skeleton.
Intramembranous Ossification
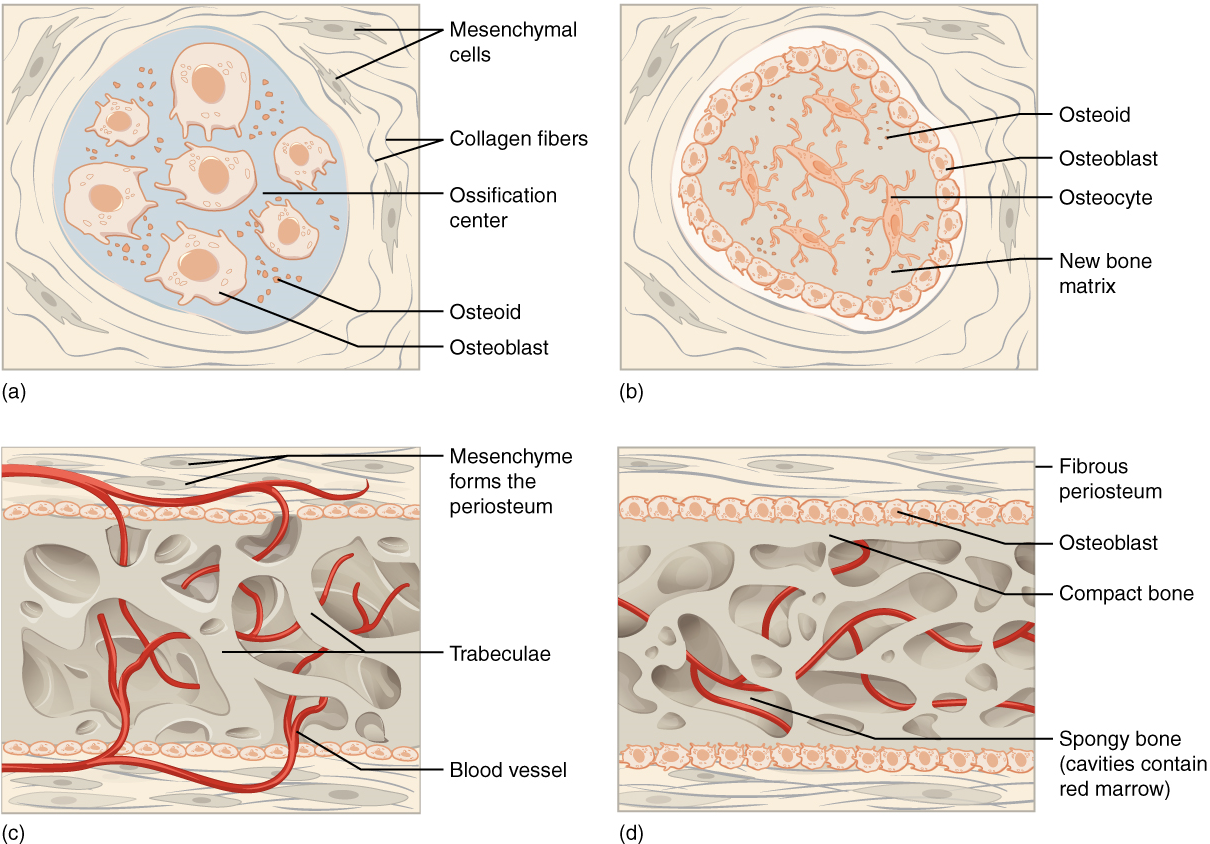
During intramembranous ossification, compact and spongy bone develops directly from sheets of mesenchymal (undifferentiated) connective tissue. The flat bones of the face, most of the cranial bones, and the clavicles (collarbones) are initially formed via intramembranous ossification.
The process begins when mesenchymal cells in the embryonic skeleton gather together and begin to differentiate into specialized cells (Figure 10.12a). Some of these cells will form capillaries, while others will become osteogenic cells and then osteoblasts. Although they will ultimately be spread out by the formation of bone tissue, early osteoblasts appear in a cluster called an ossification center.
