2 Chapter Two: Legal and Ethical Considerations of Intravenous Therapy
Learning Objectives
- Summarize the major legal implications and limitations of intravenous therapy related to the Louisiana Nurse Practice Act.
- Identify and explain ethical principles that guide the practice of intravenous therapy such as autonomy, beneficence, non-maleficence, and justice as guided by the Code of Ethics for Nurses from the American Nurses Association.
- Demonstrate knowledge of the process of obtaining informed consent before initiating intravenous therapy.
- Understand the legal implications of negligence and malpractice related to intravenous therapy and the responsibilities of healthcare providers.
Nursing in Louisiana
Type your examples here.
- First
- Second
Introduction
Healthcare systems rely on the expertise of varied practitioners to provide high-quality care to all patients. Physicians, nurses, medical assistants, phlebotomists and many others play a direct role in the delivery of safe and ethical care. Since IV therapy is one of the most common invasive medical procedures performed today, it is imperative that the related legal and ethical implications are reviewed and understood. A competent healthcare professional has the education and training necessary to perform intravenous therapy in a safe and effective manner. Many organizations contribute to the process and oversight of standards of care that guide clinical decisions resulting in optimal outcomes. Understanding policy on the local, state, and federal level will ensure the professional remains within the bounds of the law. Healthcare professionals have the responsibility to adhere to these laws and regulations and are accountable for their actions. Every patient deserves fair and equitable treatment that preserves their dignity and individual rights.
Legal Frameworks for IV Therapy
Federal Regulations
On a federal level there are regulations and policies related to IV therapy that establish standards of care. These standards are used to determine a facility’s reimbursement eligibility from the Centers for Medicare and Medicaid Services (CMS) and can be found in Title 42 of the Code of Federal Regulations. While these specific guidelines are tied to financial accountability, they are also considered standard practice and are often incorporated into more specific policies within each state or facility. The Infusion Nurses Society (INS) is an international organization that has developed a set of high-quality Standards of Practice used by much of the U.S. healthcare industry. Failure to meet standards of practice can lead to legal repercussions. Malpractice related to intravenous (IV) therapy occurs when a healthcare professional performs below the established standard, resulting in harm or injury to the patient. A practitioner can be guilty of negligence when intravenous therapy is not monitored or safety protocols are not followed.
Scope of Practice
Each state has a Nurse Practice Act which defines the roles and responsibilities for various healthcare providers (Registered Nurses, Practical or Vocational Nurses, and Medical Assistants) in IV therapy. Louisiana’s Nurse Practice Act is found in the Louisiana Administrative Code Title 46 and outlines professional and occupational standards of both Registered Nurses and Licensed Practical Nurses. “Scope of practice describes the services that a qualified health professional is deemed competent to perform, and permitted to undertake – in keeping with the terms of their professional license.” (ANA)
A member of the healthcare team can initiate IV therapy, perform interventions, and assess the patient’s health status if legally permitted by the Scope of Practice.
