7 Chapter Seven: Complications of Intravenous Therapy
Learning Objectives
- Discuss common complications associated with intravenous therapy, including infiltration, phlebitis, extravasation, infection, and air embolism.
- Discuss complications of central venous access devices (CVADs).
- Identify and mitigate risk factors associated with IV therapy.
- Recognize the clinical manifestations of common complications of IV therapy and fluid and electrolyte imbalances.
- Discuss how to prevent and manage complications of IV therapy and fluid and electrolyte imbalances.
- Evaluate patient outcomes related to IV therapy complications and the effectiveness of implemented interventions.
Nursing in Louisiana
Takara reiterated the potential complications associated with IV therapy. Takara explained the clinical manifestations that could arise from IV administration, such as swelling, infection, or discomfort at the insertion site, and emphasized the need for Mrs. Dupree to inform her immediately if any complications were experienced.
Introduction
Intravenous therapy is a common medical intervention in patient care which allows for the efficient delivery of fluids, medications, and nutrients directly into the bloodstream. Therefore, it’s imperative that healthcare professionals have a comprehensive understanding of the complications of IV therapy. This chapter will discuss how to identify, assess, and manage complications arising from IV therapy.
Complications of IV Therapy
Complications are categorized as local or systemic. Throughout this chapter, learners will explore common local complications such as infiltration, phlebitis, extravasation, and infection. Additionally, we will discuss systemic complications that can occur with IV therapy such as catheter-related bloodstream infection (CRBSI), air embolism, and fluid overload. Emphasis will be placed on implementing effective preventative measures, recognizing early clinical manifestations, and responding promptly to complications to ensure patient safety and optimal outcomes.
Local Complications
We will start by discussing local IV therapy complications including infiltration, phlebitis, extravasation, and infection. Complications can range from non-severe to severe. Extravasation, for example, can lead to tissue damage and necrosis, infection, loss of function, scarring and disfigurement, and compartment syndrome, in rare cases (Ignatavisius et al., 2024). If complications occur, the healthcare professional should stop the IV and remove it immediately and replace it at a different site. Notify the healthcare provider and initiate nursing interventions to relieve symptoms. In some cases of extravasation, an antidote is infused before IV removal, depending on the vesicant. Descriptions, causes, clinical manifestations, nursing interventions, prevention, and images are summarized below (Ignatavisius et al., 2024; INS, 2024; OpenStax, 2025).
Complication: Infiltration

- Infiltration Description: IV fluid or medication leaks into the surrounding tissue instead of the vein.
- Causes: Improper insertion, catheter displacement, or occlusion.
- Clinical Manifestations: Improper insertion, catheter displacement, or occlusion. Skin tight, cool, blanched, edematous around catheter; may be painful; IV rate slows with increasing swelling around the site.
- Nursing Interventions: Remove the IV, elevate the affected limb, and apply cold or warm compresses.
- Prevention: Stabilize the catheter and use the smallest appropriate size; avoid areas of flexion. If necessary, secure the site with an armboard; Regularly assess the site and educate the patient on activities to avoid, as well as the signs and symptoms of infiltration.
Complication: Phlebitis
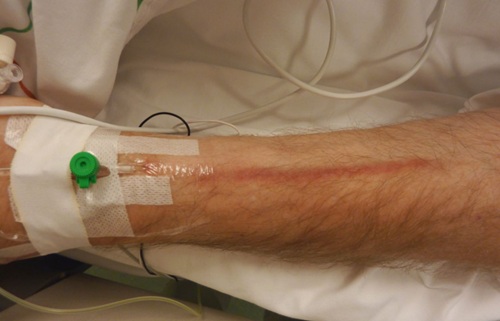
Retrieved from https://casereports.bmj.com/content/2016/bcr-2016-216448.full?sid=39b2cfd9-37f2-447d-bb40-64e8335a1d3c on 2nd April 2021
- Phlebitis Description: Inflammation of the vein at the catheter insertion site.
- Causes: Chemical or mechanical irritation, infection, or prolonged use.
- Clinical Manifestations: Pain, tenderness, redness, warmth along the vein from the access site, with possible red streaks and/or a palpable cord along the vein.
- Nursing Interventions: Discontinue the IV, apply warm compresses, and use anti-inflammatory meds.
