3 Chapter Three: Anatomy and Physiology for Intravenous Therapy
Learning Objectives
- Identify anatomical and physiological principles related to intravenous therapy.
- Identify and describe the structure and function of the heart.
- Identify and describe the major components of the vascular system, including veins, arteries, and capillaries.
- Describe how the circulatory system functions to transport fluids, nutrients, and waste products and the principles of blood pressure.
- Identify common anatomical sites for peripheral intravenous access (e.g., cephalic, basilic, median cubital veins).
- Identify common anatomical sites for central intravenous access.
- Identify how anatomical and physiological differences between pediatric, adult, and geriatric patients affect IV therapy (e.g., vein fragility, fluid requirements)
Nursing in Louisiana
Type your examples here.
- First
- Second
Introduction
An understanding of anatomy and physiology is critical for the safe and effective practice of IV therapy. IV therapy is considered invasive, requiring adequate knowledge of both external and internal body structures. Injury may result from improper techniques or a lack of necessary knowledge. The structure and function of the circulatory system is a key component of IV therapy. The role of the heart and the effects of IV therapy on cardiac output must be considered, along with the impact of IV drugs on target organs. The significance of understanding blood circulation plays a role in catheter insertion and maintenance as well as medication and fluid distribution. Identifying key anatomical sites for peripheral and central venous access assists in successful access. By understanding the body’s immune and inflammatory