The osteoblasts secrete osteoid, uncalcified matrix, which calcifies (hardens) within a few days as mineral salts are deposited on it, thereby entrapping the osteoblasts within. Once entrapped, the osteoblasts become osteocytes (Figure 10.12b). As osteoblasts transform into osteocytes, osteogenic cells in the surrounding connective tissue differentiate into new osteoblasts.
Osteoid (unmineralized bone matrix) secreted around the capillaries results in a trabecular matrix, while osteoblasts on the surface of the spongy bone become the periosteum (Figure 10.12c). The periosteum then creates a protective layer of compact bone superficial to the trabecular bone. The trabecular bone crowds nearby blood vessels, which eventually condense into red marrow (Figure 10.12d).
Intramembranous ossification begins in utero during fetal development and continues on into adolescence. At birth, the skeleton is not fully ossified. Most joints of the skull, for example, are more mobile in an infant than in an adult to allow the skull to deform during passage through the birth canal. The flat bones of the cranium continue to grow throughout childhood, ultimately being separated by narrow immobile joints called sutures. Each clavicle also initially (at about six weeks of embryonic age) forms by intramembranous ossification from two primary ossification centers that fuse together in utero to form a single bone with cartilage at both ends. This cartilage later ossifies to form the mature clavicles with articular cartilage on either end (usually in an individual’s early twenties). The last bones to ossify via intramembranous ossification are the flat bones of the face, which reach their adult size at the end of the adolescent growth spurt. The mandible in an infant, for example, consists of two separate bones (left and right), connected by a joint called a symphysis. This mandibular symphysis is fully ossified within the first year of life, permanently fusing the left and right bones to form the mandible.
Endochondral Ossification
In endochondral ossification, bone develops by replacing hyaline cartilage. Cartilage does not become bone but instead serves as a template to be completely replaced by new bone. Endochondral ossification takes much longer than intramembranous ossification. Bones at the base of the skull and long bones form via endochondral ossification.
In a long bone, for example, at about six to eight weeks after conception, some of the mesenchymal cells differentiate into chondroblasts (cells that secrete the organic components of cartilage matrix) that form the cartilaginous skeletal precursor of the bones (Figure 10.13a). Soon after, the perichondrium, a membrane that covers the cartilage, appears (Figure 10.13b).
