6 Chapter Six: Maintaining and Monitoring Intravenous Therapy
Learning Objectives
- Demonstrate knowledge of evidence-based guidelines and best practices for safe intravenous therapy administration to reduce complications.
- Explain how to monitor infusion rates and adjust according to healthcare provider orders or patient needs.
- Discuss how to assess IV sites for clinical manifestations of infiltration, phlebitis, extravasation, or infection.
- Record patient assessment and changes to the IV site or therapy.
- Describe strategies for minimizing infection risks.
- Explain the importance of changing IV dressings and tubing according to protocol to reduce the risk of infection.
- Discuss considerations for the individuals with cardiovascular and/or renal disorders when monitoring IV therapy.
Nursing in Louisiana

Mrs. Dupree, a 47-year-old woman from Pierre Part, Louisiana, is admitted to the hospital after experiencing persistent nausea and vomiting for the last 48 hours. She reports that her symptoms began suddenly while she was preparing gumbo and have been never-ending, despite attempts to manage them with over-the-counter anti-nausea medication. She has also been unable to keep any food or fluids down, which has led to a noticeable decrease in energy and increased dehydration.
Takara is a 22-year-old nursing student from Napoleonville, Louisiana assigned to Mrs. Dupree. She is a junior nursing student who has cared for other patients with gastrointestinal (GI) disorders and has demonstrated a strong understanding of basic nursing skills, including patient assessment, IV insertion, and fluid management. Under the supervision of her clinical instructor, she will be responsible for monitoring Mrs. Dupree’s hydration status, assessing her response to IV therapy, and ensuring that the patient is comfortable and well-informed about her treatment plan. Takara will also educate Mrs. Dupree on the purpose of IV therapy, signs of complications to watch for, and when to seek assistance.
Introduction
After inserting and securing a peripheral intravenous catheter, the healthcare professional can initiate IV therapy if ordered. The IV system must then be maintained and monitored. The agency policies will mandate several key components to ensure patient safety and effective care. Although agency policies vary by institution, common elements such as IV equipment and supplies, site care, monitoring, complication management, documentation, infection control, and discontinuation will be discussed in this chapter.
Key Components of IV Therapy
There are several key components of IV therapy to ensure individual safety and effective care. These components aim to standardize practices, enhance individual safety, and ensure compliance with regulatory requirements. While specific policies may vary by agency, let’s discuss common aspects of IV therapy.
Initiation of IV Therapy
Education
Before initiating IV therapy, it’s important to educate the individual and family on what to expect with IV therapy. Let’s consider what should be communicated clearly and empathetically to the individual and family to ensure they understand the purpose, indications, potential risks and complications, and clinical manifestations to report when receiving IV therapy. The healthcare professional should acknowledge any fears or anxiety the individual or family may have about IV therapy and provide reassurance. To ensure they are fully informed, written instructions may be provided and answering any questions they have will help ease concerns.
First, its purpose. Intravenous therapy involves administering fluids, medications, or nutrients directly into the vein through a peripheral IV catheter. The healthcare professional should also inform them of the duration of the therapy and how frequently they may receive treatment. The fluids, electrolytes, and medications act rapidly in the body to restore fluid and/or electrolyte balance and deliver medications. Because of its rapid action in the body, it’s crucial to administer it safely to the patient.
Second, its indications. The reason for IV therapy could be for rehydration, providing medications (e.g., antibiotics, pain management, electrolyte replacement), delivering nutrients, or blood products. Some individuals may experience fluid and electrolyte imbalances that require treatment through IV fluid and electrolyte therapy. Other reasons for IV therapy include restricted diets during and after surgery (i.e., nothing by mouth diet) and corrective or replacement losses (e.g., excessive vomiting, urination, and/or diarrhea).
Third, its potential risks and complications. Some common side effects of IV therapy might include pain, swelling, or redness at the insertion site. Complications of IV therapy include infection, infiltration, phlebitis, extravasation, air embolism, and bleeding. We will discuss complications in further detail in Chapter 7.
Fourth, when to seek help. The healthcare professional should discuss the clinical manifestations to be aware of. Tell them to report excessive redness, swelling, pain, or signs of infection such as drainage or warmth at the site. Explain how air bubbles in the tubing are a concern and they should immediately inform the healthcare professional if this happens. Lastly, encourage the individual to report if they feel faint, dizzy, or experience any unusual reaction.
