4.2 Basic Concepts
Open Resources for Nursing (Open RN)
Before learning how to use the nursing process, it is important to understand basic concepts concerning how critical thinking relates to nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing client care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[1] Using critical thinking means that nurses take extra steps to maintain client safety and don’t just “follow orders.” It also means the accuracy of client information is validated and plans for caring for clients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentric: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentric)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions.”[2] To make sound judgments about client care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience.[3]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, generalizing, and creating hypotheses based on specific information or incidents. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a client’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes clearer. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a client problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a client, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1.[4] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to act quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Example: A nurse assesses a client and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the client’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.

Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Deductive reasoning relies on a general statement or hypothesis – sometimes called a premise or standard – that is held to be true. The premise is used to reach a specific, logical conclusion. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about client care and solve problems.
Example: Based on research findings, hospital leaders determine clients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2).[5] The nurse further implements this policy by organizing care for clients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all clients regardless if they have difficulty sleeping or not.
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.”[6] The NCSBN administers the national licensure exam (NCLEX) that evaluates the decision-making ability of nursing graduates and sets a minimum standard for safe, competent nursing care by entry-level licensed nurses. The NCLEX uses the NCSBN Clinical Judgment Measurement Model (NCJMM) to measure clinical judgment.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.”[7]
Nursing Process
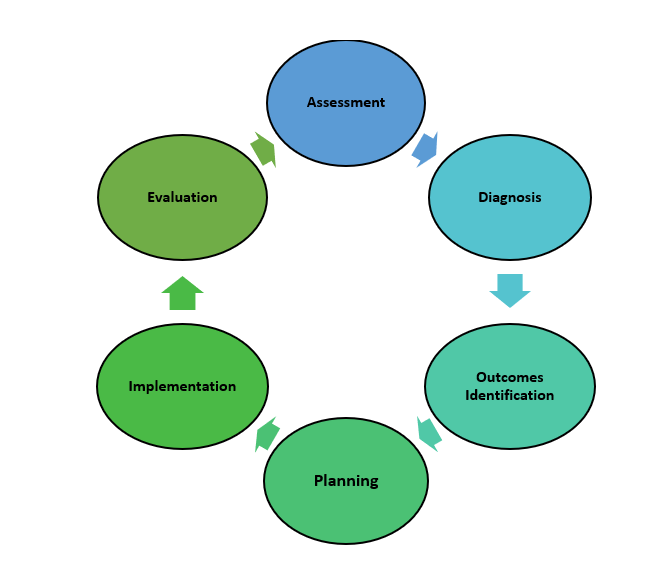
The nursing process is a critical thinking model based on a systematic approach to client-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing client care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses (RNs), regardless of role, population, specialty, and setting, are expected to perform competently.[8] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
The nursing process is a continuous, cyclical process that is constantly adapting to the client’s current health status. See Figure 4.3a[9] for an illustration of the nursing process.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[10] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized client in pain includes recognizing cues such as the client’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff.[11]
Licensed practical/vocational nurses (LPN/VNs) assist with gathering data according to their state’s scope of practice, but do not analyze data because this is outside their scope of practice. The “Assessment” component of the nursing process is further described in the “Assessment” section of this chapter.
Diagnosis
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[12] A nursing diagnosis is the nurse’s clinical judgment about the response from the client to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.[13]
Analyzing assessment data and formulating a nursing diagnosis is outside the scope of practice for LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Diagnosis” component of the nursing process is further described in the “Diagnosis” section of this chapter.
Outcome Identification
The “Outcome Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[14] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Outcome identification is outside the scope of practice of LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Outcome Identification” component of the nursing process is further described in the “Outcome Identification” section of this chapter.
Planning
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[15] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs in order to achieve their previously established goals and outcomes. Nursing interventions are planned and documented by the nurse in the client’s nursing care plan so that nurses, as well as other health professionals, can refer to it for continuity of care.[16]
The “Planning” component of the nursing process is further described in the “Planning” section of this chapter.
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific client using the nursing process. RNs create nursing care plans so that the care provided to the client across shifts is consistent among health care personnel. Some interventions can be delegated to LPN/VNs or trained Unlicensed Assistive Personnel (UAPs) with RN supervision.
Creating the nursing care plan is outside the scope of practice, and as such, the LPN/VNs do not perform this task, although they may contribute to it. Developing nursing care plans and implementing appropriate delegation are further discussed under the “Planning” and “Implementation of Interventions” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.”[17] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the client. Interventions are documented in the client’s electronic medical record as they are completed.[18] LPN/VNs implement interventions contained in the nursing care plan, provided they are within their scope of practice. The LPN/VN is responsible for documenting the interventions they perform in the client’s medical record.