As more matrix is produced, the chondrocytes in the center of the cartilaginous model grow in size. As the matrix calcifies, nutrients can no longer reach the chondrocytes. This results in their death and the disintegration of the surrounding cartilage. Blood vessels invade the resulting spaces, not only enlarging the cavities but also carrying osteogenic cells with them, many of which will become osteoblasts (Figure 10.13c). These enlarging spaces eventually combine to become the medullary cavity (Figure 10.13d).
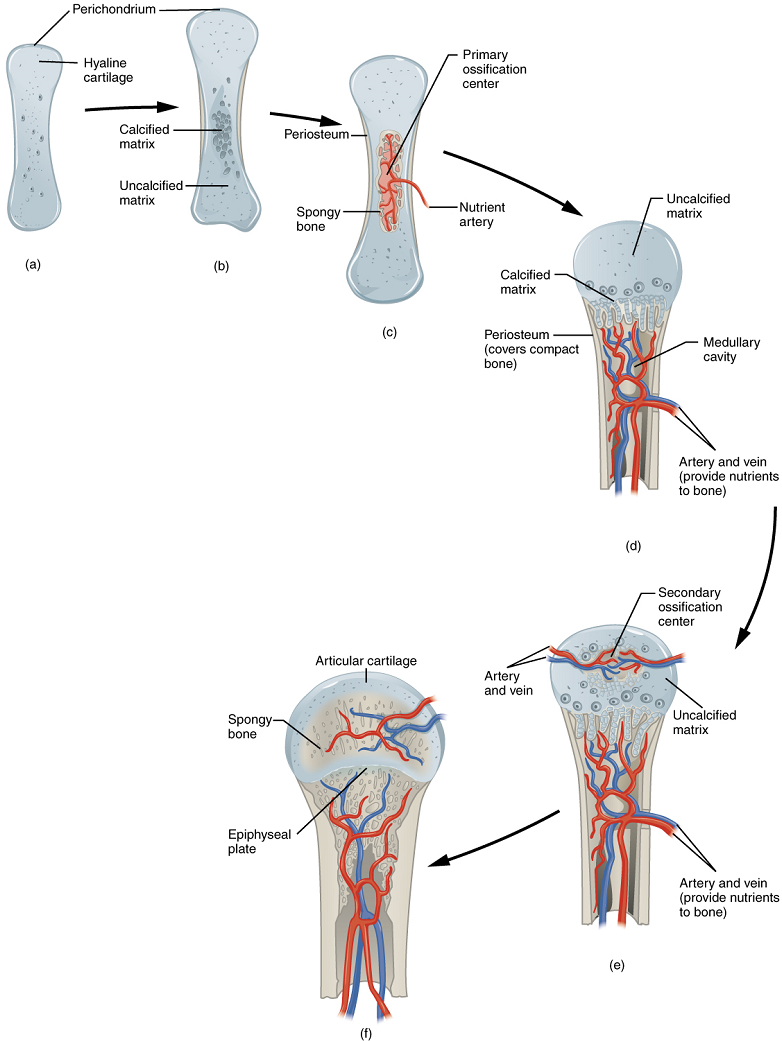
As the cartilage grows, capillaries penetrate it. This penetration initiates the transformation of the perichondrium into the bone-producing periosteum. Here, the osteoblasts form a periosteal collar of compact bone around the cartilage of the diaphysis. By the second or third month of fetal life, bone cell development and ossification ramps up and creates the primary ossification center, a region deep in the periosteal collar where ossification begins (Figure 10.13c).
While these deep changes are occurring, chondrocytes and cartilage continue to grow at the ends of the bone (the future epiphyses), which increases the bone’s length at the same time bone is replacing cartilage in the diaphyses. By the time the fetal skeleton is fully formed, cartilage only remains at the joint surface as articular cartilage and between the diaphysis and epiphysis as the epiphyseal plate, the latter of which is responsible for the longitudinal growth of bones (Figure 10.13f). After birth, this same sequence of events (matrix mineralization, death of chondrocytes, invasion of blood vessels from the periosteum, and seeding with osteogenic cells that become osteoblasts) occurs in the epiphyseal regions, and each of these centers of activity is referred to as a secondary ossification center (Figure 10.13e).
How Bones Grow in Length
The epiphyseal plate is the area of growth in a long bone. It is a layer of hyaline cartilage where ossification occurs in immature bones. On the epiphyseal side of the epiphyseal plate, cartilage is formed. On the diaphyseal side, cartilage is ossified, and the diaphysis grows in length. The epiphyseal plate is composed of four zones of cells and activity (Figure 10.14). The reserve zone is the region closest to the epiphyseal end of the plate and contains small chondrocytes within the matrix. These chondrocytes do not participate in bone growth but secure the epiphyseal plate to the osseous tissue of the epiphysis.
