Infancy

Diet and nutrition have a major impact on a child’s development from infancy into the adolescent years. A healthy diet not only affects growth, but also immunity, intellectual capabilities, and emotional well-being. One of the most important jobs of parenting is making sure that children receive an adequate amount of needed nutrients to provide a strong foundation for the rest of their lives.
Most expectant mothers begin thinking about how they will feed their baby early in their pregnancy. Therefore, it is important to offer breastfeeding education and support starting with the first prenatal appointment.
How long should infants be breastfed?
Exclusive breastfeeding for about the first six months is recommended. The Dietary Guidelines for Americans recommends continued breastfeeding while introducing appropriate complementary foods until children are 12 months or older. The American Academy of Pediatrics and the World Health Organization recommend continued breastfeeding along with introducing appropriate complementary foods for up to 2 years or longer.[1]
Support from family members, especially the baby’s father and grandmother, plus friends, employers, and others can greatly help with both the decision-making process during pregnancy and the beginning and maintenance of breastfeeding after the baby’s birth. U.S. data show that about 84 percent of infants born in 2017 were ever fed human milk, with only 25 percent fed human milk exclusively through age 6 months, and 35 percent continuing to be fed any human milk at age 12 months. Nearly one-quarter of infants were fed some human milk beyond age 12 months, with about 15 percent of toddlers being fed human milk at age 18 months.[2]
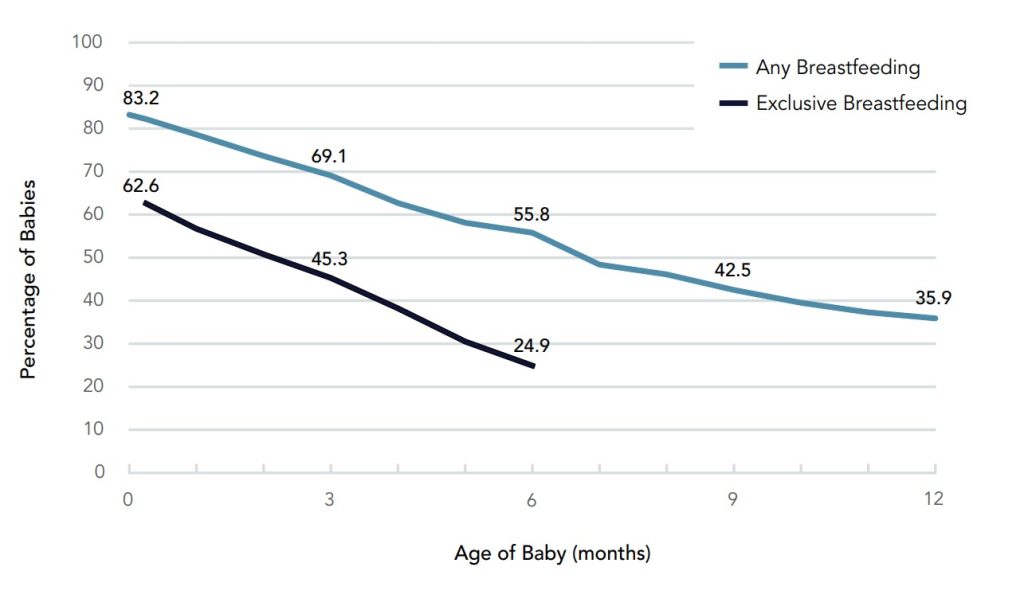
(Source: Centers for Disease Control and Prevention, Public Domain)
The approval and assistance of family members, friends, employers, health-care providers, and policymakers can make an enormous difference and provide the needed promotion and support for mothers who wish to breastfeed their children. Education about breastfeeding typically begins with healthcare providers. During prenatal care and often soon after a woman has given birth, doctors, nurses, and other clinicians can explain the benefits of breastfeeding and describe the proper technique. Nearly all births in the United States and Canada occur in hospital settings, and hospital practices in labor, delivery, postpartum care, and discharge planning can inform and support women who want to breastfeed. Once a new mother has left the hospital for home, she needs access to a trained individual who can provide consistent information. International Board Certified Lactation Consultants (IBCLCs) are health-care professionals (often a registered nurse or registered dietitian) certified in breastfeeding management that work with new mothers to solve problems and educate families about the benefits of this practice. Research shows that breastfeeding rates are higher among women who had infants in hospitals that make IBCLCs available to new mothers, rather than those who gave birth in institutions without these professionals on staff.[3]
Other important practices for maternity hospitals to support breastfeeding are summarized in the Ten Steps to Successful Breastfeeding, launched jointly by the WHO and UNICEF.[4] These recommended practices include: helping mothers initiate breastfeeding within one hour of birth; keeping mothers and babies together (rooming in); encouraging breastfeeding on demand, and giving breastfed infants no food or drink other than breast milk, unless medically indicated.
In addition, spouses, partners, and other family members can play critical roles in helping a pregnant woman decide to breastfeed and assisting with feeding after the baby is born. Employment can also factor into a woman’s decision to breastfeed or her ability to maintain the practice. Employed mothers have been less likely to initiate breastfeeding and tend to breastfeed for a shorter period of time than new mothers who are not employed or who have lengthy maternity leaves. In 2010, in the United States, the passage of the Affordable Care Act (ACA) required most employers to provide accommodations within the workplace for new mothers to pump breast milk. This law requires a private and clean space within the workplace, other than a restroom, along with adequate break time for a woman to express milk.[5] It also requires health insurance to cover certain breastfeeding services and supplies, such as a breast pump.
Louisiana state breastfeeding support resources are many. It is easy to find local breastfeeding support, including lactation consultants, WIC clinics, community breastfeeding support groups and educators, and physicians, at LABreastfeedingSupport.org, or by calling the Partners for Healthy Babies line at 1-800-251-BABY (2229).[6]
Members of a community can also promote and support breastfeeding. New mothers can join peer counseling groups or turn to other women within their community who have previous experience with breastfeeding. In addition, community-based programs can provide education and support. The US Department of Agriculture’s Women, Infants, and Children program provides information on breastfeeding and professional and peer support for women and their babies from low-income families. Launched in 2004, the Loving Support program combines peer counseling with breastfeeding promotion efforts to increase duration rates across the United States. La Leche League is an international program that provides mother-to-mother support, encouragement, and education about breastfeeding for women worldwide. Visit the La Leche League web site for more information (opens in a new window).
One of the primary goals of the Louisiana WIC program is to improve infants’ health status by encouraging WIC mothers to breastfeed their infants. Since its beginning in 1974, the WIC program continues to promote breastfeeding as the optimal feeding choice for most infants.
The Louisiana WIC Program provides:
- Breastfeeding help and support at WIC clinics
- Prenatal breastfeeding education support
- Individual breastfeeding education for participants
- Group breastfeeding education for participants
- Healthy WIC Food Packages
- Breastfeeding Peer Counselor Program
- Breast pump support – Free hospital-grade pumps and personal electric pumps
- Certified Lactation Consultants
- Partners for Health Baby Support Line 1-800-251-BABY
- Lactation rooms at most WIC sites
- Louisiana Women, Infants, and Children (WIC) program continues to provide pumps to eligible participants through the LA WIC Breast Pump Program.
Everyday Connection

Louisiana mandates that the state provide several accommodations within the workplace for new mothers. All employers are required to allow breastfeeding mothers adequate break time to pump or nurse in a location other than a bathroom. Louisiana Breastfeeding legislation supports breastfeeding and prohibits discriminatory practices.[7]
A. Legislative findings and declarations.
(1) The Legislature of Louisiana hereby finds that the surgeon general of the United States recommends that babies from birth to one year of age be breastfed, unless medically contraindicated, for the babies to attain an optimal healthy start in life, but that despite that recommendation, statistics reveal a declining percentage of mothers who are now choosing to breastfeed their babies, and nearly half of all new mothers are choosing formula over breastfeeding before they even leave the hospital.
(2) The legislature further finds that breast milk provides better nutrition and more immunity to disease, is easier for babies to digest, and may raise a baby’s intelligence quotient, but that the social constraints of modern society work against the choice of breastfeeding and lead new mothers with demanding time schedules to opt for formula feeding for reasons such as embarrassment and the fear of social ostracism or criminal prosecution.
(3) The legislature does hereby declare that the promotion of family values and infant health demands that our society put an end to the vicious cycle of embarrassment and ignorance that constricts women and men alike on the subject of breastfeeding, and that in a genuine effort to promote family values, our society should encourage public acceptance of this most basic act of nurture between mother and baby and should take appropriate steps to ensure that no mother is made to feel incriminated or socially ostracized for breastfeeding her baby.
B. Right to breastfeed. Notwithstanding any other provision of law to the contrary, a mother may breastfeed her baby in any place of public accommodation, resort, or amusement.