responses to IV therapy, as well as age-related changes affecting IV therapy in pediatric and elderly patients, healthcare professionals can better prevent complications and ensure optimal outcomes for their patients. Mastery of these principles enables clinicians to tailor IV therapy appropriately and deliver patient-centered care.
The Circulatory System – The Heart
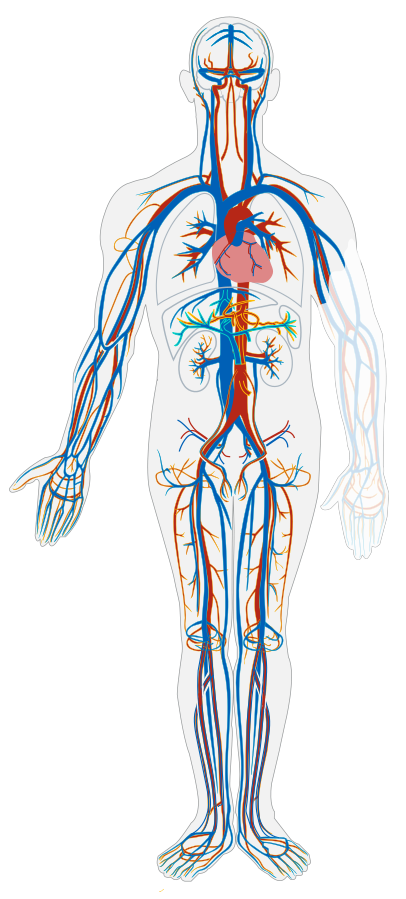
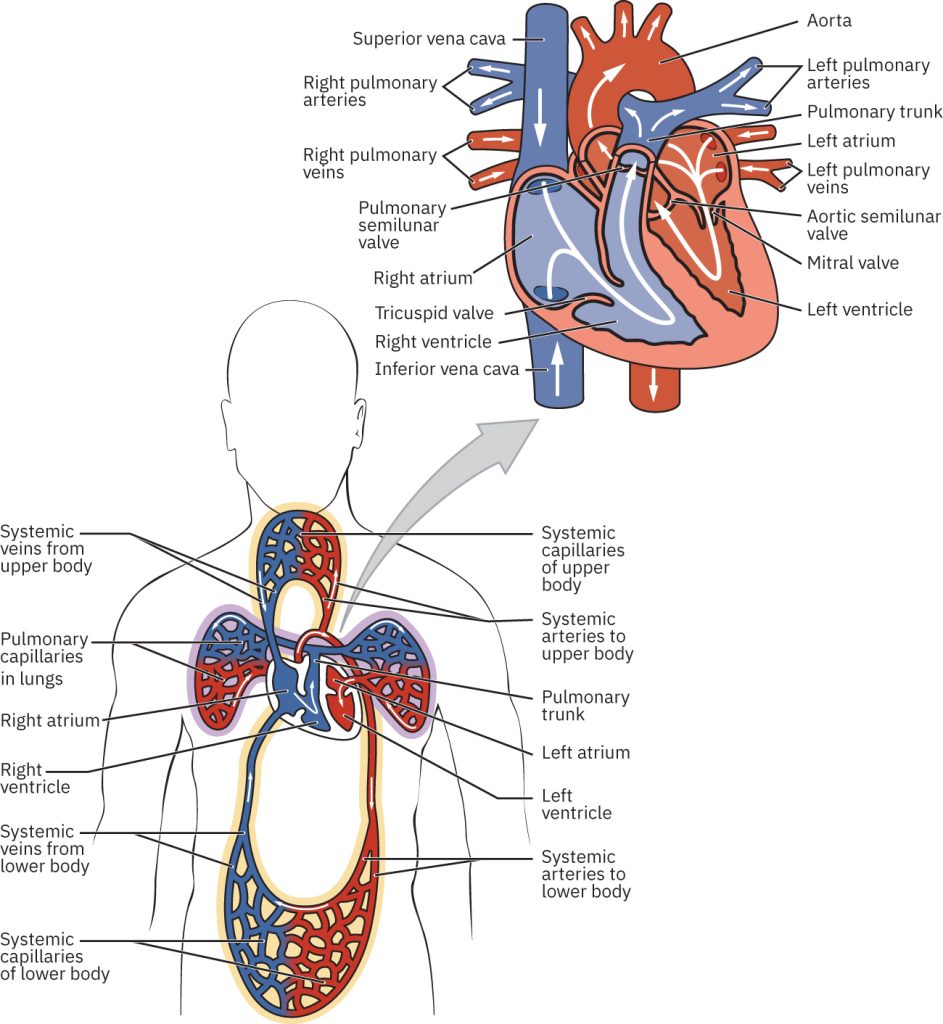
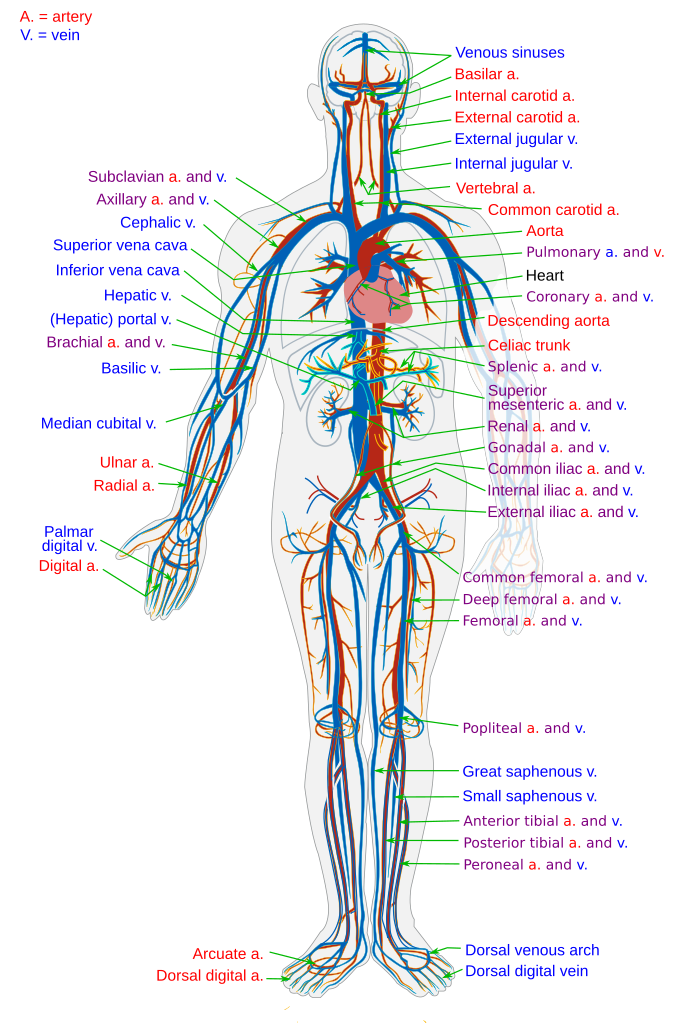
The circulatory system, or cardiovascular system, is composed of three main components: the heart, blood vessels, and blood (Figure 3.1). Each plays a crucial role in maintaining the body's homeostasis by transporting oxygen, nutrients, hormones, and waste products. The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum. The great veins, the superior and inferior venae cavae, and the great arteries, the aorta and pulmonary trunk, are attached to the superior surface of the heart. The heart serves as the central pump of the cardiovascular system, ensuring continuous blood flow throughout the body. It is divided into four chambers, two atria and two ventricles, that work together to pump oxygenated blood to the body and deoxygenated blood to the lungs. The rhythmic contraction and relaxation of the heart creates the pressure necessary to propel blood through the vessels.
Although primarily controlled by the autonomic nervous system, the heart rate can also be influenced by chemical, emotional, or electrical stimuli. Cardiac output refers to the total volume of blood the heart pumps per minute and is a measure of the heart's efficiency and overall cardiovascular health. Since this output is determined by multiplying