4.3 Aseptic Technique
Ernstmeyer & Christman - Open Resources for Nursing (Open RN)
In addition to using standard precautions and transmission-based precautions, aseptic technique (also called medical asepsis) is the purposeful reduction of pathogens to prevent the transfer of microorganisms from one person or object to another during a medical procedure. For example, a nurse administering parenteral medication or performing urinary catheterization uses aseptic technique. When performed properly, aseptic technique prevents contamination and transfer of pathogens to the patient from caregiver hands, surfaces, and equipment during routine care or procedures. The word “aseptic” literally means an absence of disease-causing microbes and pathogens. In the clinical setting, aseptic technique refers to the purposeful prevention of microbe contamination from one person or object to another. These potentially infectious, microscopic organisms can be present in the environment, on an instrument, in liquids, on skin surfaces, or within a wound.
There is often misunderstanding between the terms aseptic technique and sterile technique in the health care setting. Both asepsis and sterility are closely related, and the shared concept between the two terms is removal of harmful microorganisms that can cause infection. In the most simplistic terms, asepsis is creating a protective barrier from pathogens, whereas sterile technique is a purposeful attack on microorganisms. Sterile technique (also called surgical asepsis) seeks to eliminate every potential microorganism in and around a sterile field while also maintaining objects as free from microorganisms as possible. It is the standard of care for surgical procedures, invasive wound management, and central line care. Sterile technique requires a combination of meticulous hand washing, creation of a sterile field, using long-lasting antimicrobial cleansing agents such as betadine, donning sterile gloves, and using sterile devices and instruments.
Principles of Aseptic Non-Touch Technique
Aseptic non-touch technique (ANTT) is the most commonly used aseptic technique framework in the health care setting and is considered a global standard. There are two types of ANTT: surgical-ANTT (sterile technique) and standard-ANTT.
Aseptic non-touch technique starts with a few concepts that must be understood before it can be applied. For all invasive procedures, the “ANTT-approach” identifies key parts and key sites throughout the preparation and implementation of the procedure. A key part is any sterile part of equipment used during an aseptic procedure, such as needle hubs, syringe tips, needles, and dressings. A key site is any nonintact skin, potential insertion site, or access site used for medical devices connected to the patients. Examples of key sites include open wounds and insertion sites for intravenous (IV) devices and urinary catheters.
ANTT includes four underlying principles to keep in mind while performing invasive procedures:
- Always wash hands effectively.
- Never contaminate key parts.
- Touch non-key parts with confidence.
- Take appropriate infective precautions.
Preparing and Preventing Infections Using Aseptic Technique
When planning for any procedure, careful thought and preparation of many infection control factors must be considered beforehand. While keeping standard precautions in mind, identify anticipated key sites and key parts to the procedure. Consider the degree to which the environment must be managed to reduce the risk of infection, including the expected degree of contamination and hazardous exposure to the clinician. Finally, review the expected equipment needed to perform the procedure and the level of key part or key site handling. See Table 4.3 for an outline of infection control measures when performing a procedure.