C. “Discriminatory practice in connection with public accommodations” to include a discriminatory practice against a mother breastfeeding her baby. Any direct or indirect act or practice of exclusion, distinction, restriction, segregation, limitation, refusal, denial, or any other act or practice of differentiation or preference in the treatment of a mother breastfeeding her baby shall be a “discriminatory practice in connection with public accommodations” for this Chapter.
D. Breastfeeding; discriminatory practices prohibited. It is a discriminatory practice in connection with public accommodations for a person to deny an individual the full and equal enjoyment of the goods, services, facilities, privileges, advantages, and accommodations of a place of public accommodation, resort, or amusement, as defined in this Chapter, because the individual is a mother breastfeeding her baby. This discriminatory practice in connection with public accommodations is prohibited.
E. Breastfeeding is not a violation of the law. A mother breastfeeding her baby in any location, public or private, where the mother is otherwise authorized to be, shall not be deemed to violate R.S. 14:106 or any other law provision.
Although breastfeeding should be recommended and encouraged for almost all new mothers, it is important to remember that the decision to breastfeed is a personal choice, and women should not be made to feel guilty if they cannot, or choose not, to breastfeed their infants. In some rare cases, a woman is unable to breastfeed, or it is not in the baby’s best interest, for example, if the baby has galactosemia, an inborn error of metabolism.
Parents’ Nutritional choices, such as the decision to breastfeed or bottle-feed, affect early childhood development and a child’s health and wellness later in life. Therefore, promoting and supporting the best practices for the well-being of infants and mothers alike is imperative.
Infancy (Birth to Age One)

Several significant physiological changes occur during infancy. The trunk of the body grows faster than the arms and legs, while the head becomes less prominent than the limbs. Organs and organ systems grow at a rapid rate. Also, during this period, countless synapse pathways to link brain neurons are reinforced while others are trimmed back in the brain. Two soft spots on the baby’s skull, known as fontanels, allow the skull to accommodate rapid brain growth. The posterior fontanel closes first, by the age of eight weeks. The anterior fontanel closes about a year later, at eighteen months on average. Developmental milestones include sitting up without support, learning to walk, teething, and vocalizing, among many others. All of these changes require adequate nutrition to ensure development at the appropriate rate.[8].

The average weight of a newborn in the United States in the past decade is between 5 pounds, 8 ounces (2,500 grams) and 8 pounds, 13 ounces (3,850 grams). Maternal factors that can influence the weight of a newborn are health, nutrition during pregnancy, intervals between pregnancies, use of substances including tobacco, nicotine, narcotics, and alcohol, gestational diabetes, and the size of both parents. The newborn will initially lose weight—up to 10 percent of their birth weight—in the first 3 days after birth. They are expected to regain their birth weight by 2 weeks of life.[9]

Healthy infants grow steadily but not always at an even pace. For example, during the first year of life, height increases by 50 percent while weight triples. Physicians and other health professionals use growth charts to track a baby’s development. Because infants cannot stand, length is used instead of height to determine the rate of a child’s growth. Other necessary developmental measurements include head circumference and weight. All of these must be tracked and compared against standard infant age measurements.
In the US, the WHO growth charts are used to monitor the growth of infants and toddlers from birth to 24 months. These standards represent optimal growth for children at this age and allow tracking growth trends over time through percentile rankings. Growth charts may warn that a child has a medical problem or is malnourished. Growth that is too rapid can increase the risk of being overweight and obese in childhood and later in life. Insufficient weight or height gain during infancy may indicate a condition known as failure to thrive (FTT), characterized by poor growth. FTT can happen at any age, but in infancy, it typically occurs after six months. Some causes include poverty, lack of food, inappropriate foods, and excessive fruit juice intake.
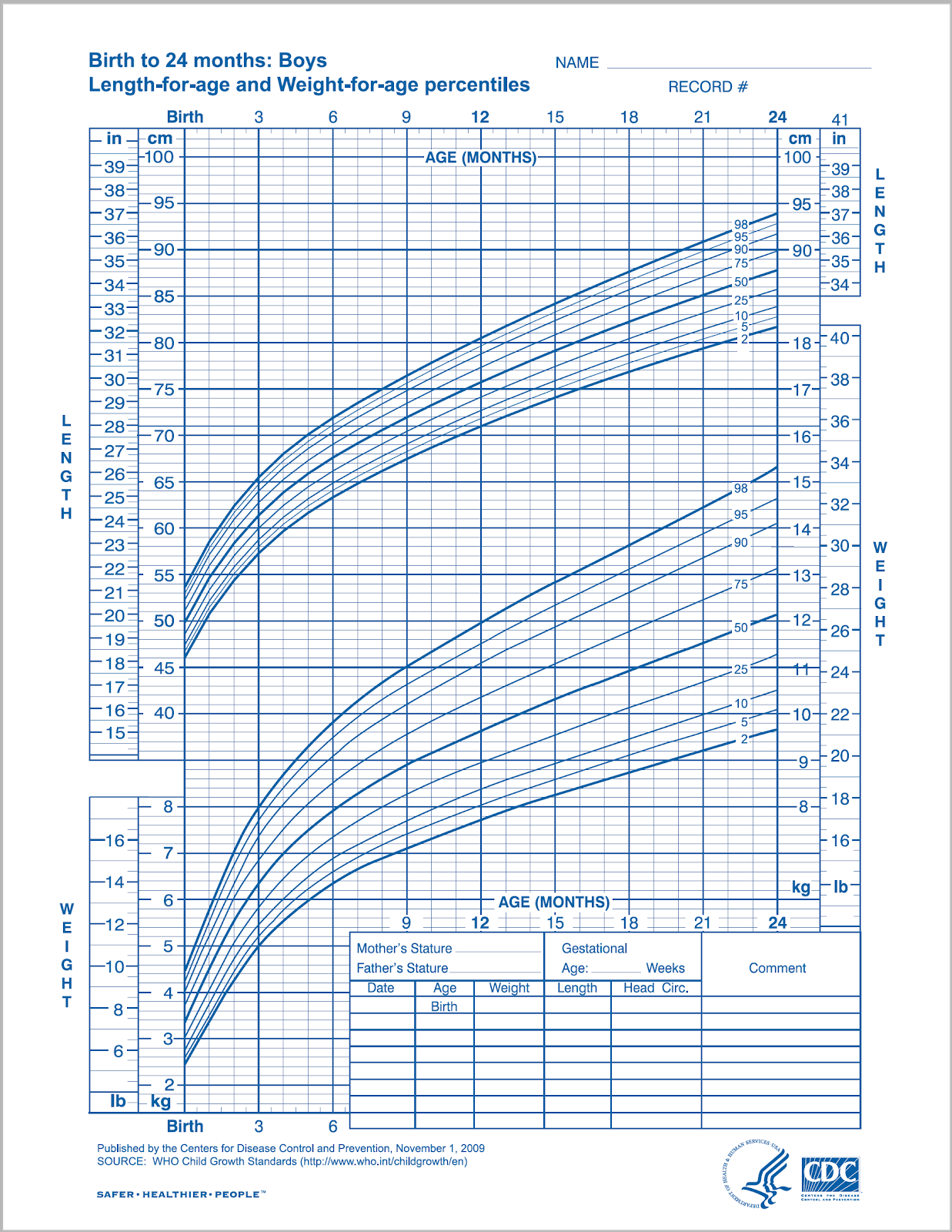
(Source: Centers for Disease Control and Prevention, Public Domain)
Nutritional Requirements During Infancy

Requirements for macronutrients and micronutrients per kilogram are higher during infancy than at any other stage in the human life cycle. These needs are affected by the rapid cell division that occurs during growth, which requires energy and protein, along with the nutrients involved in synthesizing DNA and other cellular components. Children depend entirely on their parents or other caregivers during this period to meet these needs. Breast milk is the best source to fulfill nutritional requirements for almost all infants six months or younger. An exclusively breastfed infant does not even need extra water, including in hot climates.