heart rate by the stroke volume (amount of blood volume ejected by the left ventricle with each contraction), IV therapy is deeply interconnected. Medications and fluids can be used to alter both heart rate and blood volume. Understanding cardiac output is particularly important in clinical settings, as it helps evaluate and guide treatments. Healthcare professionals must aim to maintain effective blood circulation and overall homeostasis.
The Circulatory System – The Blood
Blood is the fluid component that carries essential substances throughout the body. It consists of plasma, red blood cells, white blood cells, and platelets. Plasma is the liquid portion that contains water, electrolytes, and proteins, serving as a transport medium for nutrients, hormones, and waste. Red blood cells are responsible for transporting oxygen from the lungs to tissues and returning carbon dioxide for exhalation. White blood cells play a vital role in the immune response, defending the body against pathogens, while platelets are essential for blood clotting and wound healing. Together, these components ensure the circulatory system supports the body's vital functions. The amount of fluid within the blood vessels, or intravascular volume, contributes to blood pressure as measured by pressure within the arteries. Other organs may contribute waste products from metabolic functions into the bloodstream to be transported for further metabolism, and ultimately for some waste excretion from the body. An example is water entering the body through oral intake, absorption through the gastrointestinal tract, delivery to cells in need of fluid, and excess being delivered to the renal system for processing and urinary excretion.