- Prevention: Use smallest appropriate size; Avoid areas of flexion; Secure the catheter.
Complication: Extravasation
- Extravasation Description: IV infusion of a vesicant (irritant) drug causes tissue damage.
- Causes: Infusion of chemotherapy or irritant drugs.
- Clinical Manifestations: Similar to infiltration, blistering and tissue sloughing may not become apparent for several days and can take 1–4 weeks to resolve, especially with the infiltration of certain chemotherapeutic agents.
- Nursing Interventions: Stop the infusion, attempt to aspirate the drug, and follow protocols for the specific drug involved (e.g., antidote).
- Prevention: Identical to infiltration; Choose the correct vascular access device and site for administering vesicant medications; Identify the vesicant potential before administering any IV medication.
Complication: Infection

- Infection Description: Local or systemic infection caused by bacteria or fungi.
- Causes: Poor aseptic technique, prolonged catheter use, or contamination.
- Clinical Manifestations: Site appears red, swollen, and warm, with tenderness present. Purulent or foul-smelling exudates may also be observed.
- Nursing Interventions: Remove the catheter, clean the site, administer antibiotics, and monitor for systemic symptoms.
- Prevention: Always apply strict aseptic technique when inserting, maintaining, or removing catheters; Follow evidence-based hand hygiene practices; Ensure the dressing stays clean, dry, and securely adhered to the skin at all times.
Systemic Complications
Now let’s review systemic IV therapy complications. Systemic complications affect the entire vascular system or multiple body systems, not just the IV site. These can be life-threatening and often require urgent medical intervention. If complications occur, the healthcare professional should stop the IV and remove it immediately and replace it at a different site. Notify the healthcare provider and initiate facility protocols. Descriptions, causes, clinical manifestations, nursing interventions, prevention, and images are summarized below (Ignatavisius et al., 2024; INS, 2024; OpenStax, 2025).
For patients receiving replacement of electrolytes like sodium, potassium, or magnesium via IV route, this route is faster than oral administration. However, nurses must carefully administer the correct doses and maintain therapeutic levels. Monitoring includes regular blood tests for sodium and potassium, along with assessing the patient for signs of overdose or toxicity (OpenStax, 2025).
Complication: Catheter-Related Bloodstream Infection

https://www.idse.net/Review-Articles/Article/05-17/Prevention-of-CatheterRelated-Bloodstream-Infections-2017/41154?ses=ogst
- Catheter-Related Bloodstream Infection Description: Infection that enters the bloodstream via the catheter.
- Causes: Poor sterile technique, prolonged catheter use, or infection at the insertion site.
- Clinical Manifestations: Patient may report shortness of breath and cough; blood pressure is elevated; puffiness around the eyes; edema in dependent areas; engorged neck veins; moist breath sounds; dyspnea on exertion; decreased oxygen levels.
- Nursing Interventions: Remove the catheter, initiate systemic antibiotics, and monitor for sepsis.
- Prevention: Adhere to sterile technique and implement the recommended CRBSI prevention bundle (Centers for Disease Control and Prevention[CDC], 2024)
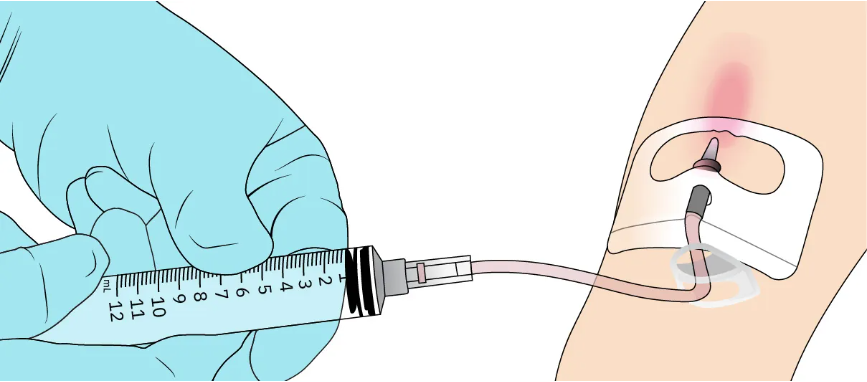
Complication: Air Embolism

Retrieved from https://vascularaccess.com.au/2017/05/14/air-embolism-understanding-why-it-occurs-and-how-to-prevent-it/ on 2nd April 2021
- Air Embolism Description: Air enters the bloodstream, potentially causing blockage.