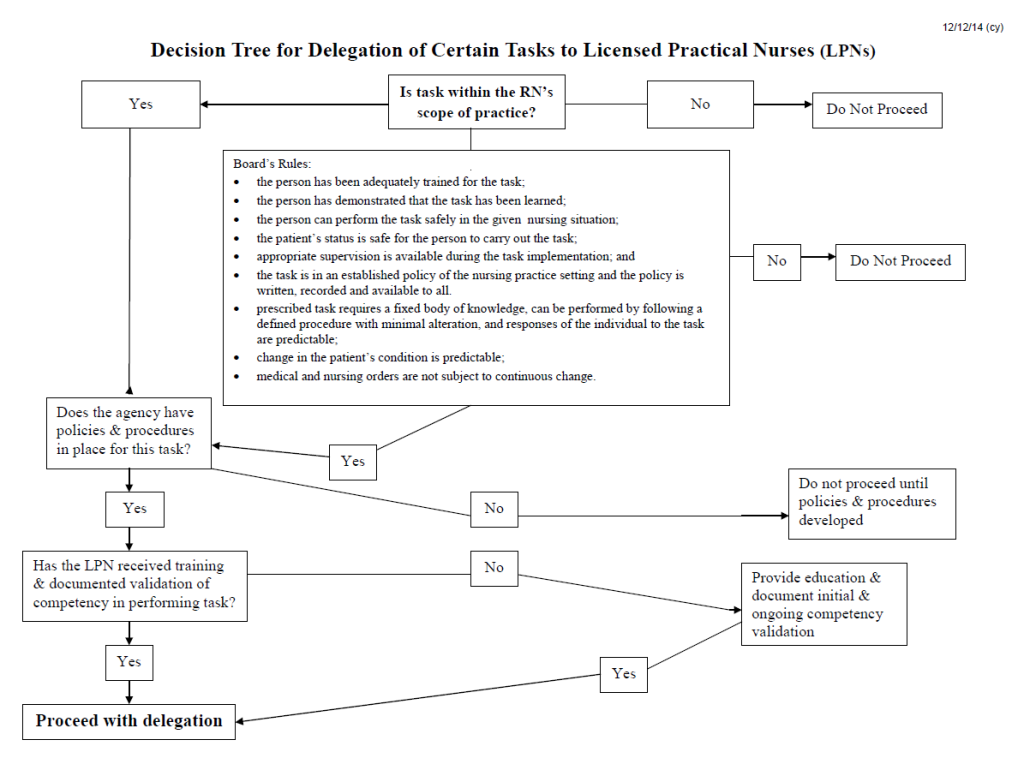
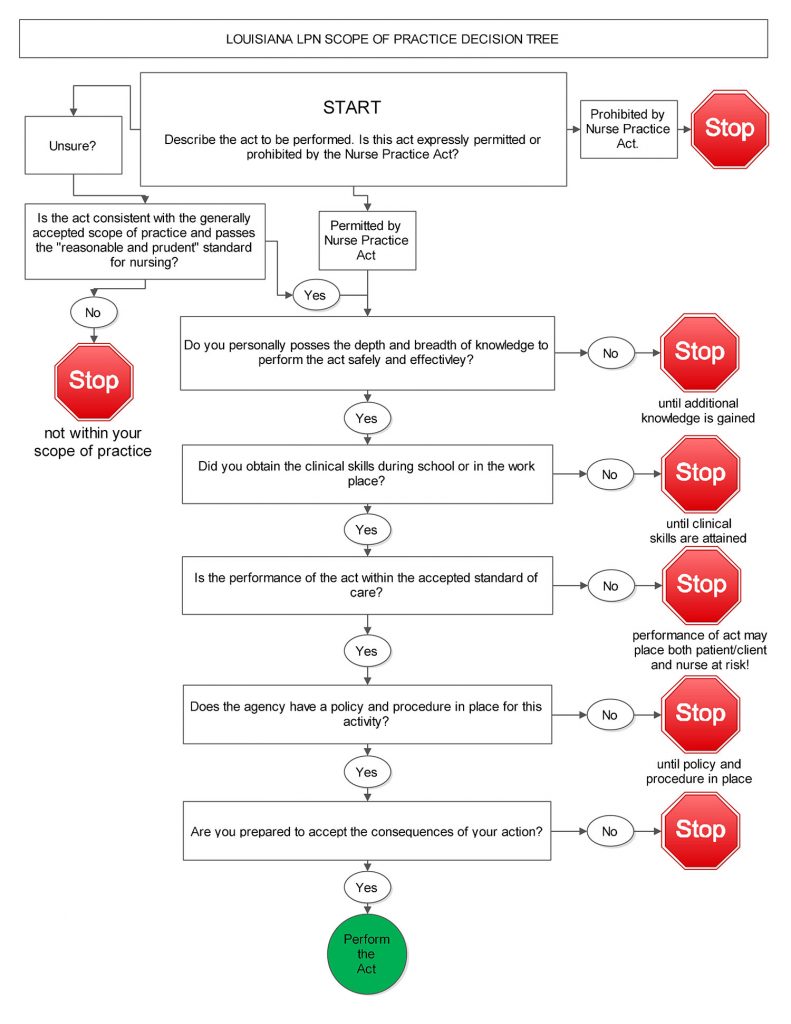
Licensed Practical Nurses and Registered Nurses in Louisiana may legally perform any of the duties related to IV therapy if they have been sufficiently trained and are knowledgeable in the skill. Both can perform advanced skills such as accessing central devices and blood products. The difference in allowable versus actual practice is related to the rules of delegation defined in the law. The Louisiana State Board of Nursing, which oversees the Advanced Practice Registered Nursing (APRN) and Registered Nurse (RN) professions and students, provides a Delegation Decision Tree (Figure 2.1) to guide the nurse’s actions. Likewise, the Louisiana State Board of Practical Nurse Examiners, which oversees Licensed Practical Nurses (LPN) and students, has a similar Scope of Practice Decision Tree. (Figure 2.2)
Delegation is the process of conferring duties onto another practitioner while maintaining personal responsibility. It is required that in order to delegate a task the nurse must determine the competence of the individual as the outcome will become a shared responsibility. Nurses are accountable for anything that is delegated to another individual and must have supervisory capacity. Intravenous therapy is considered a complex task by definition as clinical judgement is required. Therefore, unlicensed personnel such as medical assistants and phlebotomists are not usually permitted to perform IV catheterization or administer medications and fluids. Registered Nurses may delegate intravenous therapy procedures to Licensed Practical Nurses within specific guidelines. The Louisiana Administrative Code does not allow delegation of chemotherapy, investigational drugs, total parenteral nutrition, blood products, or administration via the IV push route. Although LPNs may be competent and these skills are implicitly allowed, because most facilities place the RN as the direct supervisor to the LPN, these skills are often not assigned to LPNs. In the event that an LPN is directly supervised by a Nurse Practitioner (NP) or Physician, the LPN is legally allowed to perform any of these advanced skills.
Institutional Policies