Table 4.3 Infection Control Measures When Performing Procedures
| Infection Control Measure | Key Considerations | Examples |
|---|---|---|
| Environmental control |
|
|
| Hand hygiene |
|
|
| Personal protective equipment (PPE) |
|
|
| Aseptic field management | Determine level of aseptic field needed and how it will be managed before the procedure begins:
|
General aseptic field:
IV irrigation Dry dressing changes Critical aseptic field: Urinary catheter placement Central line dressing change Sterile dressing change |
| Non-touch technique |
|
|
| Sequencing |
|
|
Use of Gloves and Sterile Gloves
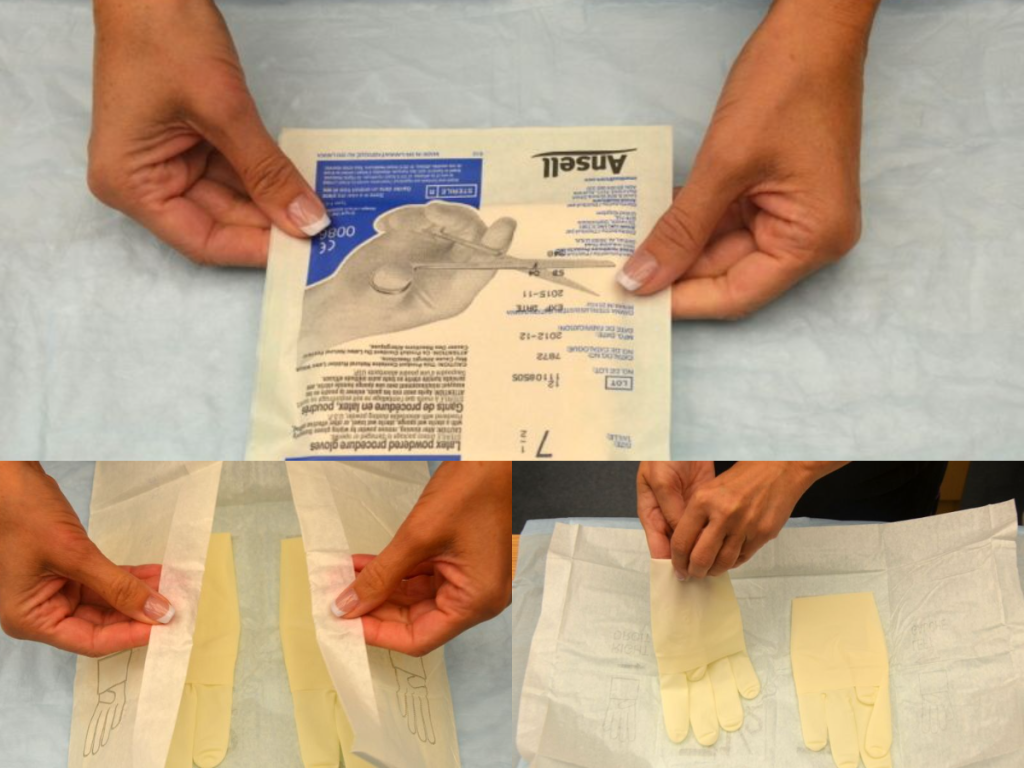
There are two different levels of medical-grade gloves available to health care providers: clean (exam) gloves and sterile (surgical) gloves. Generally speaking, clean gloves are used whenever there is a risk of contact with body fluids or contaminated surfaces or objects. Examples include starting an intravenous access device or emptying a urinary catheter collection bag. Alternatively, sterile gloves meet FDA requirements for sterilization and are used for invasive procedures or when contact with a sterile site, tissue, or body cavity is anticipated. Sterile gloves are used in these instances to prevent transient flora and reduce resident flora contamination during a procedure, thus preventing the introduction of pathogens. For example, sterile gloves are required when performing central line dressing changes, insertion of urinary catheters, and during invasive surgical procedures. See Figure 4.15[1] for images of a nurse opening and removing sterile gloves from packaging.
See the “Checklist for Applying and Removing Sterile Gloves” for details on how to apply sterile gloves.
Applying Sterile Gloves on YouTube[2]
Media Attributions
- download
- “Book-pictures-2015-199-001-300x241.jpg,” “Book-pictures-2015-215.jpg,” and “Book-pictures-2015-219.jpg” by British Columbia Institute of Technology are licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/sterile-gloving/ ↵
- RegisteredNurseRN. (2017, April 28). Sterile gloving nursing technique | Don/donning sterile gloves tips. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/lumZOF-METc ↵
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes." The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer's response and other indicators. The plan is documented using standardized language or terminology.[1]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client's medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[2] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the "Outcome Identification" section for a illustration of how the Planning phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[3]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative.
Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing intervention is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[4] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[5] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client's overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[6]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist" in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[7] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[8]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[9] for an image of a standardized care plan.
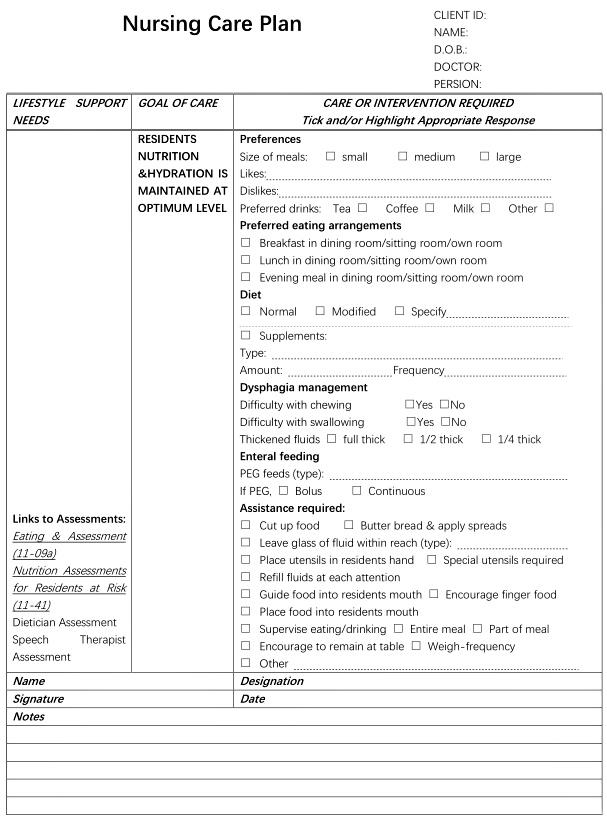
Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
ADOPIE: An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. (Chapter 4.2)
Art of nursing: Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.[10] (Chapter 4.2)
At-risk populations: Groups of people who share a sociodemographic characteristics, health/family history, stages of growth/development, exposure to certain events/experiences that cause each member to be susceptible to a particular human response. These characteristics are not modifiable by independent nursing interventions.[11](Chapter 4.4)
Associated conditions: Medical diagnoses, diagnostic/surgical procedures, medical/surgical devices, or pharmaceutical preparations that are not modifiable by independent nursing intervnetions.[12] (Chapter 4.4)
Care relationship: A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the client and family.[13] (Chapter 4.2)
Client: Individual, family, or group, which includes significant others and populations.[14] (Chapter 4.2)
Clinical judgment: The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.[15] (Chapter 4.2)
Clinical reasoning: A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions. [16] (Chapter 4.2)
Clustering data: Grouping data into similar domains or patterns. (Chapter 4.4)
Collaborative nursing interventions: Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP). (Chapter 4.6)
Coordination of care: While implementing interventions during the nursing process, includes competencies such as organizing the components of the plan with input from the health care consumer, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team.[17] (Chapter 4.7)
Critical thinking: Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.[18] (Chapter 4.2)
Cues: Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder. (Chapter 4.2)
Deductive reasoning: “Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion. (Chapter 4.2)
Defining characteristics: Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the client/family tells us), touched, or smelled.[19] (Chapter 4.4)
Delegation: The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel while retaining accountability for the outcome.[20] (Chapter 4.7)
Dependent nursing interventions: Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant. (Chapter 4.6)
Direct care: Interventions that are carried out by having personal contact with a client. (Chapter 4.6)
Electronic Medical Record (EMR): An electronic version of the client’s medical record. (Chapter 4.3)
Evidence-Based Practice (EBP): A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.[21] (Chapter 4.2)
Expected outcomes: Statements of measurable action for the client within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame. (Chapter 4.5)
Functional Health Patterns: An evidence-based assessment framework for identifying client problems and risks during the assessment phase of the nursing process. (Chapter 4.4)
Generalization: A judgment formed from a set of facts, cues, and observations. (Chapter 4.2)
Goals: Broad statements of purpose that describe the aim of nursing care. (Chapter 4.5)
Health promotion-wellness nursing diagnosis: A clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential. (Chapter 4.4)
Health teaching and health promotion: Employing strategies to teach and promote health and wellness.[22] (Chapter 4.7)
Hypothesis: A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. (Chapter 4.2)
Independent nursing interventions: Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else. (Chapter 4.6)
Indirect care: Interventions performed by the nurse in a setting other than directly with the client. An example of indirect care is creating a nursing care plan. (Chapter 4.6)
Inductive reasoning: A type of reasoning that involves forming generalizations based on specific incidents. (Chapter 4.2)
Inference: Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations. (Chapter 4.3)
Licensed Practical Nurses or Licensed Vocational Nurses (LPNs/LVNs): Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act. (Chapter 4.3)