- Causes: Improper priming of the IV line or disconnection from the catheter.
- Clinical Manifestations: Patient may experience dyspnea, tachypnea, coughing, chest pain, hypoxia or decreased oxygen saturation, altered mental status, dizziness, seizures, loss of conscious- ness, visual disturbances, tachycardia, hypotension, murmur, anxiety, cyanosis, jugular vein distension, cardiac arrest.
- Nursing Interventions: Clamp the line, position the patient in Trendelenburg, and administer oxygen; obtain vital signs.
- Prevention: Prime all IV tubing; secure all IV tubing connections, use air-eliminating filters (if applicable); avoid letting IV bags run dry; For central lines, clamp catheter before disconnecting, place patient in Trendelenburg position for insertion/removal; During central line removal, have patient perform Valsalva Maneuver; apply air-tight dressing immediately after removal.
Complication: Fluid Overload

- Fluid Overload Description: Excess fluid administration causing swelling or respiratory distress.
- Causes: Rapid infusion rates, kidney failure, or heart failure.
- Clinical Manifestations: The patient may report shortness of breath and coughing. Clinical signs include elevated blood pressure, periorbital puffiness, dependent edema, and engorged neck veins. Moist breath sounds may be present, along with dyspnea on exertion (DOE) and decreased oxygen saturation (SaO2).
- Nursing Interventions: Reduce the infusion rate, administer diuretics, and monitor vital signs and fluid balance.
- Prevention: Closely monitor intake and output, and promptly notify the healthcare provider if any imbalance is detected.
Complication: Electrolyte Imbalances
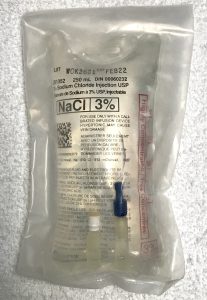
- Electrolyte Imbalances Description: Key minerals in the body, such as sodium, potassium, calcium, magnesium, chloride, and phosphate are too high or too low.
- Causes: Excessive administration of electrolyte- rich fluids; inappropriate IV fluid selection; rapid infusion rates; renal impairment; inadequate monitoring.
- Clinical Manifestations: Clinical manifestations vary based on the specific electrolyte imbalance.
- Nursing Interventions: Careful monitoring and individualized care; educate patient on electrolyte imbalances and encourage them to report symptoms; if imbalance is identified, stop infusion and notify healthcare provider; promptly adjust IV fluid composition or rate and administer electrolyte replacements or restrictions per provider orders.
- Prevention: Assess patient’s baseline electrolyte levels; select IV fluids that align with patient needs; administer at appropriate rate; avoid overuse of hypotonic or hypertonic solutions; regularly monitor serum electrolyte levels, intake and output, observe for clinical manifestations of imbalance.
Complications of Central Venous Access Devices
Complications specific to central venous access devices include catheter migration, catheter dislodgement, catheter rupture, and lumen occlusion. Notify the healthcare provider and follow facility protocol if complications occur. Descriptions, causes, clinical manifestations, nursing interventions, and prevention are summarized below. (Ignatavisius et al., 2024; INS, 2024).
Complication: Catheter Migration
- Catheter Migration Description: Displacement of the catheter tip to a different vein without any change in the external catheter length.
- Causes: Alterations in intrathoracic pressure may result from actions such as coughing, vomiting, sneezing, heavy lifting, or conditions like congestive heart failure.
- Clinical Manifestations: Migration to the jugular vein may cause the patient to report a gurgling or running water sound on the catheter side; migration to the azygos vein may result in back pain between the shoulder blades; infusion of medications in these cases can lead to neurological complications.
- Nursing Interventions: Discontinue all infusions and flush the catheter; notify the healthcare provider; if needed, obtain a chest X-ray to verify catheter tip placement; Catheter may reposition spontaneously to the superior vena cava (SVC), but radiologic repositioning might be necessary.
- Prevention: Ensure the catheter tip is positioned in the lower third of the SVC near the cavoatrial junction; advise the patient to continue normal daily activities while avoiding strenuous physical exertion.