A newborn infant (birth to 28 days) requires feedings eight to twelve times a day or more. Between 1 and 3 months of age, the breastfed infant becomes more efficient, and the number of feedings per day often become fewer even though the amount of milk consumed stays the same. After about six months, infants can gradually begin to consume solid foods to help meet nutrient needs. Foods that are added in addition to breastmilk are called complementary foods. Complementary foods should be nutrient dense to provide optimal nutrition. Complementary foods include baby meats, vegetables, fruits, infant cereal, and dairy products such as yogurt, but not infant formula. Infant formula is a substitute, not a complement to breastmilk. In addition to complementary foods, the World Health Organization recommends that breastfeeding continue up to 2 years of age or beyond.[10] Dietary Guidelines for Americans 2020-2025 recommends Human milk feeding alone is the ideal form of nutrition from birth through about age 6 months. Human milk provides necessary nutrients, protective factors against disease, and other unique immunological benefits. If human milk is unavailable, infants should be fed an iron fortified commercial infant formula. Once an infant is developmentally ready, foods and beverages should be introduced to complement human milk feeding. These complementary foods and beverages are essential to meet the nutrient requirements of infants starting at about age 6 months and should be selected carefully to help meet these needs. As an infant becomes a toddler, and learns to eat a variety of foods, flavors, and textures, the goal of complementary feeding becomes establishing a healthy dietary pattern and transitioning to a healthy family diet by age 2.[11]
Energy and Macronutrients

Energy needs relative to size are much greater in infants than in adults. A baby’s resting metabolic rate is two times that of an adult. The RDA to meet energy needs changes as an infant matures and puts on more weight. The IOM uses a set of equations to calculate the total energy expenditure and resulting energy needs. For example, the equation for the first three months of life is (89 x weight [kg] −100) + 175 kcal.
Based on these equations, the estimated energy requirement for infants from zero to six months of age is 472 to 645 kilocalories per day for boys and 438 to 593 kilocalories per day for girls. For infants ages six to twelve months, the estimated requirement is 645 to 844 kilocalories per day for boys and 593 to 768 kilocalories per day for girls. From one to two, the estimated requirement rises to 844–1,050 kilocalories per day for boys and 768–997 kilocalories per day for girls.[12] How often an infant wants to eat will also change over time due to growth spurts, typically occurring at about two weeks and six weeks of age, and again at about three months and six months.
The dietary recommendations for infants are based on the nutritional content of human breast milk. Carbohydrates make up about 40 to 55 percent of the caloric content in breast milk, which amounts to an RDA (AI) of about 60 grams for infants 0-6 months old, and 95 grams for infants 7-12 months old. Almost all of the carbohydrate in human milk is lactose, which infants digest and tolerate well. In fact, lactose intolerance is practically nonexistent in infants. Proteins make up about 5 to 9 percent of the caloric content of breast milk, which amounts to an RDA (AI) of 9.1 grams per day for infants 0-6 months, and an RDA of 11 grams per day for infants 7-12 months. Infants have a high need for protein to support growth and development. However, excess protein (which is only a concern with bottle-feeding) can cause dehydration, diarrhea, fever, and acidosis in premature infants. American Academy of Pediatrics recommends no restriction on fats and cholesterol on infants under one years of age unless there is a medical reason for restriction. Infants due to their rapid growth require high energy intake. About 30 to 50 percent of the caloric content in breast milk is made up of fat. A high-fat diet that includes cholesterol is necessary to support the development of neural pathways in the brain and throughout the body. However, saturated fats and trans fatty acids inhibit this growth. Infants who are over the age of six months, which means they are receiving complementary foods, should not consume foods that are high in these types of fats. The RDA (AI) for total fat is 30 grams per day for infants 0-6 months old and 31 grams per day for infants 7-12 months old.[13]
Micronutrients
Almost all of the nutrients that infants require during the first 6 months can be met if they consume an adequate amount of breast milk. There are a few exceptions, though. Unless the mother is taking a large dose of Vitamin D, human milk will be low in vitamin D, which is needed for calcium absorption and building bone, among other things. Therefore, breastfed children often need to take a vitamin D supplement in the form of drops. Infants at the highest risk for vitamin D deficiency are those with darker skin and little to no exposure to sunlight, and those born prematurely. Breast milk is also low in vitamin K[14], which is required for blood clotting, and deficits could lead to bleeding or hemorrhagic disease. Babies are born with limited vitamin K, so supplementation may be needed initially and some states require a vitamin K injection after birth. Also, breast milk is not high in iron, but the iron in breast milk is well absorbed by infants. After five to eight months, however, an infant needs an additional source of iron other than breast milk. For exclusively breastfed infants, 6 months of age is a good time to introduce sources of highly bioavailable iron and zinc such as baby meats. Iron-fortified cereals and beans can boost the iron intake as well.
Fluids
Infants have a high need for fluids, 1.5 milliliters per kilocalorie consumed compared to 1.0 milliliters per kilocalorie consumed for adults. This is because children have a larger body surface area per unit of body weight and a higher metabolic rate. Therefore, they are at greater risk of dehydration. However, parents or other caregivers can meet an infant’s fluid needs with breast milk or formula. As solids are introduced, parents must make sure that young children continue to drink fluids throughout the day.
Breastfeeding
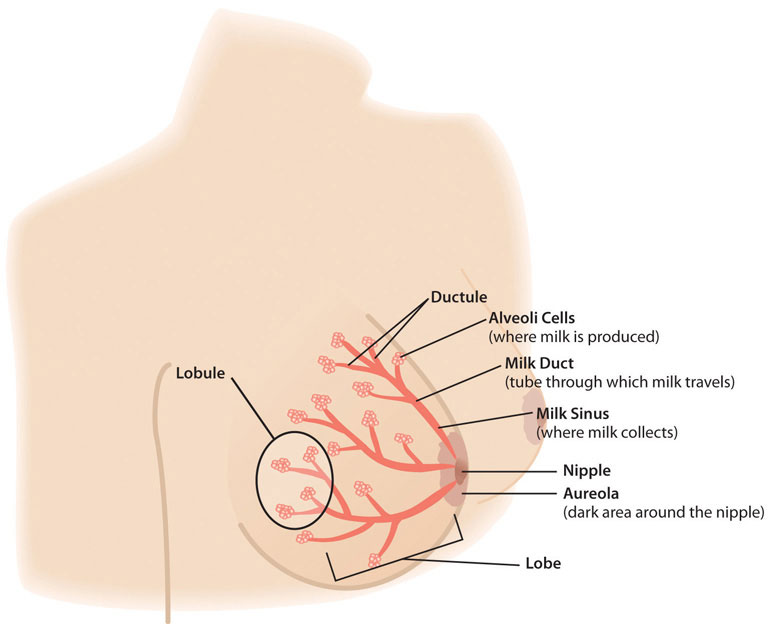
(Source: University of Hawaii @ Manoa, CC-BY-NC-SA)
Although few aspects of human nutrition are surrounded by as much public controversy as is the choice to breastfeed or formula feed an infant, a little knowledge about the science of breastfeeding can go a long way to settling this debate. This section will cover the science of lactation and practical ways to improve both the breastfeeding experience and the nutritional status of mothers and infants. Learning about the different parts of the breast and their function is a first step to becoming better able to support mothers who want to breastfeed.
The structure of the breast includes the alveoli which are grape-like clusters where milk is made. A network of ducts branch out and carry the milk from the alveoli to the nipple. A tiny muscle surrounds each of the alveoli; when a baby nurses at the breast, a hormone is released from the mother’s brain that makes these muscles contract and push the milk out into the ducts and towards the nipple. Groups of alveoli connected by ducts are organized into lobes, or sections, of the breast. The breast contains 15 to 25 lobes, and each lobe contains 10 to 100 alveoli.
The areola is the darker skin around the nipple and is a visual target that helps the baby find the breast. The bumps on the areola are glands that provide lubrication and protection to the tissue. These glands also produce a scent to help the baby find the nipple. The nipple and areola contain erectile smooth muscles that contract to make the nipple protrude more during breastfeeding. Nipples come in many sizes and shapes and contain from 4 to 18 openings for the milk to flow out. Mothers do not need to do anything to get their nipples ready to breastfeed.
Breast size is mainly determined by the amount of fat in the breast; the milk-making structures don’t vary as much as the amount of fat tissue. Most mothers can make enough milk for their babies whether they have small or large breasts. It is normal for a woman to have one breast that is different than the other in size or shape. During pregnancy, the breasts will normally increase in size. If a woman does not notice any changes to her breast during pregnancy, she should discuss this with her healthcare provider or a lactation consultant.
After the birth of the baby, nutritional needs must be met to ensure that an infant not only survives, but thrives from infancy into childhood. Breastfeeding provides the fuel a newborn needs for rapid growth and development. As a result, the WHO recommends that breastfeeding is exclusive (no other food or drink) for the first six months of an infant’s life.[15] Exclusive breastfeeding is one of the best ways a mother can support the growth and protect the health of her infant child. Breast milk contains nearly all of the nutrients that a newborn requires and gives a child the best start to a healthy life. Most women want to breastfeed their babies; in the US, over 80% of women start to breastfeed their infants.[16] Unfortunately, a mother’s intention alone may not be enough to make this practice successful. Around the world, approximately 40 percent of infants are breastfed exclusively for the recommended 6 months.[17]
Lactation Physiology
Preparation for making breast milk, although begun in puberty, is not completed until a woman’s first pregnancy. Early in the first trimester, the cells that will secrete milk divide and multiply. Hormones play a major role in preparing the woman’s body to breastfeed, particularly during the second and third trimesters. At that point, levels of the hormone prolactin increase to stimulate the growth of the milk duct system, which initiates and maintains milk production. Also during pregnancy, progesterone stimulates growth of the alveoli, the clusters of cells where the milk is made. During this process ducts that will carry the milk grow larger and branch out, and new capillaries are also formed to circulate the increased blood supply. However, levels of the hormone progesterone need to decrease for successful milk production, because progesterone inhibits milk secretion. Shortly after birth, the expulsion of the placenta triggers progesterone levels to fall, which activates lactation.[18] When the infant suckles at the breast, levels of the hormone oxytocin rise to promote the release of breast milk from the breast when the infant suckles, which is known as the milk-ejection reflex.