Many facility policies are driven by the limitations of the Nurse Practice Act. For instance, IV push administration or medications used for cancer treatment are usually assigned to RNs since the law does now allow delegation of these skills. It is important that healthcare professionals are familiar with institutional policies and ensure they align with the law. Following protocols and utilizing evidence-based practice helps to minimize risks, such as infection or medication errors.
Professional Standards
Clinical Competency
In addition to what is legally allowable for a particular provider, ‘Standards of Care’ refer to the level of skill, diligence, and care that a reasonably competent healthcare professional in the same field would provide under similar circumstances. These standards serve as guidelines for medical practice and help determine whether a healthcare provider acted appropriately in a given situation. Competency is defined as “a determination of an individual’s capability to perform expectations.” (Phillips, 2010) by the Joint Commission for Accreditation of Healthcare Organizations (JCAHO). Providers involved in intravenous therapy must have the clinical knowledge and skill to appropriately manage patient care. Competency must be documented and verified by the employer. This may be done by verification of educational training, documented continuing education, or clinical skills checklists or competency assessments. Legally, the healthcare provider is responsible for proving competency in multiple areas. Competency may include elements of accountability, communication, collaboration, and autonomy in decision making. Failure to meet the standard of care can lead to allegations of negligence or malpractice if it results in patient harm. However, as seen in the case study below, even if an adverse event occurs, a healthcare provider may still be found to have met the standard of care if they acted competently and followed accepted medical practices.
Along with JCAHO, The Infusion Nurses Society (INS) and Association for Vascular Access (AVA) are organizations that have a set of Standards of Practice and offer online education, continuing education, and resources for nurses involved in infusion therapy. These organizations publish professional medical journals on the topic. They do require membership to gain full access to all resources.