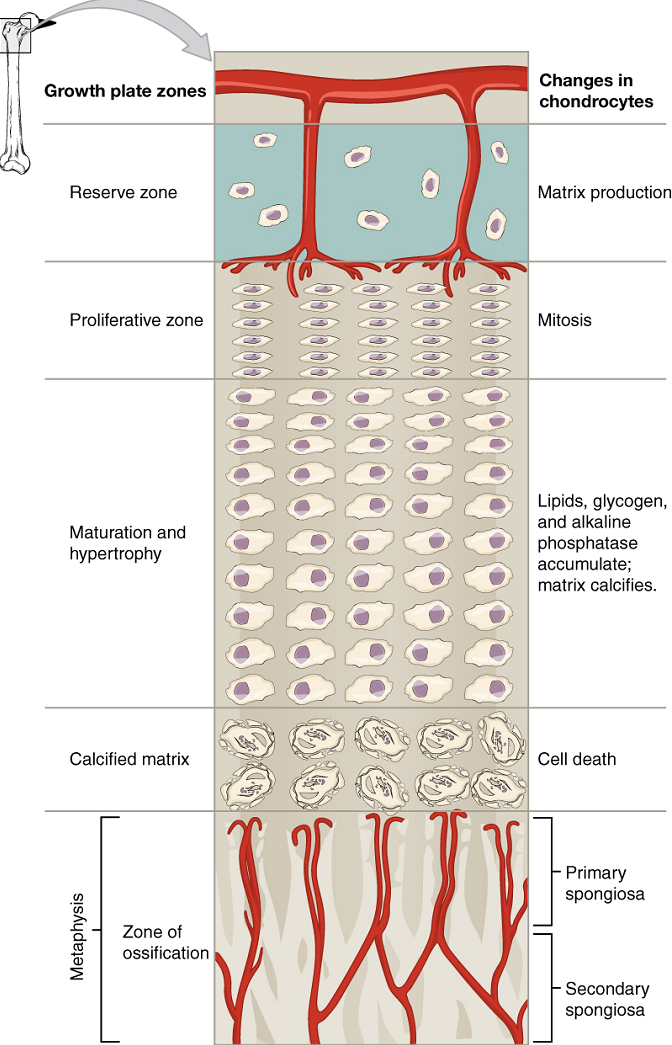
The proliferative zone is the next layer toward the diaphysis and contains stacks of slightly larger chondrocytes. It makes new chondrocytes (via mitosis) to replace those that die at the diaphyseal end of the plate. Chondrocytes in the next layer, the zone of maturation and hypertrophy, are older and larger than those in the proliferative zone. The more mature cells are situated closer to the diaphyseal end of the plate. The longitudinal growth of bone is a result of cellular division in the proliferative zone and the maturation of cells in the zone of maturation and hypertrophy.
Most of the chondrocytes in the zone of calcified matrix, the zone closest to the diaphysis, are dead because the matrix around them has calcified. Capillaries and osteoblasts from the diaphysis penetrate this zone, and the osteoblasts secrete bone tissue on the remaining calcified cartilage.
Thus, the zone of calcified matrix connects the epiphyseal plate to the diaphysis. A bone grows in length when osseous tissue is added to the diaphysis.
Bones continue to grow in length until early adulthood. The rate of growth is controlled by hormones, which will be discussed later. When the chondrocytes in the epiphyseal plate cease their proliferation and bone replaces the cartilage, longitudinal growth stops. All that remains of the epiphyseal plate is the now fully ossified epiphyseal line (Figure 10.15).
How Bones Grow in Diameter
While bones are increasing in length, they are also increasing in diameter; growth in diameter can continue even after longitudinal growth ceases. This is called appositional growth. Osteoclasts resorb old bone that lines the medullary cavity, while osteoblasts, via intramembranous ossification, produce new bone tissue beneath the periosteum. The erosion of old bone along the medullary cavity and the deposition of new bone beneath the periosteum not only increase the diameter of the diaphysis but also increase the diameter of the medullary cavity. This process is called modeling.
Bone Remodeling
The process in which matrix is resorbed on one surface of a bone and deposited on another is known as bone modeling. Modeling primarily takes place during a bone’s growth. However, in adult life, bone undergoes remodeling, in which resorption of old or damaged bone takes place on the same surface where osteoblasts lay new bone to replace that which is resorbed. Injury, exercise, and other activities lead to remodeling. Those influences are discussed later in the unit, but even without injury or exercise, about 5% to 10% of the skeleton is remodeled annually just by destroying old bone and renewing it with fresh bone.
Test Your Knowledge
I. Define ossification, compare intramembranous ossification with endochondral ossification, describe how a long bone grows in length and width, and specify how various factors might affect the rate of ossification and, by extension, the height of a mature individual.
II. Explain in detail the processes of:
- Intramembranous ossification
- Endochondral ossification
- Growth in length of a long bone
- Growth in width of a long bone
III. Compare and contrst the process of
- intramembranous ossification and endochondral ossification.
- endochondral ossification and lengthwise growth of a long bone.
- intramembranous ossification and widthwise growth of a long bone.