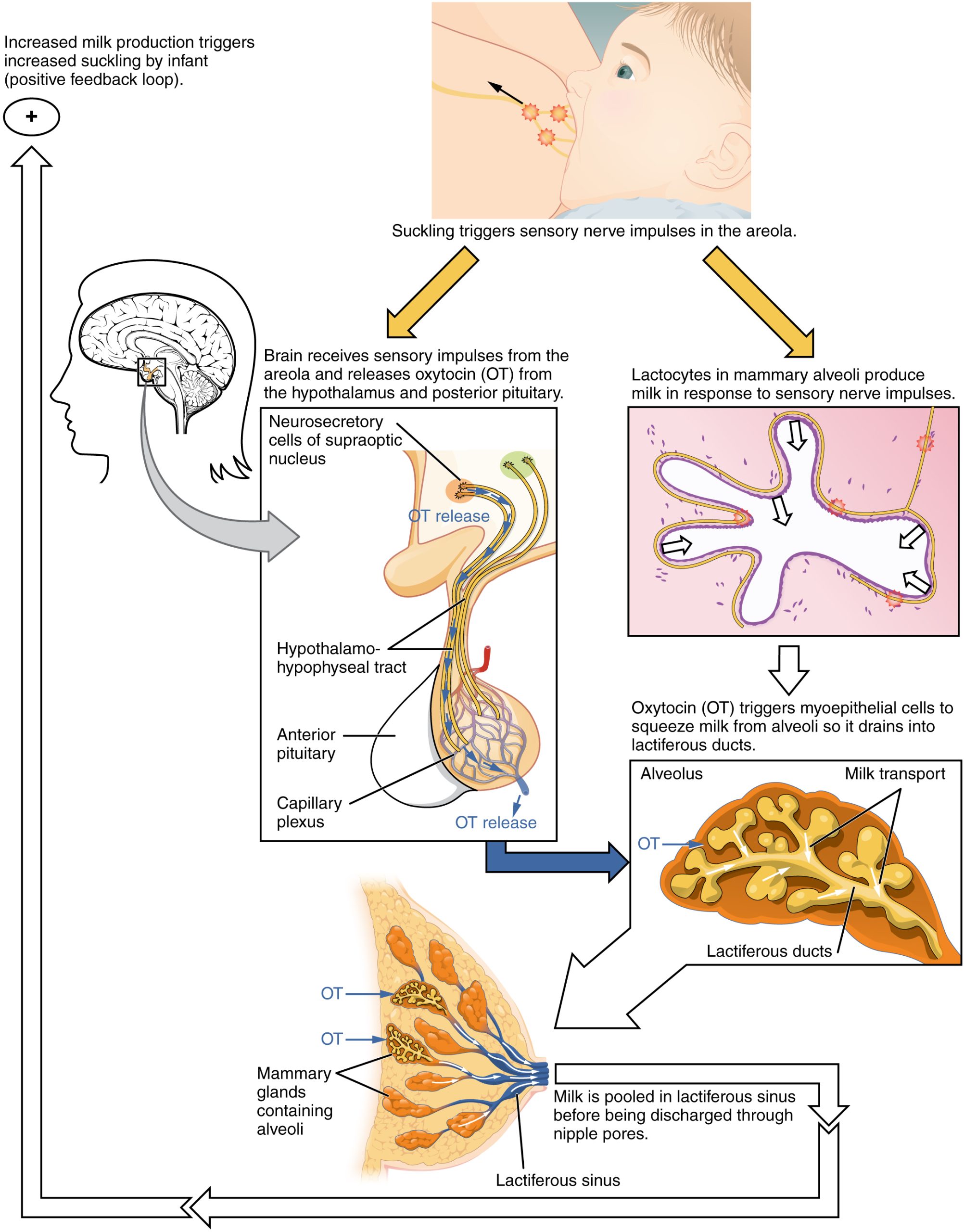
(Source: Lumen Learning, CC-BY)
Lactational Nutritional Needs
New mothers must also carefully consider their nutritional requirements to help their bodies recover in the wake of the pregnancy. This is particularly true for women who breastfeed their babies, which increases the need for specific nutrients.
New mothers usually find that their appetite and thirst are greater than before pregnancy; it is recommended that they still focus on nutrient-dense foods to nourish their body and replace their body’s nutrient stores. A conservative rate of weight loss (1-2 pounds per week) during lactation does not usually impact the quantity or quality of breast milk, but maternal deficiencies in some nutrients have been described during lactation. The nutrient content of breastmilk does not change much based on maternal diet for most nutrients. The RDA for energy is 330 additional Calories during the first six months of lactation and 400 additional Calories during the second six months of lactation. The energy needed to support breastfeeding comes from increased intake and stored fat. For example, during the first six months after her baby is born, the daily caloric cost for a lactating mother is 500 Calories, with 330 calories derived from increased intake and 170 Calories derived from maternal fat stores. This helps explain why breastfeeding may promote weight loss in new mothers. Lactating women should also drink 3.1 liters of liquids per day (about 13 cups) to avoid dehydration, according to the IOM. As is the case during pregnancy, the RDA of most vitamins and minerals increases for women who are breastfeeding their babies. Most doctors and nutritionists recommend that lactating women continue taking their prenatal vitamin/mineral supplements during lactation. The following table compares the recommended vitamins and minerals for lactating women to the levels for nonpregnant and pregnant women.[19]
| Nutrient | Nonpregnant Women | Pregnant Women | Lactating Women |
|---|---|---|---|
| Vitamin A (mcg) | 700.0 | 770.0 | 1,300.0 |
| Vitamin B6 (mg) | 1.3 | 1.9 | 2.0 |
| Vitamin B12 (mcg) | 2.4 | 2.6 | 2.8 |
| Vitamin C (mg) | 75.0 | 85.0 | 120.0 |
| Vitamin D (mcg) | 5.0 | 5.0 | 5.0 |
| Vitamin E (mg) | 15.0 | 15.0 | 19.0 |
| Calcium (mg) | 1,000.0 | 1,000.0 | 1,000.0 |
| Folate (mcg) | 400.0 | 600.0 | 500.0 |
| Iron (mg) | 18.0 | 27.0 | 9.0 |
| Magnesium (mg) | 310.0 | 350.0 | 310.0 |
| Niacin (B3) (mg) | 14.0 | 18.0 | 17.0 |
| Phosphorus | 700.0 | 700.0 | 700.0 |
| Riboflavin (B2) (mg) | 1.1 | 1.4 | 1.6 |
| Thiamine (B1) (mg) | 1.1 | 1.4 | 1.4 |
| Zinc (mg) | 8.0 | 11.0 | 12.0 |
Calcium requirements do not change during breastfeeding because of more efficient absorption, which is the case during pregnancy. However, the reasons for this differ. During pregnancy, there is enhanced absorption within the gastrointestinal tract. During lactation, the kidneys enhance retention. The RDA for phosphorus and fluoride also remains the same.
Components of Breastmilk
Human breast milk not only provides adequate nutrition for infants, it also helps to protect newborns from disease. In addition, breast milk is rich in cholesterol, which is needed for brain development. It is helpful to know the different types and components of breastmilk, along with the nutrients they provide to enable an infant to survive and thrive.
Colostrum is the milk produced immediately after birth, prior to the start of mature milk production, and lasts for two to five days after the arrival of the baby. Cells in the breast can begin to secrete colostrum by mid-pregnancy. During the last trimester, the alveoli (grape-like clusters of cells that produce milk) can become swollen with colostrum. Colostrum is thicker than mature breast milk, and is yellowish or creamy in color. This protein-rich liquid fulfills an infant’s nutrient needs during those early days. Although low in volume, colostrum is packed with concentrated nutrition for newborns. This special milk is high in fat-soluble vitamins, minerals, and immunoglobulins (antibodies) that pass from the mother to the baby. Immunoglobulins provide passive immunity for the newborn and protect the baby from bacterial and viral diseases.[20] Colostrum also helps the baby to eliminate waste (meconium).