Complication: Catheter Dislodgement
- Catheter Dislodgement Description: Catheter displacement at the insertion site, either inward or outward.
- Causes: Insufficient catheter stabilization; excessive physical activity while a PICC is in place.
- Clinical Manifestations: A change in external catheter length may indicate a shift in internal tip position, often without immediate signs or symptoms.
- Nursing Interventions: Stop all infusions and flush the catheter; do not readvance it; measure external length and compare to insertion records; notify the provider for evaluation; imaging may be needed.
- Prevention: Apply an appropriate catheter securement device; advise the patient to maintain regular daily activities while avoiding strenuous physical exertion.
Complication: Catheter Rupture
- Catheter Rupture Description: Catheter is fractured, compromised, or detached from the hub or port body
- Causes: Flushing a catheter forcefully with any syringe size against resistance; using scissors to remove a dressing; catheter compression in a subclavian- inserted line between the clavicle and first rib (pinch-off syndrome).
- Clinical Manifestations: Fluid leakage at the insertion site; pain or swelling during infusion; blood reflux into the catheter; inability to aspirate blood.
- Nursing Interventions: Repair the damaged segment if a compatible repair kit is available; this is a temporary solution; remove the catheter if necessary.
- Prevention: Avoid using excessive force when flushing a catheter; use a 10-mL syringe to prevent high pressure; prefer inserting the catheter through jugular or upper extremity sites rather than the subclavian site.
Complication: Lumen Occlusion
- Lumen Occlusion Description: Catheter lumen is either partially or fully blocked.
- Causes: Precipitates (e.g., calcium, diazepam, phenytoin); lipid sludge, blood clots, fibrin sheath, and prolonged connection of administration sets after infusion.
- Clinical Manifestations: Infusion stops; pump alarm; difficulty administering fluids or drawing blood; increased resistance during flushing.
- Nursing Interventions: Assess catheter history; sudden issues may indicate incompatible medications, while gradual problems suggest clot formation; for drug precipitates, check pH and use hydrochloric acid (acidic) or sodium bicarbonate (alkaline); use alteplase for blood clots.
- Prevention: Flush with normal saline before, between, and after medications; flush thoroughly after blood draws; use positive-pressure flushing with negative fluid-displacement connectors and a positive fluid-displacement connector; flush immediately after medication infusion.
Documentation
Here are examples of documentation for expected findings and unexpected findings.
Expected Findings
Initiated IV infusion of normal saline at 150 mL/hr using existing 20-gauge IV catheter located in the left hand. The IV site is free from pain, coolness, redness, or swelling. (WisTech Open, 2023).
Unexpected Findings
Attempted to initiate IV infusion in left hand with existing 20-gauge IV catheter. IV site free from pain, redness, or signs of infiltration. IV site flushed readily with normal saline. Normal saline IV fluids connected at 175 mL/hour with immediate leaking around infusion site. Swelling noted superior to infusion site. Fluids stopped immediately. (WisTech Open, 2023).
Key Takeaways
-
Importance of Understanding IV Complications
- IV therapy is essential for delivering fluids, medications, and nutrients efficiently, but it carries risk.
- Healthcare professionals must recognize, prevent, and manage complications promptly to ensure patient safety and positive outcomes.
- Complications are classified as local (at or near the IV site) or systemic (affecting the entire body).
-
Local Complications
- Local complications occur at the IV insertion site and can range from mild irritation to serious tissue injury.
- Infiltration
- Cause: IV fluid leaks into surrounding tissue.
- Signs: Cool, pale, swollen skin; slowed IV rate; discomfort.
- Actions: Stop IV, remove catheter, elevate limb, apply compresses.
- Prevention: Stabilize catheter, avoid flexion sites, frequent site checks.
- Phlebitis
- Cause: Inflammation due to chemical/mechanical irritation or infection.
- Signs: Pain, redness, warmth, red streaks, palpable vein cord.
- Actions: Discontinue IV, apply warm compress, use anti-inflammatories.
- Prevention: Use smallest gauge possible; secure catheter properly.
- Extravasation
- Cause: Vesicant (irritant) drug infiltrates tissue.
- Signs: Blistering, tissue sloughing, possible necrosis.