Maslow’s Hierarchy of Needs: A theory used to prioritize the most urgent client needs to address first. The bottom levels of the pyramid represent the most important physiological needs intertwined with safety. (Chapter 4.4)
Medical diagnosis: A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual. (Chapter 4.3)
Nursing: Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.[23] (Chapter 4.2)
Nursing care plan: Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission. (Chapter 4.2)
Nursing diagnosis: A clinical judgment concerning a human response to health conditions/life processes, or susceptibility to that response, by an individual, caregiver, family, group, or community. (Chapter 4.4)
Nursing interventions: Evidence-based actions that the nurse performs to achieve client outcomes. (Chapter 4.6)
Nursing process: A systematic approach to client-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.” (Chapter 4.1)
Objective data: Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data. (Chapter 4.3)
Order: An intervention, remedy or treatment as directed by an authorized primary health care provider.[24] (Chapter 4.6)
Outcome: A measurable behavior demonstrated by the client's response to nursing interventions.[25] (Chapter 4.5)
PES format: The format of a nursing diagnosis statement that includes:
- Problem (P) - statement of the client problem (i.e., the nursing diagnosis)
- Etiology (E) - related factors (etiology) contributing to the cause of the nursing diagnosis
- Signs and Symptoms (S) - defining characteristics manifested by the client of that nursing diagnosis (Chapter 4.4)
Physical examination: A systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. (Chapter 4.3)
Prescription: Intervention as it relates to medication specifically as directed by an authorized primary health care provider.[26] (Chapter 4.6)
Primary data: Information collected from the client. (Chapter 4.3)
Primary health care provider: Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client.[27] (Chapter 4.6)
Prioritization: The skillful process of deciding which actions to complete first for client safety and optimal client outcomes. (Chapter 4.4)
Problem-focused nursing diagnosis: A clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community. (Chapter 4.4)
Quality improvement: The “combined and unceasing efforts of everyone -- health care professionals, clients and their families, researchers, payers, planners, and educators -- to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[28] (Chapter 4.7)
Rapport: Developing a relationship of mutual trust and understanding. (Chapter 4.2)
Registered Nurse (RN): A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing. (Chapter 4.3)
Related factors: The underlying cause (etiology) of a nursing diagnosis. (Chapter 4.4)
Risk nursing diagnosis: A clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes. (Chapter 4.4)
Secondary data: Information collected from sources other than the client. (Chapter 4.3)
Subjective data: Data that the client or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The client appears anxious.” (Chapter 4.3)
Syndrome nursing diagnosis: A clinical judgment concerning a specific cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. (Chapter 4.4)
Unlicensed Assistive Personnel (UAP): Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated.[29] (Chapter 4.3)
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[30]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14[31] for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[32] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[33]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[34] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[35]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[36] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The nurse must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The nurse cannot delegate responsibilities requiring clinical judgment.[37]
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[38] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[39] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[40]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14[41] for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[42] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[43]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[44] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[45]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[46] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[47] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[48]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[49] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[50] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).