Two to four days after birth, colostrum is replaced by transitional milk. Nursing the baby early (within the first hour of birth) and frequently (8 to 14 times per 24 hours) helps to bring in this increased volume of milk sooner. Transitional milk is a creamy, usually yellow liquid that lasts for approximately two weeks and includes high levels of fat, lactose, and water-soluble vitamins. It also contains more calories than colostrum. As a new mother begins to produce transitional milk, she typically notices an increase in the weight and size of her breasts and a change in the volume and type of liquid secreted.[21]
Mature milk is the final milk that a new mother produces. Its composition varies from morning to night, from the beginning of the feeding to the end, and from early postpartum to later in infancy and toddlerhood. Breastmilk that is produced by mothers of premature infants is higher in protein and calcium to meet the needs of the preemie. Foremilk (the milk that comes at the beginning of a feeding) tends to be lower in fat. Hind-milk comes towards the end of a feeding containing higher levels of fat, which helps the baby to feel satisfied and full. Combined, these two types of milk ensure that a baby receives adequate nutrients to grow and develop properly.[22]
About 87.5 percent of mature milk is water, which helps an infant remain hydrated. The other 12.5 percent contains carbohydrates, proteins, fats, vitamins and minerals which support energy and growth. Similar to cow’s milk, the main carbohydrate of mature breast milk is lactose. Breast milk contains the essential fatty acids, linoleic acid and alpha-linolenic acid, and other fats that are important for development such as docosahexaenoic acid (DHA). In terms of protein, breast milk contains more whey than casein (which is the reverse of cow’s milk). Whey is much easier for infants to digest than casein. Casein and whey make a complete protein with all of the essential amino acids. Another protein in breastmilk, lactoferrin is an iron-binding protein that helps keep iron away from pathogenic bacteria and facilitates the absorption of iron into an infant’s bloodstream.
For most vitamins and minerals, breast milk provides adequate amounts for growth and maintenance of optimal health. Although the absolute amounts of some micronutrients are low, they are more efficiently absorbed by infants from breast milk. Other essential components include digestive enzymes that help a baby digest the breast milk. Human milk also provides the hormones and growth factors that help a newborn to develop.
Diet and Milk Quality
A mother’s health habits can impact milk production and quality. During pregnancy, lactating mothers should avoid illegal substances and cigarettes. Some legal drugs and herbal products can be harmful as well, so it is helpful to discuss them with a healthcare professional. In some rare cases, mothers may need to avoid certain things, such as dairy or spicy foods, that can produce gas in sensitive infants. Lactating women can drink alcohol, though they must avoid breastfeeding until the alcohol has completely cleared from their milk. Typically, this takes two to three hours for 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor, depending on a woman’s body weight.[23] Precautions are necessary because exposure to alcohol can negatively affect infant growth.
Benefits of Breastfeeding
Breastfeeding has several benefits, both for the mother and for the child. Breast milk contains immunoglobulins, enzymes, immune factors, and white blood cells. As a result, breastfeeding boosts the baby’s immune system and lowers the incidence of diarrhea, respiratory diseases, gastrointestinal infections, and ear infections. Breastfed babies are also less likely to develop asthma and allergies, and breastfeeding lowers the risk of sudden infant death syndrome. In addition, human milk encourages the growth of a healthy microbiome (the bacteria in an infant’s intestinal tract). Most of these benefits remain after an infant has been weaned from breast milk. Some studies suggest other possible long-term effects. For example, breast milk may improve an infant’s intelligence and protect against Type 1 diabetesand obesity, although research is ongoing in these areas.[24]
Breastfeeding has a number of other important benefits. It is easier for babies to digest breast milk than infant formula, which contains proteins made from cow’s milk or soybeans that are harder to tolerate. Breastfed infants are sick less often than bottle-fed infants. Breastfeeding is more sustainable and results in less plastic waste and other trash. Breastfeeding can also save families money because it typically saves over $1,200 per year in the US over purchasing formula. Other benefits include that breast milk is always ready. It does not have to be mixed, heated, or prepared. Also, breast milk is sterile and is always at the right temperature.
In addition, the skin-to-skin contact of breastfeeding promotes a close bond between mother and baby, which is an important emotional and psychological benefit. The practice also provides health benefits for the mother. Breastfeeding reduces the risk of Type 2 Diabetes in the mother and infant. Studies have also shown that breastfeeding reduces the risk of breast and ovarian cancers.[25]
The Baby-Friendly Hospital Initiative
In 1991, the WHO and UNICEF launched the Baby-Friendly Hospital Initiative (BFHI), which works to ensure that all maternity care facilities, including hospitals and free-standing facilities, become centers of breastfeeding support. A maternity care facility can be denoted as “baby-friendly” when it does not accept free infant formula and has implemented The Ten Steps to Successful Breastfeeding. These steps include having a written policy on breastfeeding communicated to health-care staff on a routine basis, informing all new mothers about the benefits and management of breastfeeding, showing new mothers how to breastfeed their infants, and how to maintain lactation, and giving newborns no food or drink other than breast milk, unless medically indicated. Since the BFHI began, more than fifteen thousand facilities in 134 countries, from Benin to Bangladesh, have been deemed “baby friendly.” As a result, more mothers are breastfeeding their newborns, and infant health has improved, in both the developed world and in developing nations.[26] Visit the Baby-Friendly Initiative in the US for more information (opens in a new window).
Barriers to Breastfeeding
Although breast milk is ideal for almost all infants, there are some challenges that nursing mothers may face when starting and continuing to breastfeed their infants. These obstacles include painful engorgement or fullness in the breasts, often around day 3 to 5 postpartum, sore and tender nipples, lack of comfort or confidence in public, and lack of accommodation to breastfeed or express milk in the workplace.
One of nursing mothers’ first challenges is learning how to position the baby at her breast comfortably. Improper position and latching usually result in pain for the mother and inadequate intake for the infant, which could slow growth and development. However, all International Board Certified Lactation Consultants (IBCLCs) and most Obstetric nurses are trained to help new mothers learn the proper technique. Some registered dietitians are trained in lactation support as well. A very helpful position for new mothers is called the “Laid-Back Nursing” position, and it usually helps the mother and baby to feel more comfortable, and helps the baby latch on without causing any nipple pain. Resources on the laid back position can be found here: https://lllusa.org/lie-back-and-relax-a-look-at-laid-back-breastfeeding/ (opens in a new window).
Education, the length of maternity leave, and laws to protect public breastfeeding, among other measures, can all help to facilitate breastfeeding for many lactating women and their newborns.
Contraindications to Breastfeeding
Although there are numerous benefits to breastfeeding, in some cases, risks must be considered. In the developed world, a new mother with HIV should not breastfeed, because the infection can be transmitted through breast milk. These women typically have access to safe infant formula and water that can be used as a replacement for breast milk. However, in developing nations where HIV infection rates are high and acceptable infant formula can be challenging to find, many newborns would be deprived of the nutrients they need to develop and grow. Also, inappropriate or contaminated infant formulas cause 1.5 million infant deaths each year. As a result, the WHO recommends that women infected with HIV in the developing world should nurse their infants while taking antiretroviral medications to lower the risk of transmission.[27] In any case, combination feeding (formula and breastmilk together) is not recommended for mothers who are HIV positive because the risk of transmitting HIV to the infant is higher than either breastfeeding or formula feeding alone.
Breastfeeding is also not recommended for women undergoing radiation or chemotherapy treatment for cancer. Additionally, if an infant is diagnosed with galactosemia, meaning an inability to process the simple sugar galactose, the child must be on a galactose-free diet, which excludes breast milk. This genetic disorder is a very rare condition, however, and only affects 1 in thirty to sixty thousand newborns.[28] Also, if mothers are using an illicit drug, such as opioids, PCP (phencyclidine), or cocaine, they should not be breastfeeding. For mothers who discontinue illicit opioids or other substances and are on stable methadone or buprenorphine maintenance therapy, breastfeeding should be encouraged.[29] Mothers with suspected or confirmed Ebola virus disease shouldnt be breastfeeding.[30] In the case of active tuberculosis[31] or certain viruses like chicken pox, breastfeeding should not be done during an active infection or if infection occurs within a certain time frame of birth but expressed breast milk can be fed to the baby. When breastfeeding is contraindicated for any reason, feeding a baby formula enables parents and caregivers to meet their newborn’s nutritional needs.
