8 Chapter Eight: Principles of Intravenous Medication Administration
Learning Objectives
- Discuss basic principles and techniques of intravenous medication. administration, including anatomy and physiology relevant to IV therapy.
- Identify and apply safety protocols to minimize risks associated with IV medication administration, including infection control and patient monitoring
- Demonstrated the ability to prepare and administer medications via intravenous routes, including calculating dosages and understanding drug interactions.
- Discuss the various types of IV equipment, including IV catheters, Infusion pumps, and administration sets.
- Assess patients before, during, and after IV medication administration to evaluate effectiveness and identify potential complications.
- Apply legal and ethical implications of IV medication in clinical practice.
Nursing in Louisiana
In the heart of Louisiana’s bayou, nestled among cypress trees, the air thick with humidity and the scent of magnolias, Ms. Robicheaux prepares for another busy day at the small backwoods clinic. The work may be familiar, but it demands precision and care. Today’s task: administering IV medication to patients who need hydration or antibiotics.
Her first patient is Mr. Henry LeBlanc, a burly fisherman in his late 60s, who arrives with a smile but a pale face. After suffering severe dehydration and infection from tainted shellfish, he needs fluids and antibiotics urgently. Ms. Robicheaux explains the process with calm assurance, reassuring him as she sets up the IV.
“Just relax, Mr. LeBlanc. We’ll have you feeling better soon,” she says as she carefully inserts the needle, checking for air bubbles and ensuring everything is sterile. As the fluids flow, she monitors his vitals and ensures everything is proceeding smoothly.
The storm outside intensifies, rain tapping against the windows, but inside the clinic, Ms. Robicheaux remains focused. She checks on each patient, making sure they receive the correct medication and dosage. Whether it’s antibiotics, pain management, or hydration, she knows the importance of safety and precision in IV therapy.
As the day winds down, she takes a moment to glance out the window. The bayou, shrouded in mist, offers a moment of peace. The clinic’s staff has worked together seamlessly, ensuring every patient receives the care they need. In her world, whether in the bayou or the busiest of cities, the principles remain the same—safety, precision, and patient care.
Introduction
Intravenous (IV) medication administration is a fundamental component of modern medical care, offering a quick and efficient way to deliver medications directly into the bloodstream. This method is especially crucial in situations where rapid therapeutic effects are needed, when oral medications are not suitable, or when patients cannot take medications by mouth due to illness or other factors. IV therapy involves more than just the insertion of a needle or catheter; it demands a thorough understanding of pharmacokinetics, patient physiology, and the technical aspects of fluid management. Administering IV medications requires adherence to specific principles designed to ensure patient safety, treatment effectiveness, and comfort. These principles are based on scientific research, established clinical standards, and professional guidelines that healthcare providers follow to minimize risks and enhance therapeutic outcomes.
Intravenous (IV) medication administration is a method of delivering fluids, medications, or nutrients directly into the bloodstream through a vein. This allows for rapid delivery of substances to the body, which can be critical in emergency situations, or when other routes (such as oral administration) are not effective or viable.
IV medication administration offers precise control over drug delivery and is commonly used in hospitals, clinics, and emergency settings. Medications delivered intravenously are absorbed quickly, resulting in immediate therapeutic effects. Common medications delivered via IV include analgesics, antibiotics, chemotherapy drugs, and electrolytes.
Types of IV Medication Administration
There are several methods for administering IV medications, which include:
Continuous IV Infusion
Continuous infusion refers to the administration of medications or fluids over an extended period, allowing for steady and controlled delivery to maintain therapeutic levels. This method is particularly critical in clinical scenarios that demand precise dosing and ongoing support. Common examples of therapies delivered via continuous infusion include parenteral nutrition (which provides essential nutrients to patients unable to eat), hydration fluids for maintaining fluid balance, and medications requiring stable plasma concentrations, such as dobutamine for heart failure or nitroprusside for hypertensive crises. Continuous infusions are especially valuable in critical care settings, where maintaining consistent drug levels can be life-saving. The Institute for Safe Medication Practices (ISMP) strongly recommends the use of Electronic Infusion Devices (EIDs) equipped with Dose Error Reduction Software (DERS) when administering high-alert medications. This technology helps reduce the risk of overdose or underdose by ensuring accuracy in infusion rates—critical for drugs like dobutamine or nitroprusside, which have narrow therapeutic windows and can cause serious adverse effects if not dosed correctly. It is essential that these devices are regularly calibrated, properly maintained, and carefully programmed according to institutional protocols to prevent discrepancies. Continuous infusions may run for several days or longer, depending on the patient’s needs, and require careful monitoring throughout their course (ISMP, 2017).