Maintaining and Monitoring the IV System
Now that you’ve covered IV therapy components and education, let’s review the maintenance and monitoring of the IV system (Table 6.1) to ensure its safety, effectiveness, and functionality.
| IV Maintenance and Monitoring Tasks | Details | Frequency/Action | Rationale |
|---|---|---|---|
| IV Site Assessment | Check IV site for patency and signs of complications. | Continuously during IV infusion | Identifies early signs of complications and ensures proper function |
| Sterile Dressing Change | Replace if wet, soiled, loose, or as per protocol | Every 48-72 hours | Reduces the risk of infection |
| IV Tubing Change | Replace per protocol, or with change of IV solution | Every 72-96 hours | Minimizes the risk of infection, ensures proper infusion, maintains tubing integrity, and promotes safe and effective treatment |
| Infusion Rate Adjustment | Check and adjust infusion rate if using IV pump; ensure correct volume is administered on time | As ordered | Ensures the proper delivery of fluids or medications at the correct amount and speed |
| IV Bag Inspection | Inspect for clarity, integrity, and expiration date | Before each use; discard if cloudy, leaking, or expired | Ensures patient safety and correct medication or fluid and prevents contamination |
| Patient Monitoring | Monitor for adverse reactions, fluid overload, or electrolyte imbalances | Continuously during IV infusion | Ensures patient safety, therapeutic effectiveness, and prompt detection of potential complications |
| Aseptic Technique Maintenance | Ensure aseptic technique is followed throughout the IV process, including during dressing changes | Throughout IV care | Prevents infections, ensures sterility of IV equipment, promotes patient safety, and promotes effective treatment. |
| Discontinuation of VAD | Removal of the device using | As ordered | Resolution of clinical need, infection, mechanical failure, or complications. |
| Documentation | Document all maintenance activities, patient responses, and changes in treatment plan | Ongoing throughout IV therapy | Ensures patient safety, promotes effective communication among the healthcare team, compliance with regulations, and meets legal and ethical standards |
Table 6.1 Evidence-based practices for IV maintenance and monitoring
IV Assessment
As long as the peripheral catheter is in place, the healthcare professional is responsible for assessing the IV site for patency and signs of complications. The IV site should be assessed per agency policy or protocol. The peripheral catheter may be saline locked (not receiving continuous IV therapy) or receiving continuous IV therapy. If the peripheral catheter is saline locked, only receiving an intravenous push (IV push) medication, intravenous piggyback (IVPB), or blood products, the healthcare professional should flush the peripheral catheter with normal saline per agency policy or protocol or before and after these administrations to assess patency. In some cases, normal saline followed by heparinized saline may be indicated (e.g., central lines) (Ignatavisius, et al., 2024). As the catheter is being flushed, assess for leakage, discomfort, and signs of complications. If the catheter is patent, the flush should flow freely without resistance or leakage and the patient should not report any discomfort upon palpation. If the patient is receiving continuous IV fluids, the IV site is assessed for signs of complications by visualizing the site through the transparent dressing and lightly palpating around the site. Document your findings in the patient’s electronic medical record (EMR).

Sterile Dressing Replacement
The sterile dressing (transparent dressing) protects the IV site from pathogens entering the surrounding tissue or bloodstream. The healthcare professional should follow the agency’s policy on routine expectations for replacing the sterile dressing. This usually occurs every 48-72 hours or when the dressing becomes wet, soiled, or loose.
IV Tubing Replacement
The IV tubing integrity is crucial for safe and effective treatment for patients. The healthcare professional should follow the agency’s policy on routine expectations when replacing the IV tubing. This usually occurs every 72-96 hours but may occur more frequently based upon the type of treatment. For example, total parenteral nutrition (TPN) typically requires that tubing be replaced every 24 hours to reduce the risk of infection because it contains high concentration of glucose which is a medium for bacterial growth.