There are a few medications that you cannot take while breastfeeding. Although many medications pass into breast milk, most have no known adverse effect on milk supply or infant well-being. However, healthcare providers should always weigh the risks and benefits when prescribing medications to women who are breastfeeding.[32]
Bottle-Feeding
Most women can breastfeed when given sufficient education and support. However, as discussed, a small percentage of women are unable to breastfeed their infants, while others choose not to. For parents who choose to bottle-feed, infant formula balances nutrients. However, not all formulas are the same, and there are important considerations that parents and caregivers must weigh. Standard formulas use cow’s milk as a base. They have 20 calories per fluid ounce, similar to breast milk, with vitamins and minerals added. Often, parents start their babies on soy formula because they incorrectly assume that soy formula will reduce allergies and other health problems, but this is not the case. Soy-based formulas are sometimes given to infants with diarrhea, constipation, vomiting, colic, or abdominal pain. Still, more often these babies are put on hydrolysate formula to address these concerns. Hypoallergenic protein hydrolysate formulas are given to infants who are allergic to cow’s milk and soy protein or have trouble tolerating them. This type of formula uses hydrolyzed protein, meaning that the protein is broken down into amino acids and small peptides, which makes it easier to digest and makes it less likely to trigger gastrointestinal distress. Preterm infant formulas are given to premature and low birth weight infants, if breast milk is unavailable. Preterm infant formulas have 24 calories per fluid ounce and are given until the infant reaches a desired weight. These formulas are also higher in protein, calcium, and phosphorus to meet the special needs of premature infants.
Infant formula comes in three basic types:
- Powder that requires mixing with water. This is the least expensive type of formula.
- Concentrates are liquids that must be diluted with water. This type is slightly more expensive.
- Ready-to-use liquids that can be poured directly into bottles. This is the most expensive type of formula. However, it requires no preparation. Ready-to-use formulas are used when a safe and sanitary water supply is unavailable. Ready-to-use formulas are also convenient for traveling.
Most babies need about 2.5 ounces of formula per pound of body weight each day. Therefore, the average infant consumes about 24 fluid ounces of breastmilk or formula per day, or one ounce per hour. If infants sleep for 2 hours, they often consume 2 ounces of breastmilk or formula at their next feeding. Parents and caregivers should carefully follow the mixing instructions and safety guidelines when preparing formula, since an infant has an immature immune system. All equipment used in formula preparation should be sterilized for newborns, and especially premature infants. Prepared, unused formula should be refrigerated to prevent bacterial growth. A partially finished bottle of infant formula should be discarded after 1 hour. Parents must make sure not to use contaminated water to mix formula in order to prevent foodborne or other illnesses. Follow the instructions for powdered and concentrated formula carefully—formula that is overly diluted will not provide adequate calories and protein, while overly concentrated formula provides too much protein and too little water, which can challenge immature kidneys and lead to dehydration.
Around 6 months of age, infants can start sipping expressed breast milk, infant formula, or water from a cup. By 12 to 14 months of age, children should be using a cup for all liquids.
It is important to note again that both the American Academy of Pediatrics and the WHO state that breast milk is far superior to infant formula. This table compares the advantages of giving a child breast milk to the disadvantages of using bottle formula.[33]
| Breast Milk | Bottle Formula |
|---|---|
| Antibodies and lactoferrin in breast milk protect infants. | The formula does not contain immunoprotective factors. |
| The iron in breast milk is absorbed more easily. Because the iron is bound to lactoferrin, it is not available for bacteria in the gut to use as a growth factor. | Formula contains more iron than breast milk, but it is not absorbed as easily, and the iron is a growth factor for pathogenic microbes. |
| The feces babies produce do not smell because breastfed infants have different bacteria in the gut. | The feces that bottle-fed infants produce tend to have a foul-smelling odor. |
| Breast milk is always available and is always at the correct temperature. | The formula must be prepared, refrigerated for storage, and warmed before giving it to an infant. |
| Breastfed infants are less likely to have constipation. | Bottle-fed infants are more likely to have constipation. |
| Breastfeeding ostensibly is free, though purchasing optional supplies such as a pump and bottles to express milk does require some expense. | The formula must be purchased and is expensive, typically costing over $1,200 in the first year. |
| Breast milk contains the fatty acids DHA and EPA, vital for brain and vision development. | Some formulas contain DHA and EPA. |
Introducing Solid Foods

Some infants may show developmental signs of readiness before age 6 months, but introducing complementary foods before age 4 months is not recommended. Waiting until after age 6 months to introduce foods is also not recommended. Starting around that time, complementary foods are necessary to ensure adequate nutrition and exposure to flavors, textures, and different foods. Infants should be given age- and developmentally appropriate foods to help prevent choking. It is important to introduce potentially allergenic foods along with other complementary foods. For infants fed human milk, it is particularly important to include complementary foods that are rich in iron and zinc when starting complementary foods.[34]
Infants should be breastfed or bottle-fed exclusively for the first six months of life, according to the WHO. At about 6 months, infants should be introduced to nutrient-dense, developmentally appropriate foods to complement human milk or infant formula feedings. Foods that are added in addition to breast milk are called complementary foods. Some infants may show developmental signs of readiness before age 6 months, but introducing complementary foods before age 4 months is not recommended. Waiting until after age 6 months to introduce foods is also not recommended. Starting around that time, complementary foods are necessary to ensure adequate nutrition and exposure to flavors, textures, and different foods. Infants should be given age- and developmentally appropriate foods to help prevent choking. It is important to introduce potentially allergenic foods along with other complementary foods. For infants fed human milk, it is particularly important to include complementary foods that are rich in iron and zinc when starting complementary foods.[35] Complementary foods include baby meats, vegetables, fruits, infant cereal, and dairy products such as yogurt, but not infant formula. Infant formula is a substitute, not a complement to breast milk.
Infants should not consume solid foods prior to six months because most solids are less nutritious than breast milk. Eating solids before 6 months of age usually means drinking less breast milk and is associated with more ear infections and respiratory infections. If parents try to feed an infant who is too young or is not ready, their tongue will push the food out; this is called an extrusion reflex. After six months, the suck-swallow reflexes are not as strong, and infants can hold up their heads and move them around, both of which make eating solid foods more feasible.
Solid baby foods can be bought commercially or prepared from regular food using a food processor, blender, food mill, or grinder at home. By nine months to a year, infants are able to chew soft foods and can eat solids that are well-chopped or mashed. Infants who are fed solid foods before 4 months of age are susceptible to developing food allergies. Therefore, as parents and caregivers introduce solids, they should feed their child only one new food at a time to help identify allergic responses or food intolerances. An iron supplement is also recommended at this time. Rice is no longer recommended as a first-born food because of its high arsenic content. When cereals are introduced, parents can try baby oats or baby wheat.
A guide to infant feeding can be found in the 2019 USDA Infant Nutrition and Feeding Guide at: https://wicworks.fns.usda.gov/resources/infant-nutrition-and-feeding-guide (opens in a new window).
Guidelines for feeding healthy infants from the USDA Infant Nutrition and Feeding Guidelines are adapted in the table below.[36]
| Age | Human Milk or infant formula | Grain products | Vegetables | Fruit | Protein-rich foods |
|---|---|---|---|---|---|
| Birth – 6 months |
|
None | None | None | None |
| 6-8 months |
|
About 1-2 ounces iron-fortified infant cereals, bread, small pieces of crackers | About 2-4 ounces of cooked, plain, strained/ pureed/ mash vegetables | About 2-4 ounces of plain strained/ pureed/ mashed fruits | About 1-2 ounces meat, poultry, fish, eggs, cheese, yogurt, or legumes; all are plain strained/ pureed/ mashed |
| 8-12 months |
|
About 2-4 ounces iron-fortified infant cereals; other grains: baby crackers, bread, noodles, corn, grits, soft tortilla pieces | About 4-6 ounces, ground/ finely chopped/ diced | About 4-6 ounces, ground/ finely chopped/ diced | About 2-4 ounces meat, poultry, fish, eggs, cheese, yogurt, or mashed legumes; all are ground/ finely chopped/ diced |
NOTE: These are general guidelines for the healthy, full-term infant per day; serving sizes may vary with individual infants. Start complementary foods when developmentally ready, about 6 months; start with about 0.5-1 ounce.
Foods to Avoid
Many foods can cause harm to infants, including:
- Honey should never be given to a child under 12 months, including honey graham crackers and other foods with honey.
- Cow’s Milk should never be given to a child under 12 months.
- Plant-based Milk Alternatives
- Added Sugars, Syrups, Sugars, Artificial Sweeteners, and Sugar-Sweetened Beverages
- Vegetables High in Nitrates – spinach, beets, carrots, collard greens, or turnips should not be fed to infants less than 6 months of age.
- Raw or Partially Cooked Meat, Fish, or Poultry
- Foods Higher in Sodium are found in a number of foods, including some salty snacks, commercial toddler foods, and processed meats.