Intermittent IV Infusion
Intermittent infusion involves administering medication at set intervals, typically over a short period (30–60 minutes), using smaller volumes of fluid—commonly around (e.g. 50-100 mL). This approach is frequently used for medications such as antibiotics, which require periodic dosing to maintain efficacy. Intermittent infusions may be delivered using infusion pumps or gravity, employing techniques like IV piggyback (IVPB), simultaneous infusions, metered volume chambers, or primary administration sets. The IVPB method is widely used, where a secondary medication bag is connected to a primary IV line through a port with a check valve. The medication is infused via the secondary line, and upon completion, the primary IV fluid resumes its flow. This method allows multiple medications to be administered safely and efficiently without disconnecting the primary line, reducing the risk of infection and ensuring continuity of therapy (Infusion Nurses Society, 2021).
Advantages of Intermittent Infusions
- Optimized Drug Dosing & Safety: Intermittent infusions allow for targeted therapeutic levels without prolonged exposure, reducing the risk of toxicity—especially important for high-alert medications like vancomycin or aminoglycosides.
- Improved Patient Mobility & Comfort: With the growing focus on patient-centered care, intermittent infusions support mobility, which has been linked to shorter hospital stays and reduced risk of pressure injuries and blood clots.
- Integration with Smart Pumps: Modern infusion pumps with programmable dosing and safety checks minimize errors and make intermittent dosing more precise and safer than before.
- Decreased Risk of Line Infections: Compared to continuous infusions, intermittent therapy gives more opportunities to flush the IV line and assess the site, reducing the risk of catheter-associated infections.
- Cost-Efficient: Reduced fluid use and shorter infusion durations can lower resource use and costs, making it a favorable option in outpatient and resource.
Disadvantages of Intermittent IV Infusion
- Potential for Inconsistent Therapeutic Levels: Some medications may not maintain optimal plasma concentrations between doses, possibly reducing efficacy in critical care or infectious disease treatments.
- Increased IV Site Manipulation: Frequent connecting and disconnecting increases the risk of mechanical phlebitis, site contamination, or occlusion if aseptic technique is not strictly followed.
- Greater Demand on Nursing Workflow: Intermittent dosing requires more frequent checks, assessments, and administration times—challenging in understaffed or high-acuity units.
- Risk of Delayed Administration: In busy clinical settings, delays in timely administration may affect therapeutic outcomes, especially for time-dependent antibiotics.
- Not Ideal for Certain Drugs or Conditions: Some critical medications (e.g., vasopressors, sedatives) require continuous delivery to maintain steady physiological effects.
Nursing Fact
Intermittent IV infusion allows for scheduled administration of medications with flushes between doses, reducing the risk of fluid overload and improving patient mobility. It requires vigilant assessment of IV site patency and adherence to aseptic technique to minimize infection risk.
IV Push (Bolus) and IV Piggyback (IVPB)
An IV push (or bolus) involves administering a single, concentrated dose of medication directly into the bloodstream through a syringe over a short time, usually within minutes. This method allows for rapid drug action and is often used in emergency or acute care settings. It is imperative that nurses strictly adhere to the “eight rights” of medication administration—right patient, right medication, right dose, right time, right route, right documentation, right reason, and right response—as defined by the American Nurses Association (ANA), verifying them at least three times during the process to ensure patient safety. The IV piggyback (IVPB) method, on the other hand, administers a secondary medication through an existing primary IV line, most commonly for antibiotics or intermittent therapies, utilizing a secondary set that attaches above the primary infusion, ensuring efficient and safe delivery of adjunct treatments (ANA, 2020; INS, 2021).

Nursing Fact
IV push medications deliver a rapid dose directly into the bloodstream, providing immediate therapeutic effects. Nurses must always verify drug compatibility, push rate, and monitor the patient closely for adverse reactions during and after administration.