If possible, change the IV tubing and solutions at the same time to minimize the number of times the IV system is opened, which limits contamination. The IV tubing should be inspected for punctures, contamination, or occlusions. When replacing the IV tubing, the healthcare professional should take precautions to prevent air emboli by properly priming the IV tubing to remove any air bubbles. The procedure for replacing IV tubing is similar to spiking and priming an IV bag; see Chapter 5 for details.
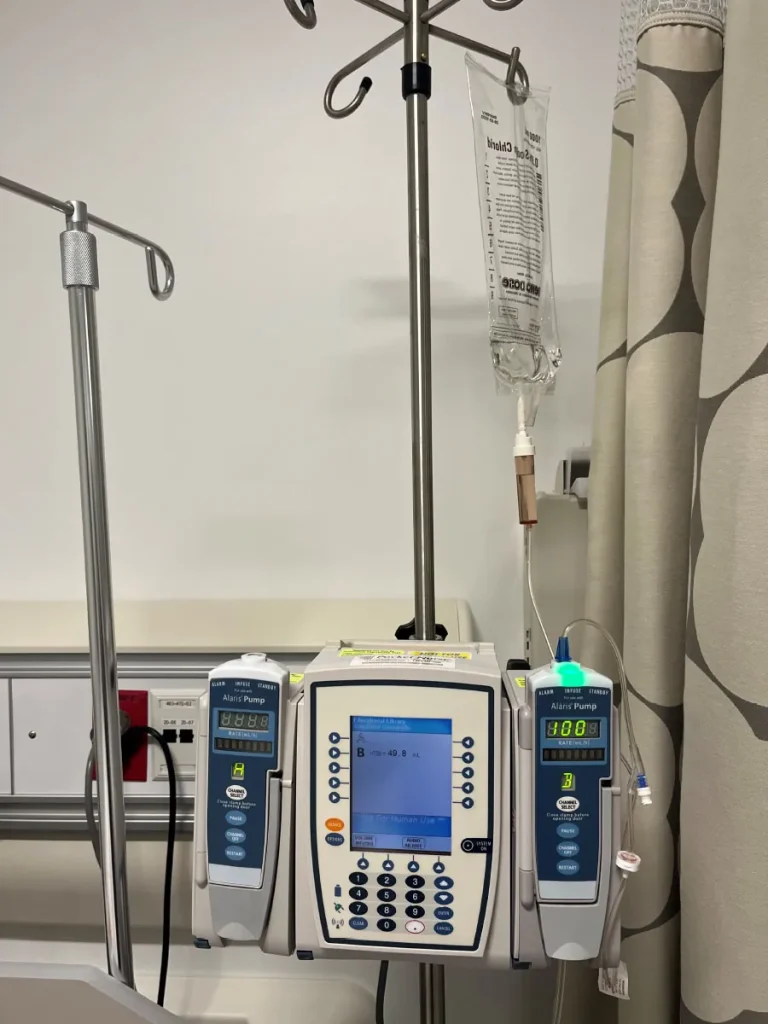
Infusion Rate Adjustment
To ensure that the patient is receiving the correct amount and speed of the IV fluids, the healthcare professional must routinely assess the IV pump to verify it is infusing properly.
IV Bag Inspection
Before replacing the IV solution, the healthcare professional should inspect the bag for discoloration, cloudiness, leakage, and expiration. This inspection ensures the integrity of the solution and patient safety to prevent infection.

Real RN Stories: The Importance of Assessing Equipment before Use
- Nurse: Kameka, RN
- Clinical setting: Emergency department
- Years in practice: 3
I was taking care of a patient who presented with high blood pressure. Another nurse on the unit started her IV while I went to prepare a dose of hydralazine. I went into the patient’s room, found the access port on the IV line, and administered the prescribed dose of hydralazine. Upon reassessing the vital signs, the patient’s blood pressure had not decreased. I followed the provider’s orders and administered a second dose of hydralazine. Again, the blood pressure had not decreased when reassessed. While I was in the room, the patient asked for another gown, as she said her gown was wet. Come to find out, the IV tubing was not tightly screwed on the IV hub, and the IV fluids were leaking into the bed instead of going into the patient’s vein. No wonder the blood pressure medication didn’t work, it had leaked into her bed instead of going into her vein. I informed the patient what had happened, spiked a new bag of fluids with a new set of tubing, and informed the provider of the incident. The provider ordered another dose of hydralazine, and the patient’s blood pressure subsided. Lesson learned, always check to make sure the tubing is secured to the IV site before administering medications.
