Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.[1] See Figure 20.1[2] for an illustration of the phases of wound healing.
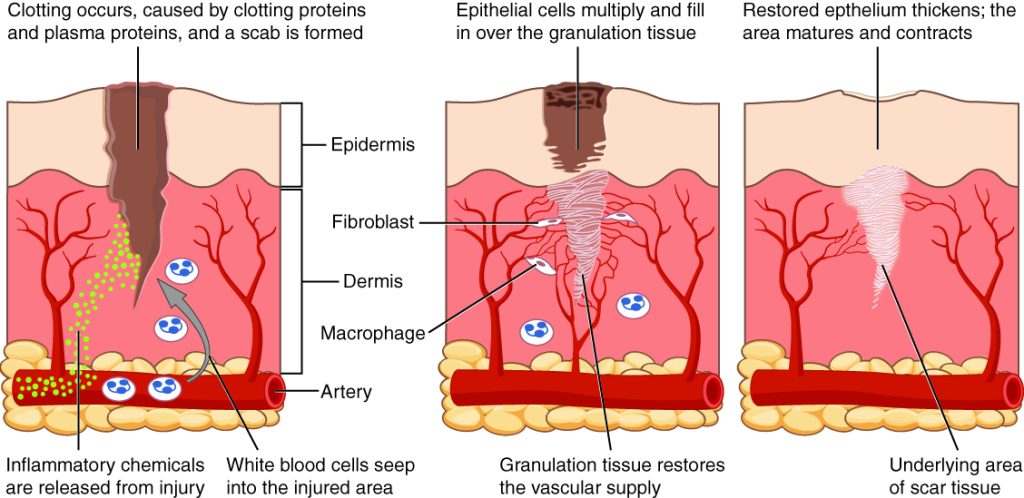
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple. Immediately after the injury occurs, blood vessels constrict, and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors form clots that stop the bleeding and act as a barrier to prevent bacterial contamination. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[3],[4]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. The inflammatory process appears to the observer as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound, also commonly called pus.[5],[6]
The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[7],[8]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is also moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue referred to as biofilm that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected. The provider can then prescribe appropriate antibiotic treatment based on the culture results.[9]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 20.2[11] for an image of a surgical wound healing by primary intention.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. Wounds that heal by secondary intention are at higher risk for infection and must be protected from contamination. See Figure 20.3[12] for an image of a wound healing by secondary intention.

Tertiary intention refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.
Wound Closures
Lacerations and surgical wounds are typically closed with sutures, staples, or dermabond to facilitate healing by primary intention. See Figure 20.4[13] for an image of sutures, Figure 20.5[14] for an image of staples, and Figure 20.6[15] for an image of a wound closed with dermabond, a type of sterile surgical glue. Based on agency policy, the nurse may remove sutures and staples based on a provider order. See Figure 20.7[16] for an image of a disposable staple remover. See the checklists in the subsections later in this chapter for procedures related to surgical and staple removal.




Common Types of Wounds
There are several different types of wounds. It is important to understand different types of wounds when providing wound care because each type of wound has different characteristics and treatments. Additionally, treatments that may be helpful for one type of wound can be harmful for another type. Common types of wounds include skin tears, venous ulcers, arterial ulcers, diabetic foot wounds, and pressure injuries.[17]
Skin Tears
Skin tears are wounds caused by mechanical forces such as shear, friction, or blunt force. They typically occur in the fragile, nonelastic skin of older adults or in patients undergoing long-term corticosteroid therapy. Skin tears can be caused by the simple mechanical force used to remove an adhesive bandage or from friction as the skin brushes against a surface. Skin tears occur in the epidermis and dermis but do not extend through the subcutaneous layer. The wound bases of skin tears are typically fragile and bleed easily.[18]
Venous Ulcers
Venous ulcers are caused by lack of blood return to the heart causing pooling of fluid in the veins of the lower legs. The resulting elevated hydrostatic pressure in the veins causes fluid to seep out, macerate the skin, and cause venous ulcerations. Maceration refers to the softening and wasting away of skin due to excess fluid. Venous ulcers typically occur on the medial lower leg and have irregular edges due to the maceration. There is often a dark-colored discoloration of the lower legs, due to blood pooling and leakage of iron into the skin called hemosiderin staining. For venous ulcers to heal, compression dressings must be used, along with multilayer bandage systems, to control edema and absorb large amounts of drainage.[19] See Figure 20.8[20] for an image of a venous ulcer.

Arterial Ulcers
Arterial ulcers are caused by lack of blood flow and oxygenation to tissues. They typically occur in the distal areas of the body such as the feet, heels, and toes. Arterial ulcers have well-defined borders with a “punched out” appearance where there is a localized lack of blood flow. They are typically painful due to the lack of oxygenation to the area. The wound base may become necrotic (black) due to tissue death from ischemia. Wound dressings must maintain a moist environment, and treatment must include the removal of necrotic tissue. In severe arterial ulcers, vascular surgery may be required to reestablish blood supply to the area.[21] See Figure 20.9[22] for an image of an arterial ulcer on a patient’s foot.