Advantages of IV Push Medications:
- Rapid Onset of Action: Delivers medication directly into the bloodstream, making it ideal for emergencies or when immediate effects are needed (e.g., pain relief, cardiac drugs).
- No Need for Large Volumes: Useful for fluid-restricted patients, as only a small volume is used compared to infusions.
- Efficient Administration: Quick and convenient for nurses—especially in high-acuity settings—requiring less equipment and time than continuous infusions.
Disadvantages of IV Push Medications:
- Higher Risk of Adverse Reactions: Rapid delivery can cause immediate side effects or toxicity if not administered correctly (e.g., too fast or without dilution).
- Requires Precise Technique and Knowledge: Must know correct rate, dilution, and compatibility—mistakes can lead to serious complications like tissue damage or cardiac effects.
- Limited Drug Compatibility: Some medications can’t be given IV push due to irritation, pH issues, or incompatibility with IV fluids.
Eight Routes of Medication Administration
- Right Patient: Confirm the correct patient using two patient identifiers as per agency policy (e.g., name and date of birth).
- Right Medication: Ensure that the correct medication is being administered and that it is appropriate for the patient’s condition. Understand the medication’s purpose and why it is being prescribed for this patient.
- Right Dose: Verify that the medication dose is appropriate based on the patient’s age, size, and clinical condition. Different conditions may require varying dosages, and pediatric doses are typically lower than adult doses. Be mindful of the medication’s side effects, peak, and onset of action. The peak refers to the time when the medication reaches its highest concentration in the bloodstream, while the onset is when the medication begins to take effect. Nurses must be aware of both to assess when the patient’s response to the medication will be observed.
- Right Route: Ensure that the route of administration is suitable for the patient’s current condition. Determine if the medication is compatible with IV push administration, whether it requires dilution (e.g., with normal saline), or if it needs reconstitution. Additionally, verify whether the medication can be administered through peripheral access or requires a central line for larger veins.
- Right Time: Administer the IV medication according to the prescribed schedule. Ensure that the rate of infusion and any required post-procedure saline flushes follow the manufacturer’s guidelines and drug references.
- Right Documentation: Always verify the accuracy and clarity of documentation before administering any medication. Ensure that all relevant details are correctly recorded.
- Right Reason: Confirm that the medication is being administered for the correct clinical reason. If the signs and symptoms no longer necessitate the prescribed medication, notify the prescribing provider.
- Right Response: After administering the IV push medication, assess the patient for expected therapeutic outcomes within the anticipated timeframe of the medication’s peak and onset. Additionally, monitor for any unexpected adverse effects. If the expected outcomes are not achieved or if adverse reactions occur, promptly notify the provider. By consistently adhering to these rights, nurses ensure safe and effective medication administration, contributing to positive patient outcomes and minimizing the risk of errors (www.ncbi.nlm.nih.gov).