Source: OpenStax, 2025
Patient Monitoring
Monitoring the patient for adverse reactions, fluid overload, or electrolyte imbalances, is an essential responsibility of the healthcare professional during IV therapy (Infusion Nurses Society (INS), 2024). For stable patients, the healthcare professional should monitor the patient every 1-2 hours (INS, 2024). Monitor every 15–30 minutes for critically ill patients, those receiving vesicants or irritants, or those unable to report symptoms (e.g., pediatric, unconscious, nonverbal) (INS, 2024).
Aseptic Technique
Maintaining the integrity of the IV tubing and peripheral catheter is essential in preventing infection. To accomplish this, the healthcare professional must use aseptic technique when manipulating the IV tubing and peripheral catheter. Use caution when disconnecting tubing to aid in mobility or patient care and never let the tubing touch the floor. The IV tubing has needleless injection ports where syringes and other adaptors can be inserted to administer medications. Before accessing the port, thoroughly clean the port with alcohol-based 2% chlorhexidine (preferred), 70% alcohol, or povidone-iodine solution and let it dry (INS, 2024).
Discontinuing the VAD
The technique for removing the vascular access device depends on the type of VAD. Regardless of the type of VAD, the procedure should be explained to the patient and any questions should be answered accordingly.
When removing a short peripheral catheter, gently lift the edges of the transparent dressing and pull it laterally to detach it from the site while keeping the catheter stable. Carefully withdraw the catheter from the skin and promptly cover the puncture site with dry gauze. Apply pressure to the site until bleeding stops. Inspect the catheter tip to ensure it is intact and fully removed. Record the time of catheter removal and note the condition of the IV site (Ignatavicius et al., 2024; OpenAI, 2024). Watch the vide below on IV removal.
Documentation
Throughout the course of therapy, the healthcare professional must follow the agency’s policies and procedures and document their assessment and any interventions in the EMR. To protect yourself from negligence and malpractice claims, remember to document the following (Ignatavisius et al., 2024):
- Location and condition of the IV therapy site
- Type and gauge of VAD
- Type of dressing and/or securement device
- Rate of the IV therapy
- Patient and family education provided
Here are examples of documentation for expected findings and unexpected findings.
Expected Findings
IV catheter on left forearm discontinued with IV catheter tip intact. Site free of redness, warmth, tenderness, or swelling. Gauze applied with pressure for one minute with no bleeding noted. Dressing applied to the site. (WisTech Open, 2023).
Unexpected Findings
IV catheter on left forearm discontinued with IV catheter tip intact. Site free of redness, warmth, tenderness, or swelling. Gauze applied with pressure for one minute. Bleeding noted to continue around gauze dressing. Pressure held for five minutes, and hemostasis achieved. Dressing applied to site. (WisTech Open, 2023).
Special Considerations
Because of the vulnerable nature of patients with cardiovascular and/or renal conditions, safety measures to avoid fluid volume overload must be considered. A patient with an IV infusion who has altered cardiovascular and/or renal function must be frequently monitored for signs of fluid overload which include elevated blood pressure and respiratory rate, crackles in the lungs, decreased oxygen saturation, and peripheral edema. Another important consideration when caring for the pediatric or elderly patient with an IV infusion is careful assessment of the IV site. Because of the fragility of the venous walls in these populations, IV sites must be monitored and assessed carefully for patency. Ensure that the IV site is secured and it remains free of moisture. Mobile children may need guidance to avoid accidentally sitting or lying on the tubing and causing a blockage. In elderly patients, it's important to closely monitor IV site patency when administering large volumes of fluids at higher rates and adjust the infusion rate as needed.
Chapter Closer

Mrs. Dupree has been diagnosed with fluid volume deficit, commonly known as dehydration. This condition must be corrected to increase perfusion. Her healthcare provider has ordered normal saline at a rate of 100 ml/hr to address the condition. Normal saline is a commonly used IV solution to replace lost fluids and maintain electrolyte balance in patients who are dehydrated. Takara, her assigned nursing student, initiated the IV therapy for Mrs. Dupree. She programmed the IV smart pump at the prescribed rate of 100 ml/hr to ensure a controlled and accurate delivery of the normal saline solution.