The Circulatory System – The Blood Vessels
After blood is pumped out of the ventricles, it is carried through the body via blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels and eventually into tiny capillaries where nutrients and wastes are exchanged at the cellular level. Capillaries combine with other small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart. Compared to arteries, veins are thin-walled, low-pressure vessels. Larger veins are also equipped with a valve that promotes the unidirectional flow of blood toward the heart and prevents backflow caused by the inherent low blood pressure in veins as well as the pull of gravity. Blood vessels form an extensive network throughout the body, enabling the circulation of blood to every tissue. Blood flows through the lumen, or hollow space within these vessels. It is within the lumen of a vein that an IV catheter is inserted. (Figure 3.2)
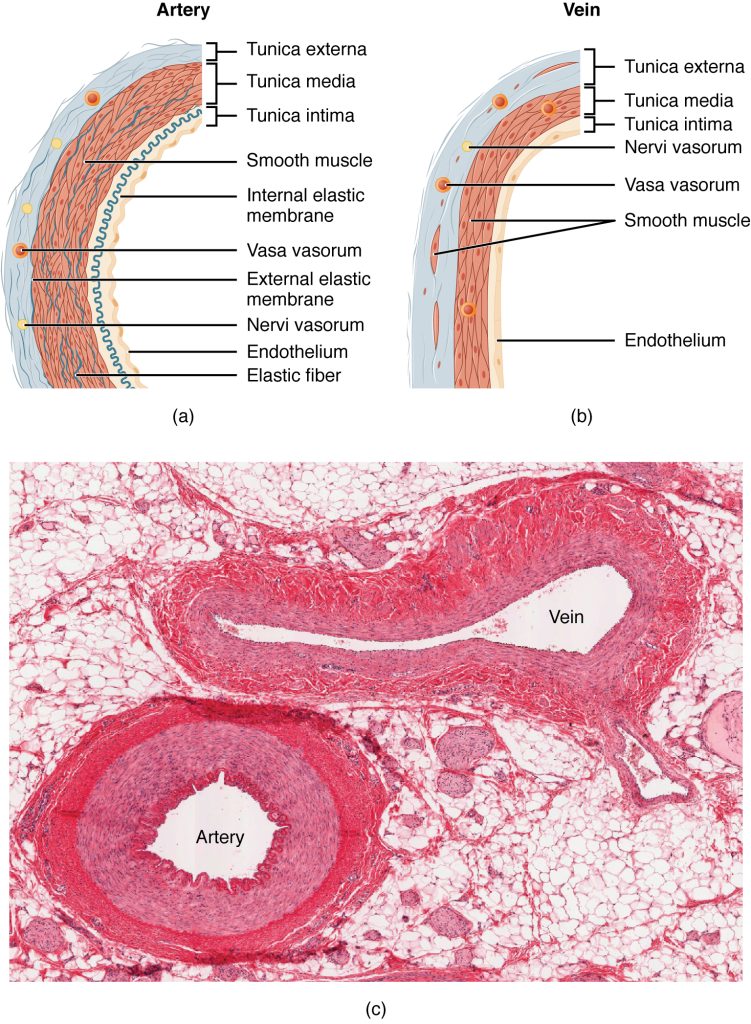
Arteries
Arteries carry oxygen-rich blood away from the heart to the body's organs and tissues. They have thick, elastic walls composed of three layers: the tunica intima, tunica media, and tunica adventitia. (Figure 3.2) These walls allow arteries to withstand and maintain the high pressure generated by the heart’s pumping action. The elasticity and structure of these vessels ensure efficient blood flow and pressure regulation.
Safety note:
Arteries are never used for IV insertion. Arteries will have a palpable pulse and are located deeper within the tissue than veins.
Capillaries
Capillaries are microscopic vessels that connect arteries and veins, facilitating the exchange of oxygen, nutrients, and waste products between blood and tissues. Arteries transition in smaller vessels called arterioles through which blood continues into the capillary bed. Returning circulation from the capillaries begins with venules before continuing into the venous system. Understanding their structure and function is essential for healthcare professionals administering IV therapy to ensure proper delivery of medications, fluids, or nutrients to the patient. While IV therapy does not directly access capillaries, the capillary network may be affected by rapid fluid infusions or if a complication of IV therapy has developed.
Veins
Veins transport oxygen-depleted blood back to the heart for reoxygenation in the lungs. Veins have thinner walls than arteries, as the blood pressure within them is significantly lower. (Figure 3.2) They also have a wider lumen, which allows for a greater volume of blood to flow at a slower rate. To prevent backflow, veins are equipped with valves, especially in the extremities, where blood must travel against gravity. (Figure 3.3) Unlike arteries, veins rely on the contraction of surrounding muscles to help propel blood toward the heart.