IV. The height of an individual is largely determined by the rate of ossification prior to physical maturity. Briefly explain why this is so.
Part 5: Fractures
A fracture is a broken bone. It will heal whether or not a physician resets it in its anatomical position. If the bone is not reset correctly, the healing process will keep the bone in its deformed position.
Types of Fractures: Fractures are classified by their complexity, location, and other features (Figure 10.16). Table 10.3 outlines common types of fractures. Some fractures may be described using more than one term because it may have the features of more than one type (e.g., an open transverse fracture). Of the types pictured in Figure 10.16 and Table 10.3, you are only required to understand the details of closed, open, comminuted, and greenstick fractures.
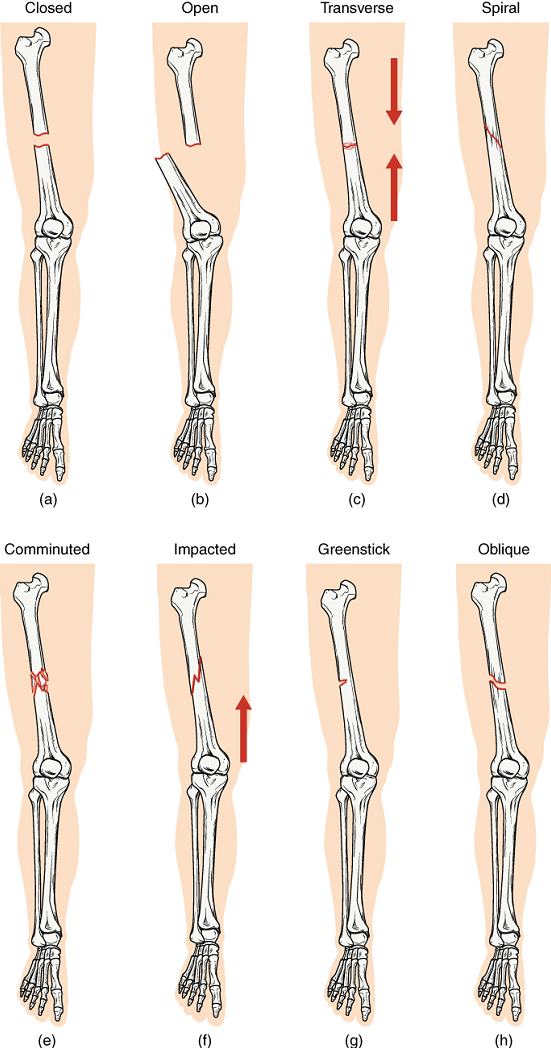
| Type of fracture | Description |
|---|---|
| Transverse | Occurs straight across the long axis of the bone |
| Oblique | Occurs at an angle that is not 90 degrees |
| Spiral | Bone segments are pulled apart as a result of a twisting motion |
| Comminuted | Several breaks result in many small pieces between two large segments |
| Impacted | One fragment is driven into the other (usually a result of compression) |
| Greenstick | A partial fracture in which only one side of the bone is broken |
| Open (compound) | A fracture in which at least one end of the broken bone tears through the skin; carries a high risk of infection |
| Closed (simple) | A fracture in which the skin remains intact |
Test Your Knowledge
I. Compare and contrast the common causes and appearance of:
- Closed (simple) vs. open (compound) fractures
- Comminuted vs. closed fractures
- Greenstick vs. closed fractures
- Comminuted vs. greenstick fractures
II. Can a fracture be classified as two of the above types at the same time? In other words, are any of the following fracture types possible? In each case, explain why or why not.
- A closed open fracture
- A closed comminuted fracture
- A closed greenstick fracture
- An open comminuted fracture
- An open greenstick fracture
Mouth
Back of the knee.
Thumb
Mouth
Back of the knee.
Knee cap.
Fluid or semi-fluid portion of the matrix.
Lowest part of the vertebral column; 'tailbone'
Specialized areolar tissue rich in stored fat.
Knee cap.
(Also, hematopoiesis) production of the formed elements of blood.