Diabetic Ulcers
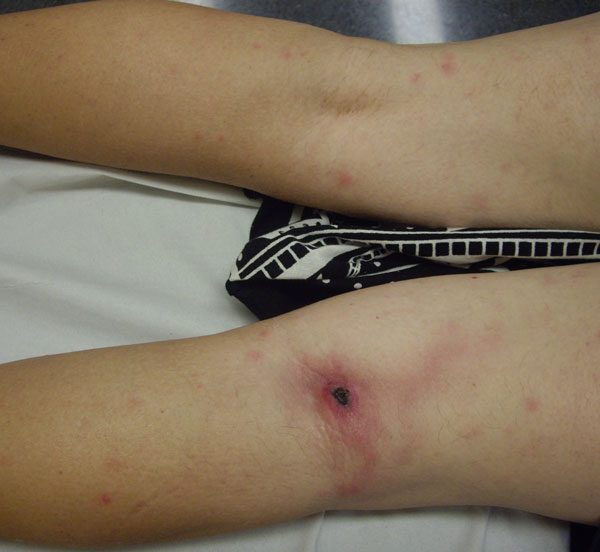
Diabetic ulcers are also called neuropathic ulcers because peripheral neuropathy is commonly present in patients with diabetes. Peripheral neuropathy is a medical condition that causes decreased sensation of pain and pressure, especially in the lower extremities. Diabetic ulcers typically develop on the plantar aspect of the feet and toes of a patient with diabetes due to lack of sensation of pressure or injury. See Figure 20.10[23] for an image of a diabetic ulcer. Wound healing is compromised in patients with diabetes due to the disease process. In addition, there is a higher risk of developing an infection that can reach the bone requiring amputation of the area. To prevent diabetic ulcers from occurring, it is vital for nurses to teach meticulous foot care to patients with diabetes and encourage the use of well-fitting shoes.[24]