- Unpasteurized Foods and Beverages
Certain foods should also be avoided as they are choking hazards. Foods such as hot dogs, nuts and seeds, hard fruits and vegetables, and sticky foods like marshmallows can cause choking and must be avoided. These foods are listed in the table from the USDA Infant Nutrition and Feeding Guidelines.[37]
| Vegetables | Fruits | Protein-rich foods | Grain products | Other foods and snacks |
|---|---|---|---|---|
| Small pieces of raw vegetable (like raw carrot rounds, baby carrots, string beans, or celery), or other raw, partially cooked vegetables | Apples or other hard pieces of raw fruit, especially those with hard pits or seeds | Tough or large chunks of meat | Plain wheat germ | Hard or round candy |
| Raw green peas | Large, hard pieces of uncooked dried fruits | Hot dogs, meat sticks, or sausages (even when cut into round slices | Whole-grain kernels | Jelly beans |
| Cooked or uncooked whole corn kernels | Whole pieces of canned fruit | Fish with bones | Crackers or breads with seeds | Caramels |
| Large, hard pieces of uncooked dried vegetables | Whole grapes, cherries, berries, melon balls, or cherry and grape tomatoes | Large chunks of cheese or string cheese | Nut pieces | Gum drops, gummy candies, or other gooey or sticky candy |
| Peanuts, nuts, or seeds (like sunflower or pumpkin seeds) | Hard pretzels | Chewy fruit snacks | ||
| Chunks or spoonfuls of peanut butter or other nut and seed butters | Chewing gum | |||
| Whole beans | Marshmallows | |||
| Popcorn, potato or corn chips, or similar snack foods | ||||
| Ice cubes |
Learning to Self-Feed
With the introduction of solid foods, young children begin to learn how to handle food and how to feed themselves. At six to seven months, infants can use their whole hand to pick up items (this is known as the palmar grasp). They can lift larger items, but picking up smaller pieces of food is difficult. At eight months, a child might be able to use a pincer grasp, which uses fingers to pick up objects. After the age of one, children slowly begin to use utensils to handle their food. Unbreakable dishes and cups are essential, since very young children may play with them or throw them when bored with their food.
Food Allergies
Food allergies impact four to six percent of young children in America. In the United States, the nine major food allergens are:
- Milk
- Eggs
- Wheat
- Soybeans
- Tree nuts
- Peanuts
- Fish
- Shellfish
- Sesame
Approximately 90% of all food allergies are caused by these nine allergens. Eggs, milk, and peanuts are the most common causes of food allergies in children. Peanuts, tree nuts, fish, and shellfish commonly cause the most severe reactions. Nearly 8% of children under the age of 5 years have food allergies. Allergies to milk, egg, wheat, and soy often resolve in childhood, but can persist for longer or can be lifelong for some. Allergies to peanuts, tree nuts, fish, and/or shellfish are typically lifelong.[38]
Despite the risks of food allergies, lactating women should not make any changes to their diets. Research shows that nursing mothers who attempt to ward off allergies in their infants by eliminating certain foods may do more harm than good. According to the American Academy of Allergy, Asthma, and Immunology, mothers who avoided certain dairy products showed decreased levels in their breast milk of an immunoglobulin specific to cow’s milk. This antibody is thought to protect against the development of allergies in children. Even when an infant is at higher risk for food allergies, there is no evidence that alterations in a mother’s diet make a difference. It is also possible that continuing breastfeeding when solid foods are introduced into the infant’s diet may help prevent allergies. There is currently no scientific evidence indicating that delayed (after six months of age) or early (before four months of age) introduction of solid foods is preventative. However, there is evidence that introduction of solid foods after 17 weeks of age is associated with decreased risk of developing food allergies.[39][40] A landmark study done in 2015 showed that infants with increased risk for allergy to peanuts (severe eczema and/or egg allergy) had a much lower incidence of peanut allergy if minimal amounts (2 grams) were consumed 3 times a week beginning between 4-6 months of age rather than avoided until 60 months of age.[41] Because of this study, doctors now advise parents of children with a significant family history of allergies to introduce peanut protein between 4-6 months of age after the infant has begun eating other solid foods.
Food allergy symptoms may begin within minutes to an hour after eating the food. However, each child may experience symptoms differently. Symptoms may include:[42]
- Nausea or vomiting
- Diarrhea
- Stomach cramps or pain
- Rash or hives
- Face swelling
- Eczema
- Itching or swelling of the lips, tongue or mouth
- Itching or tightness in the throat
- Difficulty breathing or wheezing
- Lowered blood pressure combined with dizziness
Early Childhood Caries
Primary teeth are at risk for a disorder known as early childhood caries (ECC) from breast milk, formula, juice, or other drinks fed through a bottle. Liquids can build up in a baby’s mouth, and the natural or added sugars lead to decay. Early childhood caries is caused not only by the kinds of liquids given to an infant but also by the frequency and length of fluids. Giving a child a bottle of juice or other sweet liquids several times each day, or letting a baby suck on a bottle longer than a mealtime, either when awake or asleep, can also cause early childhood caries. In addition, this practice affects the development and position of the teeth and the jaw. The risk of early childhood caries continues into the toddler years as children consume more foods with a high sugar content. Therefore, parents should avoid putting their children to bed with a bottle and giving them sugary snacks and beverages. If a parent insists on giving their child a bottle in bed, it should only be filled with water.
Fluoride overuse can cause fluorosis, which can discolor the teeth and even adversely affect a person’s bones if too much is ingested. Hydroxyapatite (HAP) is a naturally occurring mineral that plays an important structural function in bones and teeth. When incorporated into toothpaste, it sticks to the enamel and forms a protective shield to reduce tooth decay risk. HAP-containing oral products can be considered an alternative in young children where fluorosis is a concern. In addition to reducing the need for traditional dental restorations, HAP also offers relief from dentin hypersensitivity. It reduces biofilm formation, making it a multifunctional preventive oral health care agent.[43]
Newborn Jaundice
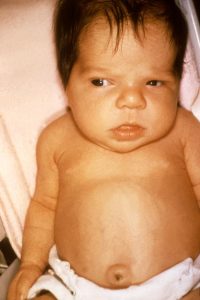
(Source: Wikimedia Commons, Centers for Disease Control and Prevention, Public Domain)
Newborn jaundice is a common occurrence in the first few weeks after birth. This condition can occur within a few days of birth and is characterized by yellowed skin or yellowing in the whites of the eyes, which can be harder to detect in dark-skinned babies. Jaundice typically appears on the face first, followed by the chest, abdomen, arms, and legs—elevated levels of bilirubin cause this condition in a baby’s bloodstream. Bilirubin is a substance created by the breakdown of red blood cells and is removed by the liver. Jaundice develops when a newborn’s liver does not efficiently remove bilirubin from the blood. There are several types of jaundice associated with newborns:
- Physiologic jaundice. The most common type of newborn jaundice can affect up to 60 percent of full-term babies in the first week of life.
- Breast-milk jaundice. The name for a condition that persists after physiologic jaundice subsides in otherwise healthy babies and can last for three to twelve weeks after birth. Breast-milk jaundice tends to be genetic, and there is no known cause, although it may be linked to a substance in the breast milk that blocks the breakdown of bilirubin. However, that does not mean breastfeeding should be stopped. As long as bilirubin levels are monitored, the disorder rarely leads to serious complications.
- “Inadequate breastfeeding jaundice.” Occurs when an infant does not get enough milk. This may happen because a newborn does not get a good start breastfeeding, does not latch on to the mother’s breast properly, or is given other substances that interfere with breastfeeding (such as juice). Treatment includes increased feedings, with help from a lactation consultant to ensure that the baby takes in adequate amounts.
Newborn jaundice is more common in a breastfed baby and tends to last a bit longer. If jaundice is suspected, a pediatrician will run blood tests to measure the amount of bilirubin in an infant’s blood. Treatment often involves increasing the number of feedings to increase bowel movements, which helps to excrete bilirubin. Within a few weeks, as the baby matures and red blood cell levels diminish, jaundice typically subsides with no lingering effects.[44]
Learning Activities
Technology Note: The second edition of the Human Nutrition Open Educational Resource (OER) textbook features interactive learning activities. These activities are available in the web-based textbook and are not in downloadable versions (EPUB, Digital PDF, Print_PDF, or Open Document).
Learning activities may be used across various mobile devices; however, for the best user experience, it is strongly recommended that users complete these activities using a desktop or laptop computer.