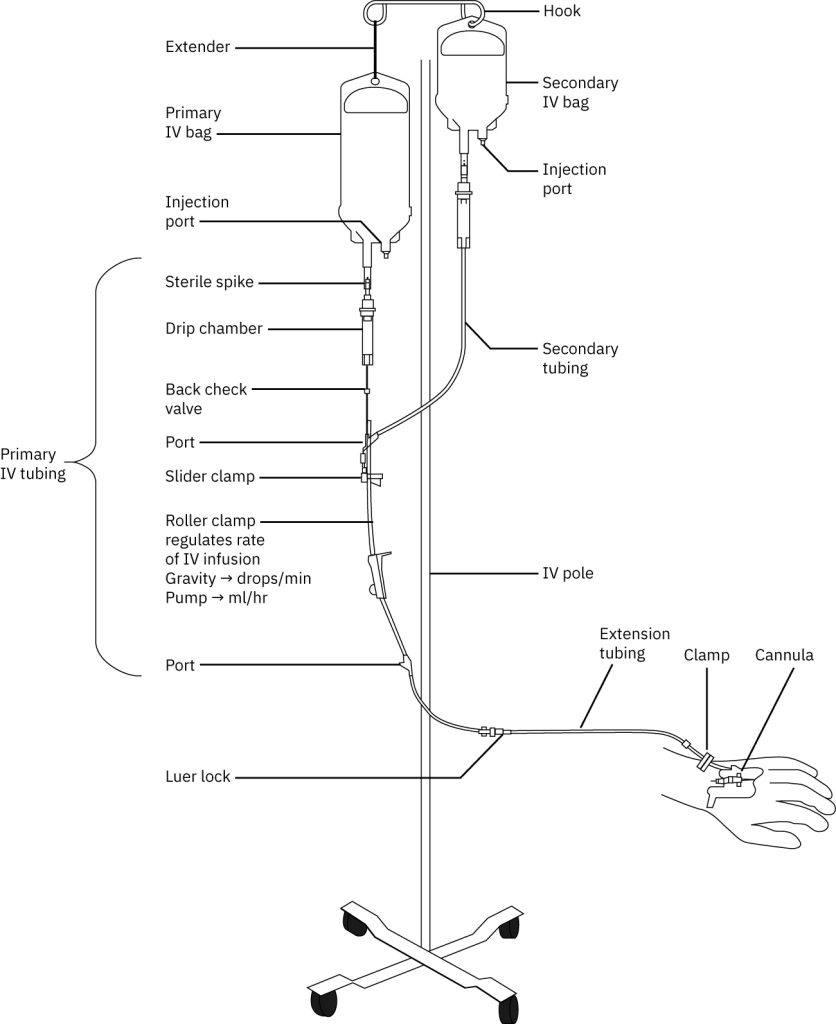
Components of an IV System
Medication administration typically requires several components:
- IV Catheter: A hollow needle or tube inserted into a vein.
- IV Fluid Bag: Holds the medication or fluid to be administered.
- IV Tubing: Connects the fluid bag to the IV catheter.
- Infusion Pump: A device that controls the rate at which the medication is infused.
Techniques for Safe Administration
- Sterility: To prevent infection, proper aseptic technique must be followed during setup and administration .
- Correct Medication and Dose: Ensure the medication is prescribed, the right dosage is confirmed, and the correct IV route is selected.
- Monitoring: Patients must be closely monitored for any adverse reactions or side effects, especially during the initial administration.
Complications and Risks
- Despite its benefits, IV medication administration poses risks such as infection from contaminated equipment, phlebitis (vein inflammation), extravasation (medication leakage into surrounding tissue causing damage), and air embolism (the introduction of air into the bloodstream, which can be life-threatening) (Smith & Jones, 2020).
Key considerations in IV medication administration include the flow rate, which must be carefully calculated based on the prescribed dosage and the patient’s condition to ensure effectiveness and minimize side effects, as well as patient factors such as age, weight, and comorbidities, which should be considered to tailor the treatment appropriately (Brown & Davis, 2019).
Pharmacokinetics
Pharmacokinetics is the study of how the body absorbs, distributes, metabolizes, and eliminates drugs. Understanding the anatomy and physiology of the relevant systems is essential for comprehending these processes.
- Absorption: Drugs are absorbed primarily in the small intestine due to its large surface area and rich blood supply. Factors such as the drug’s solubility, pH, and the presence of food can influence absorption. Drugs absorbed in the gastrointestinal tract first pass through the liver via the portal vein, where they may undergo first-pass metabolism, reducing their bioavailability Omics Online Publishing.
- Distribution: Once in the bloodstream, drugs are distributed throughout the body. The cardiovascular system, including the heart, arteries, veins, and capillaries, facilitates this process. Factors such as blood flow, tissue permeability, and the drug’s affinity for plasma proteins affect distribution. Lipophilic drugs tend to accumulate in fatty tissues, while hydrophilic drugs remain in aqueous compartments. The blood-brain barrier restricts the entry of certain substances into the central nervous system .DoveMedOmics Online Publishing
- Metabolism: Metabolism primarily occurs in the liver, where enzymes like cytochrome P450 facilitate chemical transformations of drugs. These transformations often make drugs more water-soluble and easier to excrete. Metabolism can be influenced by genetic factors, age, diet, and disease states. Some drugs may be converted into active or toxic metabolites .Omics Online PublishingScience Info
- Excretion: The kidneys play a vital role in filtering blood and excreting waste products, including drug metabolites. Drugs can also be eliminated through the liver (via bile), lungs, sweat, saliva, and even exhaled air in the case of volatile substances. Renal function and the characteristics of the drug, such as renal blood flow and glomerular filtration rate, influence excretion .