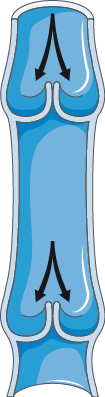
Veins closer to the surface of the skin, known as superficial veins, are more likely to be identifiable than deep veins, which are located further beneath the skin and muscle layers. The residual blood pressure and the amount of circulating volume determines the accessibility of superficial veins. In warm conditions, veins may dilate to help release heat from the body, making them appear more prominent. (Figure 3.4) In contrast, cold temperatures cause veins to constrict, making them less visible. Manipulating the natural venous function by changing position of an extremity to increase gravitational pull or by placing a tourniquet to interrupt flow can increase vein dilation at the surface level. IV therapy involves the use of both peripheral and centrally located veins. Insertion of an IV device should always follow the path of blood flowing toward the heart.

The superior vena cava is a large vein that is formed by the joining of the right and left brachiocephalic veins, which drain blood from the head, neck, arms, and upper chest. The superior vena cava is the endpoint for central venous catheters (CVCs) and peripherally inserted central catheters (PICCs). Its large diameter and high blood flow rate help dilute potentially irritating solutions and medications, reducing the risk of damage to the vein walls.
Table 3.1 Comparison of Arteries and Veins
| Arteries | Veins | |
|---|---|---|
| Direction of blood flow | Conducts blood away from the heart | Conducts blood toward the heart |
| General appearance | Rounded | Irregular, often collapsed |
| Pressure | High | Low |
| Wall thickness | Thick | Thin |
| Relative oxygen concentration | Higher in systemic arteries
Lower in pulmonary arteries |
Lower in systemic veins
Higher in pulmonary veins |
| Valves | Not present | Present most commonly in limbs and in veins inferior to the heart |
Table source: Table 20.1 Structure and Function of Blood Vessels. In Anatomy and Physiology 2e. OpenStax. Licensed CC-BY 4.0
Common Veins Used for Peripheral Venous Access
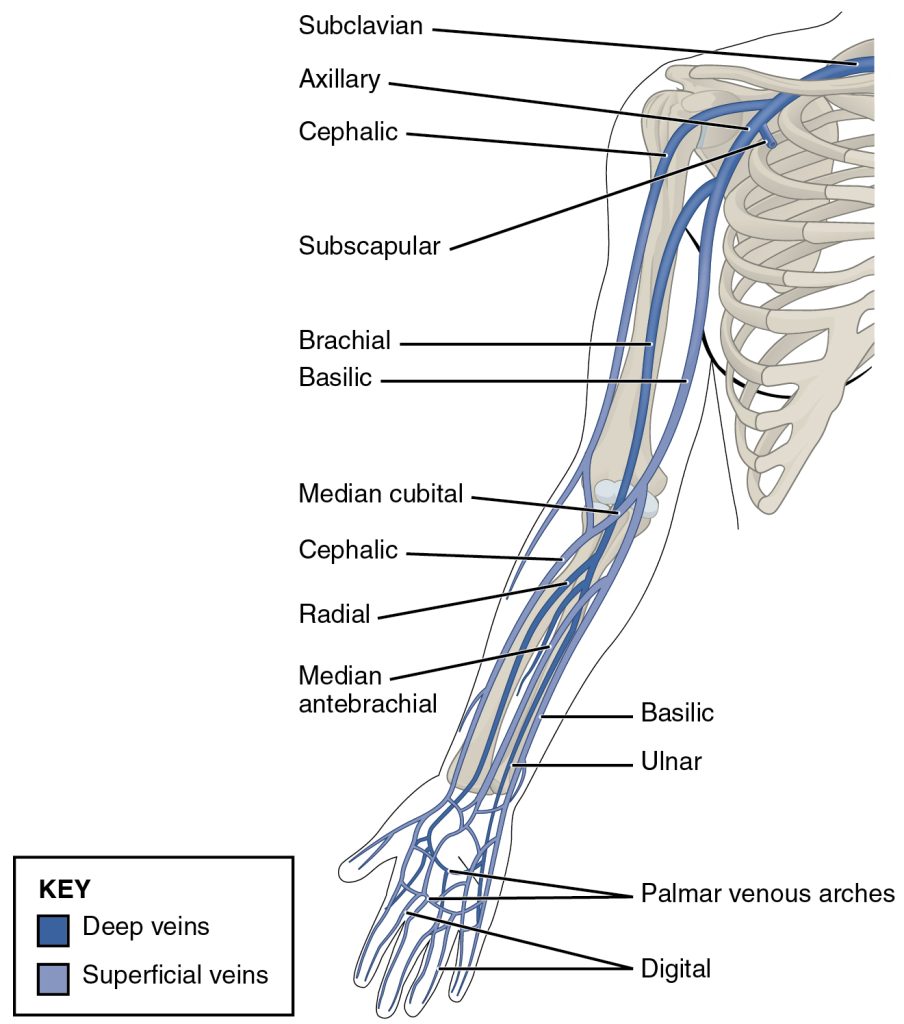
The metacarpal veins on the dorsal hand are frequently used for peripheral IV access due to their ease of accessibility. However, using these veins can sometimes limit wrist movement. They are typically selected for short-term therapy involving less irritating substances or smaller fluid volumes because they have a higher likelihood of failure. Despite these limitations, their ease of access makes them a preferred choice in many situations.