(Also, thrombocytes) one of the formed elements of blood that consists of cell fragments broken off from megakaryocytes.
See parasagittal plane
See frontal plane
See parasagittal plane
Thigh bone; the single bone of the thigh.
Abdominopelvic region (left or right) located under the lowest ribs in the superior corners of the abdominopelvic cavity.
Abdominopelvic region (left or right) located under the lowest ribs in the superior corners of the abdominopelvic cavity.
See frontal plane
Lowest part of the vertebral column; 'tailbone'
Abdominopelvic region located in the central superior area below the xiphoid process.
Abdominopelvic region located in the central superior area below the xiphoid process.
Left or right central abdominopelvic region.
Central abdominopelvic region including the belly button.
Left or right central abdominopelvic region.
Central abdominopelvic region including the belly button.
Abdominopelvic region in the left or right inferior corners of the abdomen, below the hip bone.
Abdominopelvic region in the left or right inferior corners of the abdomen, below the hip bone.
Central inferior abdominopelvic region.
(Also, cancellous bone) trabeculated osseous tissue that supports shifts in weight distribution.
Central inferior abdominopelvic region.
Most common type of cartilage, smooth and made of short collagen fibers embedded in a chondroitin sulfate ground substance.
Portion of the large intestine.
Portion of the large intestine.
Beginning of the large intestine, forming a small pouch.
Beginning of the large intestine, forming a small pouch.
Membrane that covers organs and reduces friction; also referred to as serosa.
The most abundant of three protein fibres found in the extracellular matrix of connective tissues.
A form of calcium phosphate mineral found in bones (also hydroxylapatite).
Membrane that covers organs and reduces friction; also referred to as serosa.
Primary cell in mature bone; responsible for maintaining the matrix.
(Plural = lacunae) small spaces in bone or cartilage tissue that cells occupy.
Facing the body wall.
Two-dimensional, horizontal plane that divides the body or organ into superior and inferior portions.
Facing the organs (opposite of parietal).
Facing the body wall.
Facing the organs (opposite of parietal).
Ameboid (irregular outline with peripheral projections) phagocyte found in several tissues throughout the body.
Serous membrane that lines the pleural cavity and covers the lungs.
Serous membrane that lines the abdominopelvic cavity and covers the organs found there.
Serous membrane that lines the pleural cavity and covers the lungs.
Serous membrane that lines the abdominopelvic cavity and covers the organs found there.
See serous membrane
(In physiology) ideal value for a physiological parameter; the level or small range within which a physiological parameter such as blood pressure is stable and optimally healthful, that is, within its parameters of homeostasis.
(In physiology) ideal value for a physiological parameter; the level or small range within which a physiological parameter such as blood pressure is stable and optimally healthful, that is, within its parameters of homeostasis.
Homeostatic mechanism that tends to stabilize an upset in the body’s physiological condition by preventing an excessive response to a stimulus, typically as the stimulus is removed.
Region of the brain inferior to the thalamus that functions in neural and endocrine signaling, temperature regulation, and control of the autonomic nervous system.
Compares values to their normal range; deviations cause the activation of an effector.
Lacking blood vessels.
Embryonic tissue from which connective tissue cells derive.
Homeostatic mechanism that tends to stabilize an upset in the body’s physiological condition by preventing an excessive response to a stimulus, typically as the stimulus is removed.
Organ that can cause a change in a value.
Organ that can cause a change in a value.
Region of the brain inferior to the thalamus that functions in neural and endocrine signaling, temperature regulation, and control of the autonomic nervous system.
Middle region of the adult brain that develops from the mesencephalon.
Layer of dense irregular connective tissue surrounding cartilage.
cartilage cells
Mechanism that intensifies a change in the body’s physiological condition in response to a stimulus.
Mechanism that intensifies a change in the body’s physiological condition in response to a stimulus.
Also called urination or voiding.
Also called urination or voiding.
In neurons, that portion of the cell that contains the nucleus; the cell body, as opposed to the cell processes (axons and dendrites).
(In connective tissue) extracellular material that is produced by the cells embedded in it, containing ground substance and fibers.