Case Study: IV Infiltration
A 40-year-old female patient undergoing Mitomycin chemotherapy for cancer alleged that a nurse improperly inserted an intravenous (IV) line, causing infiltration of the drug into her right hand. This led to tissue necrosis, multiple surgeries, and permanent loss of function in two fingers. The patient also claimed inadequate nurse supervision contributed to the injury.
The nurse followed protocol, immediately stopping the IV upon noticing displacement and notifying a physician. No immediate complications were documented. However, three months later, the patient developed severe complications, including deformity and chronic pain.
While defense experts confirmed the nurse met the standard of care and staffing levels were adequate, legal complexities led to an eventual settlement. After multiple expert reviews affirmed the nurse’s actions, a settlement of $235,000 was reached, preventing further legal risk.
Consider how the nurse’s actions in upholding standards of care as well as adequate documentation played a role in the outcome of this case. Knowing the legal implications of IV therapy and the provider’s role are crucial to mitigating risk and legal consequences.
Adapted from Nurse Case Study: Improper administration and monitoring of Mitomycin by Nurses Service Organization (NSO)
Ethical Principles
Ethics refers to the principles, values, and standards that guide the professional conduct of healthcare professionals. It provides a framework for making decisions that ensure the dignity, well-being, and rights of patients while maintaining professional integrity. The main ethical principles related to IV therapy are listed below. (Table 2.1)
Ethical Prinicples
| Ethical Principle | Definition | IV Therapy Connection |
|---|---|---|
| Autonomy | “The principle that an individual has the right to make their own decisions about their own life and body, even when those decisions might be different from what healthcare providers recommend.”(OpenStax, 2024, section 1.3) | Respecting patients’ autonomy in choosing or refusing IV therapy. |
| Nonmaleficence | “The principle that nurses have an obligation to do no harm intentionally.”(OpenStax, 2024, section 1.3) | Ensuring that IV therapy benefits patients without causing harm.
Take steps to prevent harm, such as monitoring for adverse reactions, ensuring proper site care, and using aseptic techniques. |
| Beneficence | “The principle that nurses have an obligation to do good and promote the well-being of patients.” (OpenStax, 2024, section 1.3) | Understanding the purpose of IV therapy and the necessity on a patient-by-patient basis. |
| Justice | “The principle that all individuals should be treated with fairness and equity.” (OpenStax, 2024, section 1.3) | Providing equal access to IV therapy regardless of patient background or status.
Advocating for patient preferences or concerns, such as alternative treatments. |
| Fidelity and Trust | The principles that healthcare professionals should act with honesty and build a relationship with each patient based on respect. This leads to patient confidence. | Building trust through honest communication and adherence to ethical standards.
Staying updated on best practices and institutional policies related to IV therapy. |
Table 2.1 Ethical Principles
One source of ethical guidelines is the American Nurses Association (ANA) which provides a Code of Ethics for Nurses, including principles applicable to IV therapy. Ethical practice of IV therapy may include reporting errors or complications honestly and seeking guidance when needed. Ethics emphasizes the nurse's responsibility to provide safe, effective, and patient-centered care while upholding principles such as autonomy, beneficence, and non-maleficence.
Learn More
Patient Rights
Informed Consent
Healthcare Professionals must ensure informed consent by clearly explaining the purpose, benefits, and risks of IV therapy, respecting the patient’s right to make decisions about their care. Initiating IV therapy is an invasive procedure that is not without risks.
By outlining the benefits, such as rapid medication delivery or fluid replacement, patients can understand the necessity and advantages of IV therapy. However, transparency about potential risks is essential so the patient maintains autonomy and makes an informed decision. Open communication empowers the patient to actively participate in their care. Trust builds between patients and healthcare providers while minimizing ethical or legal conflicts. All patients maintain a right to refuse IV therapy. If fully informed, the patient’s decision must be respected and adhered to. A healthcare professional can be legally charged with assault or battery for violating this right.