- Pharmacokinetic Principles: Key concepts include half-life (the time required for the plasma concentration of a drug to decrease by 50%), volume of distribution (the extent to which a drug is distributed throughout the body), and clearance (the rate at which a drug is removed from the body). These parameters are influenced by factors such as drug properties and individual patient characteristics .DoveMed
- A comprehensive understanding of these processes is essential for optimizing drug therapy and minimizing adverse effects.
Medication Safety Protocols
- Always verify the correct drug, dose, and route before administration. Confirm the drug name and dosage with the prescriber. When available, use barcode technology to ensure the correct medication and patient are matched. Confirm that the patient does not have allergies or contraindications to the prescribed IV medication (ismp.org).
- Always verify the patient’s identity using two identifiers (e.g., name, date of birth, or ID number) before administration. Ensure that the patient is in the right position and is comfortable during the procedure.
- Ensure that the medication has not expired. Look for any discoloration, particulates, or other signs of damage to the drug. Follow instructions on proper dilution of IV medications, as improper dilution can affect medication potency and safety. Clearly label the IV bag or syringe with the drug name, dose, concentration, and the time it was prepared (myamericannurse.com).
- Select an appropriate vein for IV access based on the type of medication being administered and the duration of therapy. Use the least invasive site whenever possible. Check for signs of infiltration, phlebitis, or other complications at the injection site. Use proper techniques to secure the IV catheter and minimize movement or dislodgement (ismp.org).
- Adhere to recommended infusion rates for the specific medication to avoid complications such as toxicity or adverse reactions. Monitor the patient for any immediate reactions during administration, including changes in vital signs, discomfort, or signs of an allergic reaction. Record the time, dosage, and any relevant patient observations (ismp.org).
- Observe for signs of an allergic reaction, side effects, or complications during and after IV medication administration. Depending on the medication, vital signs may need to be monitored before, during, and after administration. Provide the patient with appropriate post-administration care instructions, including signs and symptoms of possible adverse reactions (ismp.org).
- If a medication error occurs (e.g., wrong drug, wrong dose), follow institutional protocols to address the error, such as contacting the prescribing provider and the pharmacy. Document the error and the actions taken. Report it according to your healthcare facility’s incident reporting system to help prevent future errors(myamericannurse.com)
- Maintain strict aseptic technique when preparing and administering IV medications to prevent infections. Perform hand hygiene before and after administering IV medications, handling equipment, or touching the patient. Use sterile needles, syringes, and IV solutions (cdc.gov).
- Be prepared to recognize and respond to signs of severe adverse reactions like anaphylaxis or an overdose. When administering high-risk medications, have resuscitation equipment available, including epinephrine, oxygen, and defibrillators. Be aware of antidotes or reversal agents for medications that may cause toxic effects and ensure they are readily available.
- Staff should be trained regularly on the latest IV medication safety protocols, proper techniques, and drug updates. Inform patients about their treatment plan, potential side effects, and signs of complications to watch for. By adhering to these protocols, healthcare providers can ensure the safe and effective administration of IV medications, improve patient outcomes while minimizing the risk of complications (myamericannurse.com).
- Preparing and administering intravenous (IV) medications require strict adherence to established protocols to ensure patient safety and therapeutic efficacy. Here’s a comprehensive overview of the process, along with current resources:
- Confirm the medication order, patient identity, and any allergies.
- Accurately calculate the required dosage and infusion rate.
- Gather necessary supplies, including syringes, needles, IV bags, and appropriate diluents.
- Employ strict aseptic techniques to prevent contamination.
- Clearly label the medication with patient identifiers, medication name, dose, date, time, and your initials (ncbi.nlm.nih.gov)
Administration of IV Medications
- Examine the IV insertion site for signs of infection, infiltration, or phlebitis.
- If required, flush the IV line with a compatible solution to ensure patency.
- Depending on the medication, administer via IV push (bolus) or infusion.
- Continuously monitor the patient for adverse reactions during and after administration.
- Record all relevant details, including medication name, dose, time, route, and any patient responses.