The accessory cephalic vein, which extends from the metacarpal vein of the thumb along the radial bone, is another commonly used vein. It is large, easily accessible, and can accommodate larger bore needles and higher fluid volumes. This vein generally allows for better mobility compared to others, although closer placement to the wrist can result in discomfort and restricted movement.
The antecubital veins, located in the antecubital fossa, include three distinct veins: the median cephalic on the radial side, the median basilic on the ulnar side, and the median cubital in the inner elbow. (Figure 3.6) These veins are large and frequently chosen for emergency IV access and blood draws. While they can be used routinely, their location in the elbow region restricts movement, which may compromise the integrity of the catheter over time.
The basilic (ulnar side) and cephalic (radial side) veins (Figure 3.6) in the upper arm are extensions of the forearm veins and are often selected for IV therapy. These veins are typically long and straight, making them suitable for stable catheter placement and reliable access.
Alternative sites are considered when clinical circumstances necessitate. Certain veins, such as the digital veins and wrist veins, are used only when other sites are unavailable due to their higher failure rates and the discomfort associated with insertion. The brachial vein in the upper arm, typically running alongside the brachial artery and the median nerve, is not commonly used for routine peripheral IV access due to its depth and proximity to these critical structures. It may be accessed under ultrasound guidance in specific clinical situations when more superficial veins are unavailable or unsuitable.
Similarly, veins in the dorsum of the foot are considered a last resort, especially for patients with conditions such as delayed wound healing, decreased peripheral sensation, or circulatory issues, including those caused by diabetes mellitus. In infants under six months of age, scalp veins may be used for IV access. These veins are fragile and require careful handling, making them suitable only for very young patients.