- Actions: Stop infusion, aspirate drug if possible, administer antidote per protocol.
- Prevention: Verify vesicant risk; use correct vascular access device.
- Infection
- Cause: Poor aseptic technique or prolonged catheter use.
- Signs: Redness, warmth, swelling, tenderness, purulent drainage.
- Actions: Remove catheter, cleanse site, administer antibiotics.
- Prevention: Maintain strict aseptic technique, hand hygiene, clean/dry dressing.
- Infiltration
- Local complications occur at the IV insertion site and can range from mild irritation to serious tissue injury.
- Systemic Complications
- Systemic complications affect the entire vascular or organ system and can be life-threatening.
- Catheter-Related Bloodstream Infection (CRBSI)
- Cause: Bacteria enter bloodstream via catheter.
- Signs: Fever, chills, hypotension, signs of sepsis.
- Actions: Remove catheter, start systemic antibiotics, monitor for sepsis.
- Prevention: Use sterile technique; follow CDC CRBSI prevention bundle.
- Air Embolism
- Cause: Air enters the bloodstream through improper priming or disconnection.
- Signs: Dyspnea, chest pain, cyanosis, altered consciousness.
- Actions: Clamp line, place in Trendelenburg, give oxygen, monitor vitals.
- Prevention: Prime tubing, secure connections, clamp lines before disconnection.
- Fluid Overload
- Cause: Excessive or rapid IV infusion, renal or heart failure.
- Signs: Shortness of breath, edema, high BP, moist breath sounds.
- Actions: Slow infusion, give diuretics, monitor I&O and vitals.
- Prevention: Control infusion rate, assess fluid balance closely.
- Electrolyte Imbalance
- Cause: Incorrect fluid selection, rapid infusion, poor monitoring.
- Signs: Depend on affected electrolyte (e.g., muscle weakness, arrhythmia).
- Actions: Stop infusion, notify provider, correct imbalance.
- Prevention: Monitor labs, select appropriate fluids, educate patient.
- Catheter-Related Bloodstream Infection (CRBSI)
- Systemic complications affect the entire vascular or organ system and can be life-threatening.
- Central Venous Access Device (CVAD) Complications
- Catheter Migration: Tip moves to another vein — stop infusions, verify via X-ray.
- Catheter Dislodgement: External catheter length changes — stop infusions, notify provider.
- Catheter Rupture: Caused by excessive pressure or forceful flushing — stop infusion, repair or remove catheter.
- Lumen Occlusion: Blocked lumen due to clots or drug precipitate — assess cause, flush appropriately, use alteplase if needed.
- Documentation Essentials
- Document site condition, type of complication, interventions, and patient response.
- Example: “Fluids stopped immediately; swelling noted above site; site elevated.”
- Thorough, timely documentation supports patient safety and legal protection.
Review Questions
References
Centers for Disease Control and Prevention (2024, February 28). Background Information: Strategies for Prevention of Catheter-Related Infections in Adult and Pediatric Patients. CDC. https://www.cdc.gov/infection-control/hcp/intravascular-catheter-related-infection/prevention-strategies.html
Exline, M. C. & Sopirala, M. M. (2017). Prevention of catheter-related bloodstream infections, 2017: An overview of current approaches in diagnosis, management, and prevention. Infectious Disease Special Edition, Spring 2017, 65-72.
Ignatavisius, D. D., Rebar, C. R., & Heimgartner, N. M. (2024). Concepts of infusion therapy. In J. H. Ingalls (Ed.), Medical-Surgical nursing: Concepts for clinical judgment and collaborative care (11 ed., pp. 285-315). Elsevier.
Infusion Nurses Society (INS). (2024). Infusion therapy standards of practice (9th ed.). Journal of Infusion Nursing, 47(Suppl. S1), S1–S285.
OpenStax (2025). Clinical Nursing Skills. Rice University. Creative Commons Attribution 4.0 International License Retrieved from https://openstax.org/books/clinical-nursing-skills/pages/13-3-intravenous-infusion
WisTech Open (2023). Nursing Skills (2nd edition).Creative Commons Attribution 4.0 International License Retrieved from https://wtcs.pressbooks.pub/nursingskills/chapter/23-4-sample-documentation/