- Breastfeeding Recommendations. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/php/guidelines-recommendations/index.html. Accessed August 4, 2025. ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services (2020). Dietary Guidelines for Americans, 2020-2025. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf#page=66 . Accessed July 30, 2025 ↵
- Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/breastfeeding-call-to-action-executive-summary.pdf. Published January 20, 2011. Accessed August 14, 2025. ↵
- 10 Steps and International Code. Baby-Friendly USA. https://www.babyfriendlyusa.org/for-facilities/practice-guidelines/10-steps-and-international-code/. Accessed August 14, 2025. ↵
- Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/breastfeeding-call-to-action-executive-summary.pdf. Published January 20, 2011. Accessed August 14, 2025. ↵
- Resources. Louisiana Breastfeeding Coalition. http://www.louisianabreastfeeding.org/resources/#:~:text=Find%20local%20breastfeeding%20support%2C%20including%20lactation%20consultants%2C%20WIC,or%20by%20visiting%20the%20Partners%20for%20Family%20..Accessed August 4, 2025. ↵
- Acts 2001, No. 576, §1. Louisiana Laws - Louisiana State Legislature. https://legis.la.gov/Legis/Law.aspx?p=y&d=104292 Accessed August 4, 2025. ↵
- McMillan B. (2008). Illustrated Atlas of the Human Body. Weldon Owen. ↵
- OpenStax (2024). Chapter 23.2 Physical Assessment of the Newborn. Maternal-Newborn Nursing. https://med.libretexts.org/Bookshelves/Nursing/Maternal-Newborn_Nursing_(OpenStax)/23%3A_Newborn_Assessment/23.02%3A_Physical_Assessment_of_the_Newborn. Accessed August 4, 2025. ↵
- Infant and Young Child Feeding. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding. Published December 20, 2023. Accessed August 14, 2025. ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services (2020). Dietary Guidelines for Americans, 2020-2025. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf#page=66 . Accessed July 30, 2025 ↵
- Food and Nutrition Board, Institute of Medicine. (2005). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. The National Academies Press. https://nap.nationalacademies.org/read/10490/chapter/1. Accessed August 14, 2025. ↵
- Infant Nutrition and Feeding. United States Department of Agriculture. https://wicworks.fns.usda.gov/sites/default/files/media/document/infant-feeding-guide.pdf. Accessed August 4, 2025. ↵
- Ballard, O., & Morrow, A. L. (2013). Human Milk Composition: Nutrients and Bioactive Factors. Pediatric clinics of North America, 60 (1): 49–74. https://doi.org/10.1016/j.pcl.2012.10.002. Accessed August 14, 2025. ↵
- Infant and Young Child Feeding. UNICEF Data. https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/ Accessed August 14, 2025. ↵
- Breastfeeding Report Card. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding-data/breastfeeding-report-card/. Accessed August 4, 2025. ↵
- Global Breastfeeding Collective. UNICEF. https://www.unicef.org/breastfeeding/. Accessed August 14, 2025. ↵
- King, J., (2007). Contraception and Lactation. Journal of Midwifery and Women’s Health, 52 (6): 614–20. https://doi.org/10.1016/j.jmwh.2007.08.012. Accessed August 14, 2025. ↵
- Institute of Medicine (2006). Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. The National Academies Press. https://www.nap.edu/catalog/11537/dietary-reference-intakes-the-essential-guide-to-nutrient-requirements. Accessed August 4, 2025. ↵
- Breastfeeding: Overview. American Pregnancy Association. https://americanpregnancy.org/healthy-pregnancy/breastfeeding/breastfeeding-overview/. Access August 4, 2025 ↵
- Breastfeeding: Overview. American Pregnancy Association. https://americanpregnancy.org/healthy-pregnancy/breastfeeding/breastfeeding-overview/. Access August 4, 2025 ↵
- Breastfeeding: Overview. American Pregnancy Association. https://americanpregnancy.org/healthy-pregnancy/breastfeeding/breastfeeding-overview/. Access August 4, 2025 ↵
- Breastfeeding and Alcohol: Is it okay to drink?. Mayo Clinic. http://www.mayoclinic.com/health/breast-feeding-and-alcohol/AN02131. Accessed August 4, 2025. ↵
- Breastfeeding Benefits Your Baby’s Immune System. American Academy of Pediatrics. https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Breastfeeding-Benefits-Your-Babys-Immune-System.aspx. Accessed August 4, 2025. ↵
- Reproductive History and Breast Cancer Risk. National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/Risk/reproductive-history. Accessed August 4, 2025. ↵
- UNICEF. The baby-friendly hospital initiative. http://www.unicef.org/programme/breastfeeding/baby.htm ↵
- HIV/AIDS: Infant Feeding and Nutrition. World Health Organization. https://www.who.int/news-room/questions-and-answers/item/hiv-aids-infant-feeding-and-nutrition. Accessed August 4, 2025. ↵
- Galactosemia. MedlinePlus Genetics. https://medlineplus.gov/genetics/condition/galactosemia/. Accessed August 4, 2025. ↵
- Contraindications to Breastfeeding - Breastfeeding Special Circumstances. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/contraindications/index.html. Accessed August 4, 2025. ↵
- Ebola Virus Disease - Breastfeeding. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/ebola.html. Accessed August 4, 2025. ↵
- Tuberculosis in Pregnancy. Centers for Disease Control and Prevention. https://www.cdc.gov/tb/about/pregnancy.html. Accessed August 4, 2025. ↵
- Prescription Medication Use - Breastfeeding Special Circumstances. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/vaccine-medication-drugs/prescriptions.html. Accessed August 4, 2025. ↵
- Breastfeeding Versus Bottle Feeding. American Pregnancy Association. https://americanpregnancy.org/healthy-pregnancy/breastfeeding/breastfeeding-vs-bottle-feeding-formula/. Accessed August 4, 2025. ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services (2020). Dietary Guidelines for Americans, 2020-2025. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf#page=66 . Accessed July 30, 2025 ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services (2020). Dietary Guidelines for Americans, 2020-2025. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf#page=66 . Accessed July 30, 2025 ↵
- Infant Nutrition and Feeding. United States Department of Agriculture. https://wicworks.fns.usda.gov/sites/default/files/media/document/infant-feeding-guide.pdf. Accessed August 4, 2025. ↵
- Infant Nutrition and Feeding. United States Department of Agriculture. https://wicworks.fns.usda.gov/sites/default/files/media/document/infant-feeding-guide.pdf. Accessed August 4, 2025. ↵
- Food Allergies in Children and Babies. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/food-allergies-in-children. Accessed August 4, 2025. ↵
- Alvisi, P., Brusa, S., Alboresi, S., (2015). Recommendations on Complementary Feeding for Healthy, Full-Term Infants. Italian Journal of Pediatrics, 41 (36). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464122/. Accessed August 14, 2025. ↵
- Nursing Mom's Diet No Guard Against Baby's Allergies. Medpage Today. http://www.medpagetoday.com/MeetingCoverage/AAAAIMeeting/31527. Accessed August 14, 2025. ↵
- Du Toit, G., et al. (2015). Randomized Trial of Peanut Consumption in Infants at Risk for Peanut Allergy. New England Journal of Medicine, 372 (9): 803-813. https://doi.org/10.1056/nejmoa1414850. Accessed August 14, 2025. ↵
- Food Allergies in Children and Babies. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/food-allergies-in-children. Accessed August 4, 2025. ↵
- O'Hagan-Wong, K., et al., (2021). The Use of Hydroxyapatite Toothpaste to Prevent Dental Caries. Odontology, 110 (2): 223-230. https://link.springer.com/article/10.1007/s10266-021-00675-4. Accessed August 4, 2025. ↵
- Breastfeeding and Jaundice. https://americanpregnancy.org/healthy-pregnancy/breastfeeding/breastfeeding-and-jaundice/. Accessed August 4, 2025. ↵
The period of early childhood from birth to 1 year of age.
The production and secretion of milk.
The amount of energy that a person burns each day.
The daily requirement for dietary energy intake that is predicted to maintain energy balance in healthy, normal weight individuals.
A disaccharide made of glucose linked to galactose found in milk.
A condition that results from the inability to digest lactose. Symptoms include bloating, gas, abdominal pain, discomfort, and diarrhea.
A fat-soluble vitamin that is needed for blood clotting.
The standard unit of energy used in nutrition; the amount of heat required to raise temperature of 1 kg water 1℃ .
part of the structure of the human female breast, grape-like clusters where milk is made
A hormone released by the anterior pituitary that stimulates the mammary glands to produce milk.
The organ that anchors the developing fetus to the uterus that secretes hormones, transfers nutrients and oxygen from the mother’s blood to the fetus and removes metabolic wastes.
A hormone released by the posterior pituitary that stimulates the ejection of milk during lactation.
The first fluid secreted by the breast during late pregnancy and the first few days after birth. It is rich in immune factors and protein.
Proteins that contain all of the essential amino acids in proportions capable of promoting growth when they are the only proteins in the body.
A unexplained death of an infant that usually occurs during sleep.
Type 1 diabetes is a chronic autoimmune disease that prevents the pancreas from making insulin. It requires daily management with insulin injections and blood sugar monitoring. Both children and adults can be diagnosed with Type 1 diabetes
Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin.
A 6-carbon monosaccharide arranged in a ring structure part of the disaccharide lactose.
Two or more amino acids joined together by peptide bonds.
An infant that is born before the 37 weeks of gestation.
A birth weight less than 2.5 kg or 5.5 lbs.