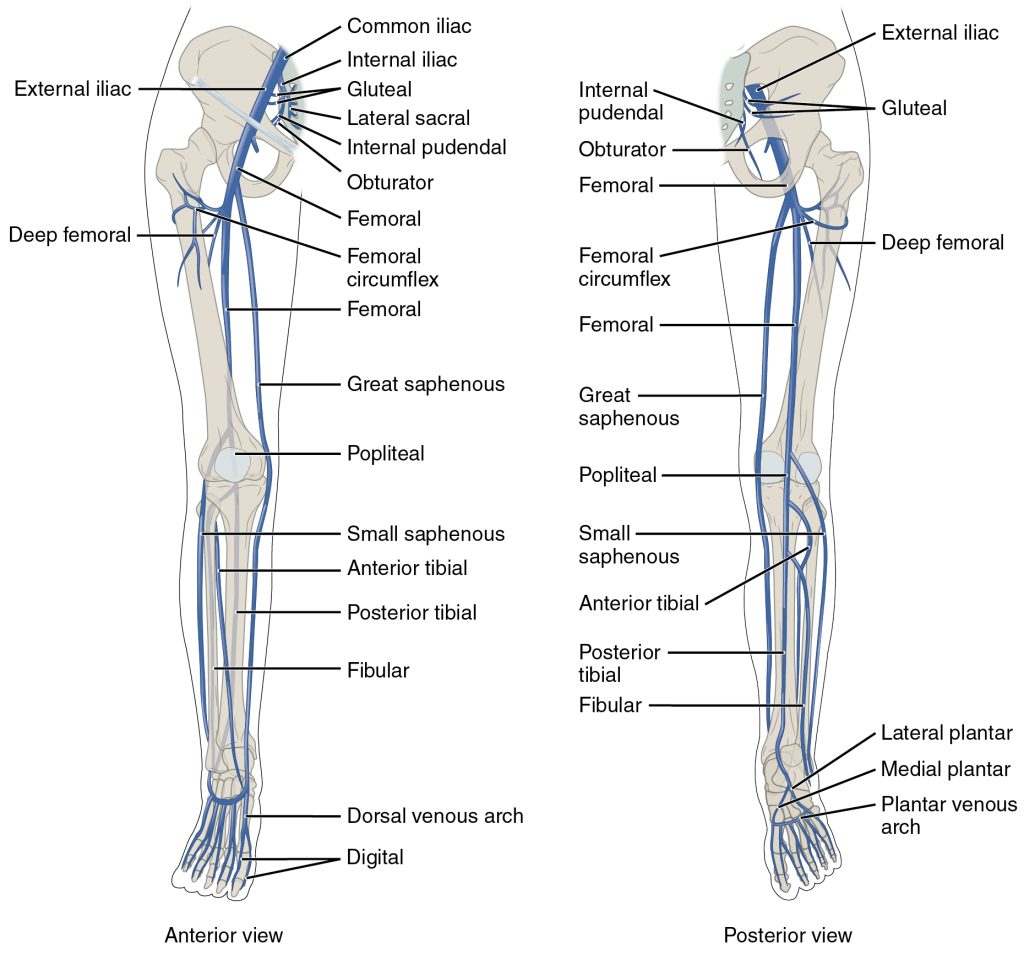
Common Veins Used for Central Venous Access
The external and internal jugular veins are located in the neck. The external jugular vein runs along the side of the neck, while the internal jugular vein lies deeper and closer to the carotid artery. Both veins are commonly used for central venous catheterization in IV therapy when peripheral access is difficult. The internal jugular vein is often preferred because it provides a straight path to the superior vena cava, allowing for efficient administration of fluids, medications, and monitoring of central venous pressure.
The subclavian vein is situated beneath the clavicle (collarbone), running alongside the subclavian artery. It is frequently accessed for central venous catheter placement in IV therapy, particularly for long-term use such as total parenteral nutrition or chemotherapy. This vein offers a relatively stable location with a low risk of infection compared to other sites, although there is a higher risk of complications like pneumothorax during insertion.
The femoral vein is located in the groin area, running alongside the femoral artery and nerve. It is often used for central venous access in emergency situations or when other access points are unavailable. While the femoral vein is easily accessible and allows for rapid catheterization, it carries a higher risk of infection and deep vein thrombosis due to its proximity to the groin and high movement area.
Due to the location of these veins, minimal activity restrictions are required as most access devices are sutured or otherwise adequately secured with a stabilization device.
Clinical Note:
Certain veins can be used for both peripheral and central access. The basilic vein is the vein most commonly used to insert a Peripherally Inserted Central Catheter (PICC) line. This vein is located in the upper arm and is preferred because it is large, superficial, and provides a direct path to the central circulation via the superior vena cava. Other veins, such as the cephalic vein or brachial veins, may also be used in this manner.