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment.[19]
The “Implementation” component of the nursing process is further described in the “Implementation of Interventions” section of this chapter.
Evaluation
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[20] During evaluation, nurses reassess the client and compare the findings against established outcomes to determine the effectiveness of the interventions and overall nursing care plan. During this phase, RNs ask, “Were outcomes met? Are any modifications required for the nursing care plan?” Both the client’s status and the effectiveness of the nursing care plan are continuously evaluated and modified as needed.[21]
Evaluating and modifying the nursing care plan is outside the scope of practice of LPN/VNs, although they can assist in gathering assessment data to assist the RN in performing this step of the nursing process. The “Evaluation” component of the nursing process is further described in the “Evaluation” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, clients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality client care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a client’s health care problems
- Improves client safety
- Improves client satisfaction
- Identifies a client’s goals and strategies to attain them
- Increases the likelihood of achieving positive client outcomes
- Saves time, energy, and frustration by creating a care plan that is accessible to all staff caring for a client
By using these components of the nursing process as a critical thinking model, nurses plan outcomes and interventions that are customized to the client’s specific needs, ensure the interventions are evidence-based, and evaluate the effectiveness of interventions in meeting the client’s needs.
NCSBN Clinical Judgment Measurement Model
The NCSBN Clinical Judgment Measurement Model (NCJMM) complements the nursing process, but it is a model that assesses an NCLEX candidate’s clinical judgment. Terminology used by this model includes recognize cues, analyze cues, prioritize hypotheses, generate solutions, take action, and evaluate outcomes. See Figure 4.3b[22] and Table 4.2 for comparisons of NCJMM terms and the nursing process.[23],[24],[25]
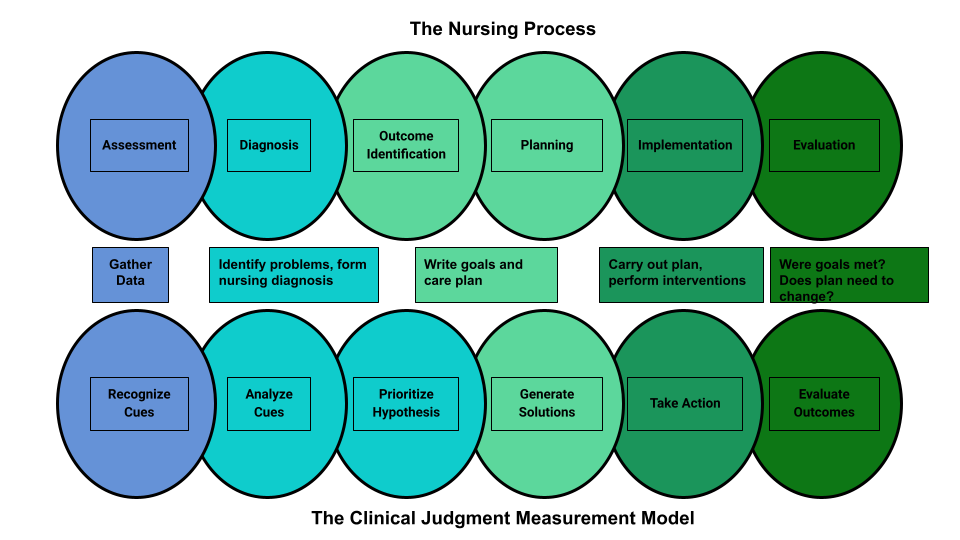
Table 4.2 Comparison of the NCJMM to the Nursing Process
| NCSBN Clinical Judgment Skill | Description | Corresponding Step of the Nursing Process |
|---|---|---|
| Recognize Cues | What data is clinically significant?
Determining what client findings are significant, most important, and of immediate concern to the nurse (i.e., identifying “relevant cues”). |
Assessment |
| Analyze Cues | What does the data mean?
Analyzing data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for this client at this time according to their age, development, and clinical status. Making a clinical judgment concerning the client’s “human response to health conditions/life processes, or a vulnerability for that response”; also referred to as “forming a hypothesis.” |
Diagnosis
(Analysis of Data) |
| Prioritize Hypotheses | What hypotheses should receive priority attention?
Ranking client conditions and problems according to urgency, complexity, and time. |
Planning |
| Generate Solutions | What should be done?