Patient Assessment and Monitoring
Effective patient assessment and monitoring during intravenous (IV) medication administration are crucial for ensuring safety and therapeutic efficacy. Key guidelines include:
Pre-administration Assessment
- Patient Evaluation: Assess the patient’s medical history, allergies, and current condition to identify contraindications or potential interactions (ncbi.nlm.nih.gov)
- Medication Verification: Confirm the medication order, including the correct drug, dose, route, and timing. Ensure compatibility with other IV fluids or medications.
- IV Site Inspection: Examine the IV insertion site for signs of infection, phlebitis, or infiltration. Ensure the site is patent and properly secured (wtcs.pressbooks.pub)
Vital Signs: Obtain baseline vital signs to monitor for any changes during administration.Citation
During Administration
- Patient Education: Inform the patient about the medication, its purpose, and potential side effects. Encourage them to report any discomfort or unusual symptoms. (ncbi.nlm.nih.gov)
- Continuous Monitoring: Regularly assess the IV site for redness, swelling, or discomfort, which could indicate complications like infiltration or phlebitis.
- Rate of Administration: Administer the medication at the prescribed rate to prevent adverse effects. For certain medications, slow infusion rates may be necessary to avoid complications (wtcs.pressbooks.pub)
- Adverse Reaction Vigilance: Monitor for signs of allergic reactions or other side effects such as nausea, dizziness, or changes in heart rate or blood pressure
Post-administration Monitoring:
- IV Site Assessment: After administration, inspect the IV site for any signs of irritation, swelling, or hematoma. Flush site to ensure patency. Clean the area and apply a bandage if necessary.
- Vital Signs Reassessment: Monitor the patient’s vital signs for a period after the medication is administered, as some medications can have delayed effects.
- Documentation: Record all assessments, the time of medication administration, patient’s response, and any adverse reactions in the patient’s medical record (wtcs.pressbooks.pub)
- Patient Education (Post-Administration): Educate the patient about possible side effects that could occur after administration and when to seek help. Provide clear instructions for any required follow-up(ncbi.nlm.nih.gov) citation
Special Considerations:
- High-Alert Medications: For medications like chemotherapy agents or vasoactive drugs, additional precautions are necessary due to their potential for severe adverse effects (hospitals.vchca.org)
- Antibiotics: Monitor for signs of allergic reactions, especially after the first dose.citation
- Sedatives or Analgesics: Close monitoring of respiratory rate, level of consciousness, and oxygen saturation is critical.
- Anticoagulants: Monitor for signs of bleeding and ensure the patient is not at risk of hemorrhagic complications (hospitals.vchca.org)
By adhering to these guidelines, healthcare providers can enhance patient safety and optimize the therapeutic outcomes of IV medication administration.
Legal and Ethical Considerations
Administering intravenous (IV) medications in clinical practice involves significant legal and ethical considerations to ensure patient safety, uphold professional standards, and maintain trust in healthcare systems.
Legal Implications:
- Healthcare professionals must comply with established protocols and institutional guidelines when administering IV medications. Failure to do so can result in legal consequences, including malpractice claims. Accurate and thorough documentation of medication administration is essential. Inadequate records can lead to legal challenges, especially if adverse events occur. Obtaining informed consent is a legal requirement. Patients must be fully informed about the medication, its purpose, potential risks, and benefits before administration. Prompt reporting of medication errors is legally mandated in many jurisdictions. Failure to report can result in legal repercussions and compromise patient safety (pmc.ncbi.nlm.nih.gov).
Ethical Implications:
- Beneficence and Nonmaleficence: Healthcare providers are ethically obligated to act in the best interest of patients (beneficence) and avoid causing harm (nonmaleficence). This includes ensuring the correct medication and dosage are administered.
- Autonomy: Respecting patient autonomy involves providing information and obtaining consent for IV medication administration. Patients have the right to make informed decisions about their treatment.citation
- Justice: Ethically, healthcare providers must ensure equitable access to medications and avoid discrimination in treatment administration.
- Confidentiality: Maintaining patient confidentiality is an ethical duty. Information about medication administration should be shared only with authorized personnel karger.com
Key Takeaways
- Some cohort members prepared this as a bulleted list