Inflammatory and Immune Response
The body’s immune response to IV catheterization involves several key mechanisms aimed at protecting the body from potential harm. The skin is the natural first-line of defense to pathogen entry. During IV therapy this barrier is compromised, leaving the body susceptible to infectious organisms. Another response is the formation of a thrombus, or blood clot, which can occur when the endothelial wall of a blood vessel is injured during the insertion or presence of an IV catheter. This process is part of the body’s natural defense mechanism to prevent excessive bleeding and seal the injury site. Additionally, mechanical friction caused by the IV catheter's movement within the vein can exacerbate the inflammatory response. This friction irritates the vessel walls, prompting the immune system to release inflammatory mediators.
Age-related Changes Affecting Intravenous Therapy
Age-related changes significantly influence the approach to intravenous therapy, requiring tailored considerations for pediatric and elderly patients to ensure safety and effectiveness.
Pediatric Patients
For children, the insertion of an IV line requires special care due to their reduced pain tolerance. The use of topical or local anesthetics prior to insertion can help minimize discomfort. Pediatric patients may not fully understand mobility limitations, which increases the likelihood of accidental dislodgement; therefore, splinting or protective devices may be necessary. Additionally, IV infusions for children must be calculated based on weight, with careful monitoring of infused volumes to prevent fluid overload, as their immature organ systems and higher water content relative to body surface area make them more vulnerable. Furthermore, their limited ability to communicate discomfort or complications necessitates frequent and thorough monitoring.
Elderly Patients

In older adults, IV therapy is increasingly common due to their higher rates of hospitalization and medical care needs. Age-related physiological changes, such as subcutaneous fat loss, dermal thinning, and decreased tissue elasticity, can make vein stabilization more challenging. Elderly veins may appear tortuous and are more fragile, increasing the risk of bruising, bleeding, or intolerance to irritating medications and solutions. Some elderly npatients may also experience vein sclerosis, which can complicate catheter insertion and advancement. Additional caution is required during procedures, such as applying a tourniquet, cleansing the site, or using adhesive tape, as aging skin is more prone to tearing. Preexisting conditions like cardiac or renal disease increase their risk of fluid overload and sensitivity to medication dosages. Finally, an age-related decline in immune response puts elderly patients at greater risk of complications, including infections.
Key Takeaways:
- IV therapy requires a thorough understanding of the circulatory system, including the structure and function of the heart, blood, and blood vessels.
- The heart’s role in maintaining cardiac output is directly linked to the effects of IV medications and fluids.
- Blood components, including plasma, red blood cells, white blood cells, and platelets, are critical to nutrient and oxygen transport, immune defense, and wound healing.
- Veins, with their thinner walls and valves, are essential for venous return and are the primary access points for IV therapy, unlike arteries.
- The most common veins for peripheral access include the metacarpal, basilic, and cephalic veins, while central access is typically achieved through the internal jugular, subclavian, or femoral veins.
- Age-related changes necessitate different approaches to IV therapy in pediatric and elderly patients to minimize complications.
- Understanding the immune and inflammatory responses to IV therapy helps mitigate risks such as infection, thrombosis, and vein irritation.
Review Questions
References
OpenStax. (2024). Anatomy and physiology 2e. OpenStax. https://openstax.org/books/anatomy-and-physiology-2e
Phillips, L. D. (2010). Manual of IV therapeutics: Evidence-based practice for infusion therapy (5th ed.). F. A. Davis Company.
Martini, F. H., Nath, J. L., & Bartholomew, E. F. (2018). Essentials of Anatomy and Physiology (8th ed.). F.A. Davis Company.
Marieb, E. N., & Hoehn, K. (2018). Human anatomy & physiology (11th ed.). Pearson Education.