Planning individualized interventions that meet the desired outcomes for the client; may include gathering additional assessment data. |
Planning |
| Take Action | What will I do now?
Implementing interventions that are safe and most appropriate for the client’s current priority conditions and problems. |
Implementation |
| Evaluate Outcomes | Did the interventions work?
Comparing actual client outcomes with desired client outcomes to determine effectiveness of care and making appropriate revisions to the nursing care plan. |
Evaluation |
Learning activities are incorporated throughout this book to help students practice answering NCLEX Next Generation-style test questions.
Review Scenario A in the following box for an example of a nurse using the nursing process and NCJMM skills while providing client care.
Client Scenario A: Using the Nursing Process[26]

A nurse is caring for a hospitalized client with a medical diagnosis of heart failure who has a prescription to receive furosemide 80mg IV every morning. The nurse uses critical thinking according to the nursing process and the NCJMM before administering the prescribed medication:
Assessment/Recognize Cues: During the morning assessment, the nurse notes that the client has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F.
Diagnosis/Analyze Cues: The nurse reviews the medical record for the client’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s.
Planning/Prioritize Hypothesis: The nurse recognizes cues (assessment data) that form a pattern related to fluid imbalance and hypothesizes that the client may be dehydrated.
Planning/Generate Solutions: The nurse gathers additional information and notes the client’s weight has decreased four pounds since yesterday. The nurse talks with the client and validates the hypothesis when the client reports that their mouth feels like cotton, and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the client with the nursing diagnosis Fluid Volume Deficit and plans interventions for reestablishing fluid balance.
Implementation/Take Action: The nurse withholds the administration of IV furosemide and contacts the health care provider to discuss the client’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitors hydration status.
Evaluation/Evaluate Outcomes: By the end of the shift, the nurse evaluates the client status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the client, recognizes and analyzes cues, creates a hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates outcomes. While performing these steps, the nurse promotes client safety by contacting the provider before administering a medication that could cause harm to the client at this time.
Holistic Nursing Care
Using the nursing process and clinical judgment while implementing evidence-based practices is referred to as the “science of nursing.” Before getting deeper into the science of nursing in the remainder of this chapter, it is important to discuss the “art of nursing” that relies on holistic care provided in a compassionate and caring manner using the nursing process.
The American Nurses Association (ANA) defines nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”[27]
The ANA further describes nursing as a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.”[28]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a client and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.”[29] Successful use of the nursing process requires the development of a care relationship with the client. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the client and family. Assessing and caring for the whole person considers the physical, mental, emotional, and spiritual aspects of being a human being.[30] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, using therapeutic touch, and providing emotional support while respecting their cultural beliefs associated with caring behaviors.[31] See Figure 4.4[32] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their clients while creating a healing environment.[33]

Now that we have discussed basic concepts related to the nursing process, as well as the science and art of nursing, let’s look more deeply at each component of the nursing process in the following sections.
Media Attributions
- 3550755709_d8be7ba08b_b
- 2786901401_78efa24a0a_k
- pasted image 0
- Nursing Process and NCJMM
- hospice-1793998_1280
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221. doi: 10.1097/01.NEP.0000000000000669. PMID: 32569111. https://pubmed.ncbi.nlm.nih.gov/32569111/ ↵
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15(7), 37-39. https://www.myamericannurse.com/nurse-preceptors-and-new-graduate-success/ ↵
- “The Detective” by paurian is licensed under CC BY 2.0 ↵
- “In the Quiet Zone…” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment measurement model. https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “The Nursing Process” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- “Nursing Process and NCJMM” by Tami Davis is licensed under CC BY 4.0 ↵
- NCSBN (n.d.) NCSBN Clinical Judgment Measurement Model. https://www.ncsbn.org/14798.htm ↵
- Ignativicius, V., & Silvestri, L. (2022). Preparing for the Next-Generation NCLEX (NGN): A “how-to” step-by-step faculty resource manual. Elsevier. https://evolve.elsevier.com/education/wp-content/uploads/sites/2/NGN_FacultyGuide_Final.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7, 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “hospice-1793998_1280.jpg” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN). https://www.watsoncaringscience.org/jean-bio/ ↵
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.
A type of reasoning that involves forming generalizations based on specific incidents.
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
A judgment formed from a set of facts, cues, and observations.
A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies, theories, clinical expertise, health care resources, and patient preferences and values.
An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
Individual, family, or group which includes significant others and populations.
Specific documentation of the planning and delivery of nursing care that is required by the Joint Commission.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.
Defined as, "Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family.
Developing a relationship of mutual trust and understanding.