Takara must maintain the IV therapy system and monitor the patient’s response to fluid replacement. She should assess Mrs. Dupree for indicators of adequate rehydration at least every 2 hours or per agency policy. This assessment would include the patient’s blood pressure, pulse quality, respirations, and temperature. Takara must also assess the IV infusion site hourly for indications of infiltration, phlebitis, and infection.
Key Takeaways
- Key Components of IV Therapy
- Aims to standardize practices, enhance individual safety, and ensure compliance with regulatory requirements.
- Initiation of IV Therapy
- Includes educating the individual and family about its purpose, indications, potential risks and complications, and when to seek help.
- IV Site Assessment
- Assess IV site for patency and complications (e.g., redness, swelling, infiltration).
- Assess continuously during infusion or per agency policy.
- Flush saline-locked catheters before and after medications or IVPB to maintain patency.
- Document findings in the electronic medical record (EMR).
- Sterile Dressing Replacement
- Replace the transparent dressing every 48–72 hours or when wet, soiled, or loose.
- Maintains a barrier against infection and protects IV integrity.
- IV Tubing Replacement
- Replace tubing every 72–96 hours, or more often for certain infusions (e.g., TPN every 24 hours).
- Change tubing and IV solution together to reduce contamination risk.
- Inspect and prime tubing to prevent leaks and air embolism.
- Infusion Rate Adjustment
- Regularly check IV pump settings to ensure proper infusion rate and volume.
- Ensures accurate medication/fluid delivery and patient safety.
- IV Bag Inspection
- Inspect IV solution for clarity, integrity, and expiration date before use.
- Discard cloudy, leaking, or expired bags to prevent contamination or error.
- Patient Monitoring
- Monitor for adverse reactions, fluid overload, or electrolyte imbalance.
- Frequency:
- Every 1–2 hours for stable patients
- Every 15–30 minutes for critical, pediatric, or nonverbal patients
- Promotes early detection of complications.
- Aseptic Technique
- Maintain strict aseptic technique when accessing IV ports or changing tubing.
- Clean ports with 2% chlorhexidine (preferred), 70% alcohol, or povidone-iodine and let dry.
- Prevents infection and contamination of IV system.
- Discontinuation of VAD
- Explain procedure to patient.
- Remove catheter carefully, apply pressure, and inspect tip for completeness.
- Document time, condition of site, and catheter integrity.
- Documentation
- Record all IV-related actions and assessments, including:
- Site condition and location
- Type/gauge of device
- Dressing and infusion rate
- Patient/family education
- Any interventions or unexpected findings
- Ensures legal protection, communication, and continuity of care.
- Record all IV-related actions and assessments, including:
Review Questions
References
Attribution 23.5 Sample Documentation – Nursing Skills – 2
Ignatavisius, D. D., Rebar, C. R., & Heimgartner, N. M. (2024). Concepts of infusion therapy. In J. H. Ingalls (Ed.), Medical-Surgical nursing: Concepts for clinical judgment and collaborative care (11 ed., pp. 285-315). Elsevier.
Infusion Nurses Society (INS). (2024). Infusion therapy standards of practice (9th ed.). Journal of Infusion Nursing, 47(Suppl. S1), S1–S285.
OpenStax (2025). Clinical Nursing Skills. Rice University. Creative Commons Attribution 4.0 International License Retrieved from https://openstax.org/books/clinical-nursing-skills/pages/13-3-intravenous-infusion
WisTech Open (2023). Nursing Skills (2nd edition).Creative Commons Attribution 4.0 International License Retrieved from https://wtcs.pressbooks.pub/nursingskills/chapter/23-7-sample-documentation/
Chapter opener: When prompted with “create a scenario for a female in Louisiana experiencing fluid volume deficit” the ChatGPT-generated text provided the above text. (OpenAI, 2025)
Chapter closer: When given a follow-up prompt of “continue the scenario for Mrs. Dupree and introduce IV therapy complications” the ChatGPT-generated text provided the above text. (OpenAI, 2025)