It should also be noted that there may be special considerations regarding obtaining consent for minors, unconscious patients, or those with impaired decision-making ability. It should be determined who is the legally responsible party by verifying legal guardianship or power of attorney. Documentation should be included in the health record for reference if the patient is unable to provide consent for themselves.
Confidentiality and Privacy in IV Therapy
As with any patient experience, confidentiality must be upheld. Safeguarding patient information related to IV therapy ensures compliance with Patient Privacy Laws such as the Health Insurance Portability and Accountability Act (HIPAA). Any information related to a patient’s IV therapy, such as medication details, dosage, reasons for the therapy, or associated conditions, is considered protected information and should only be accessible to those directly involved in the patient’s care. Care should also be taken to remove visitors or other personnel according to the patient’s preference when procedures or interventions are being performed. More information about patient rights and the law can be found in the Louisiana Administrative Code Title 48, Part I 69 §9319. Patient Rights and Privacy.
Documentation and Record-Keeping
Documentation of IV therapy is a communication tool between healthcare providers. Documentation should be accurate, timely, and thorough in order to prove standards of care were met and monitor patient outcomes. The patient chart is a legal document that can be used as a defense in a court of law. Litigation related to IV therapy is commonly seen in the following categories:
- Failure to monitor or assess clinical status
- Failure to prevent infection
- Failure to use equipment properly
- Failure to protect from avoidable injury (Phillips, 2010, p. 10)
The healthcare provider’s risk can be mitigated with proper documentation. Reporting adverse events and near misses according to facility policy are essential for quality improvement evaluation. It is of the utmost importance to avoid negligence and malpractice violations.
Key Takeaways
- IV therapy is a common invasive procedure requiring legal and ethical understanding.
- Healthcare providers must follow local, state, and federal policies to avoid malpractice, ensure patient rights, and ensure reimbursement for the facility.
- Each state’s Nurse Practice Act defines IV therapy roles for healthcare providers.
- The INS sets widely accepted standards of practice.
- In Louisiana, RNs and LPNs can perform IV therapy if trained and competent.
- Delegation rules allow RNs to assign IV therapy tasks to LPNs within legal guidelines.
- LPNs cannot be delegated to tasks such as IV push administration, chemotherapy, or blood product administration unless directly supervised by an NP or physician.
- Unlicensed personnel (medical assistants, phlebotomists) generally cannot perform IV catheterization or medication administration.
- Institutional policy may reflect evidence-based protocols that minimize risks such as infection or medication errors.
- Competency is verified through education, training, assessments, and continuing education.
- Failure to meet standards can lead to allegations of negligence or malpractice.
- Patients must be fully informed of IV therapy's purpose, risks, and benefits and they have the right to refuse.
- IV therapy information is protected under HIPAA regulations.
- Documentation is a legal and clinical tool ensuring proper IV therapy standards.
- Accurate patient records protect healthcare providers in legal cases.
Review Questions
References
Emily needs to update based on notes in file of what is an adaptation/reuse versus reference
Peripheral IV (PIV) Standards of Care article from AVA. https://meridian.allenpress.com/java/article/29/3/15/503118/Standards-of-Care-for-Peripheral-Intravenous
Louisiana Nurse Practice Act, LA. ADMIN. CODE tit. 46, [Specific Section Number] 2025. URL of the Louisiana Administrative Code.
OpenStax. (2024). Fundamentals of nursing. In 1.3 Nursing as a Profession. OpenStax. https://openstax.org/books/fundamentals-nursing/pages/1-3-nursing-as-a-profession
Phillips, L. D. (2010). Manual of IV therapeutics: Evidence-based practice for infusion therapy (5th ed.). F. A. Davis Company.
Nurses Service Organization. (n.d.). Nurse case study: Improper administration and monitoring of Mitomycin. Nurses Service Organization. https://www.nso.com/Learning/Artifacts/Legal-Cases/Nurse-Case-Study-Improper-administration-and-monitoring-of-Mitomycin
American Nurses Association. (n.d.). Scope of practice. https://www.nursingworld.org/practice-policy/scope-of-practice/