Pressure Injuries
Pressure injuries are defined as “localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.”[25] Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer skin remains immobile because it remains attached to the sheets due to friction, but deeper tissue attached to the bone moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then impacts the blood flow and oxygenation of the surrounding tissues.
Braden Scale
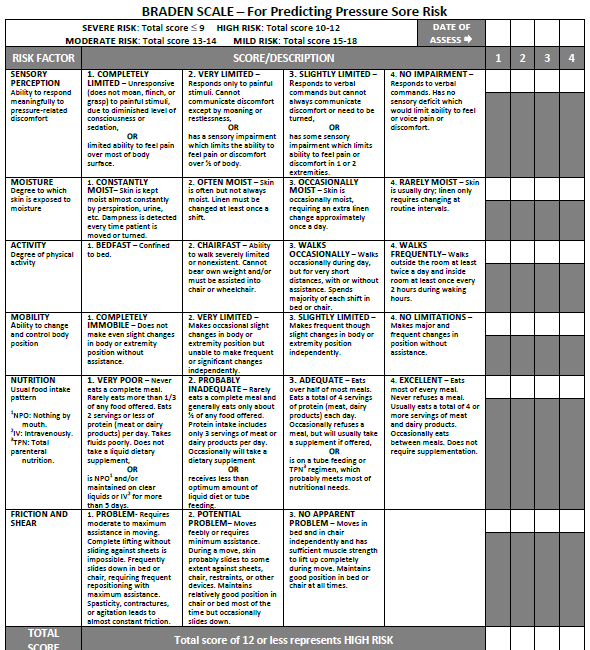
Several factors place a patient at risk for developing pressure injuries, including nutrition, mobility, sensation, and moisture. The Braden Scale is a tool commonly used in health care to provide an objective assessment of a patient’s risk for developing pressure injuries. See Figure 20.11[26] for an image of a Braden Scale. The six risk factors included on the Braden Scale are sensory perception, moisture, activity, mobility, nutrition, and friction/shear, and these factors are rated on a scale from 1-4 with 1 being “completely limited” to 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a patient’s risk for developing a pressure injury. A total score of 15-19 indicates mild risk, 13-14 indicates moderate risk, 10-12 indicates high risk, and less than or equal to 9 indicates severe risk. Nurses create care plans using these scores to plan interventions that prevent or treat pressure injuries.
For more information about using the Braden Scale, go to the “Integumentary” chapter of the Open RN Nursing Fundamentals textbook.
Staging
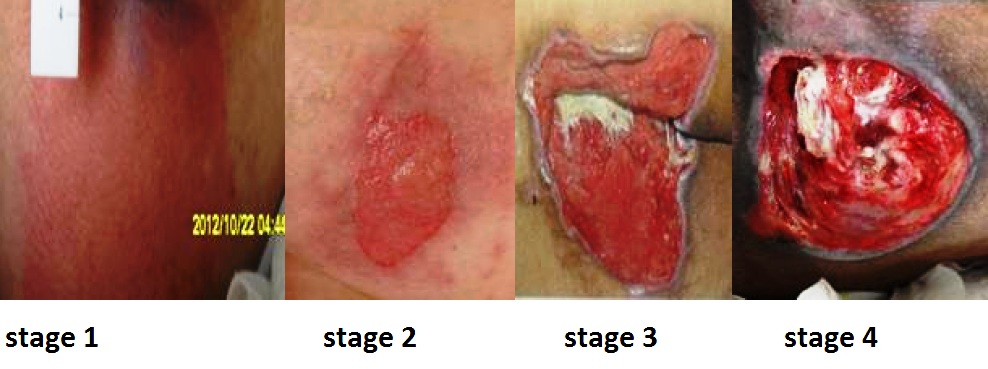
Pressure injuries commonly occur on the sacrum, heels, ischial tuberosity, and coccyx. The 2016 National Pressure Ulcer Advisory Panel (NPUAP) Pressure Injury Staging System now uses the term “pressure injury” instead of pressure ulcer because an injury can occur without an ulcer present. Pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have reddened but intact skin, and Stage 4 pressure injuries have deep, open ulcers affecting underlying tissue and structures such as muscles, ligaments, and tendons. See Figure 20.12[27] for an image of the four stages of pressure injuries.[28] The NPUAP’s definitions of the four stages of pressure injuries are described below:
- Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe skin redness that does not turn white when pressed.
- Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation.[29]
- Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Tunneling refers to passageways underneath the surface of the skin that extend from a wound and can take twists and turns. Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is an inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. See Figure 20.13 [30] for an image of eschar in the center of the wound. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[31] In most wounds, slough and eschar must be removed by debridement for healing to occur.
- Stage 4 pressure injuries are full-thickness tissue loss like Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may be present.[32]
View a supplementary YouTube video on Pressure Injuries[33]
Factors Affecting Wound Healing
Multiple factors affect a wound’s ability to heal and are referred to as local and systemic factors. Local factors refer to factors that directly affect the wound, whereas systemic factors refer to the overall health of the patient and their ability to heal. Local factors include localized blood flow and oxygenation of the tissue, the presence of infection or a foreign body, and venous sufficiency. Venous insufficiency is a medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs.[34]
Systemic factors that affect a patient’s ability to heal include nutrition, mobility, stress, diabetes, age, obesity, medications, alcohol use, and smoking.[35] When a nurse is caring for a patient with a wound that is not healing as anticipated, it is important to further assess for the potential impact of these factors:
- Nutrition. Nutritional deficiencies can have a profound impact on healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation is recommended daily.[36] In addition, vitamin C and zinc deficiency have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[37]
- Stress. Stress causes an impaired immune response that results in delayed wound healing. Although a patient cannot necessarily control the amount of stress in their life, it is possible to control one’s reaction to stress with healthy coping mechanisms. The nurse can help educate the patient about healthy coping strategies.
- Diabetes. Diabetes causes delayed wound healing due to many factors such as neuropathy, atherosclerosis (a buildup of plaque that obstructs blood flow in the arteries resulting in decreased oxygenation of tissues), a decreased host immune resistance, and increased risk for infection.[38] Read more about neuropathy and diabetic ulcers under the “Common Types of Wounds” subsection. Nurses provide vital patient education to patients with diabetes to effectively manage the disease process for improved wound healing.
- Age. Older adults have an altered inflammatory response that can impair wound healing. Nurses can educate patients about the importance of exercise for improved wound healing in older adults.[39]
- Obesity. Obese individuals frequently have wound complications, including infection, dehiscence, hematoma formation, pressure injuries, and venous injuries. Nurses can educate patients about healthy lifestyle choices to reduce obesity in patients with chronic wounds.[40]
- Medications. Medications such as corticosteroids impair wound healing due to reduced formation of granulation tissue.[41] When assessing a chronic wound that is not healing as expected, it is important to consider the side effects of the patient’s medications.
- Alcohol consumption. Research shows that exposure to alcohol impairs wound healing and increases the incidence of infection.[42] Patients with impaired healing of chronic wounds should be educated to avoid alcohol consumption.
- Smoking. Smoking impacts the inflammatory phase of the wound healing process, resulting in poor wound healing and an increased risk of infection.[43] Patients who smoke should be encouraged to stop smoking.
Lab Values Affecting Wound Healing
When a chronic wound is not healing as expected, laboratory test results may provide additional clues regarding the causes of the delayed healing. See Table 20.2 for lab results that offer clues to systemic issues causing delayed wound healing.[44]
Table 20.2 Lab Values Associated with Delayed Wound Healing[45]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets are important during the proliferative phase in the creation of granulation tissue and angiogenesis.[46] |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information, including the type and number of bacteria present, as well as identifying antibiotics to which the bacteria is susceptible. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Wound Complications
In addition to delayed wound healing, several other complications can occur. Three common complications are the development of a hematoma, infection, or dehiscence. These complications should be immediately reported to the health care provider.
Hematoma
A hematoma is an area of blood that collects outside of the larger blood vessels. A hematoma is more severe than ecchymosis (bruising) that occurs when small veins and capillaries under the skin break. The development of a hematoma at a surgical site can lead to infection and incisional dehiscence.[47] See Figure 20.14[48] for an image of a hematoma.

Infection
A break in the skin allows bacteria to enter and begin to multiply. Microbial contamination of wounds can progress from localized infection to systemic infection, sepsis, and subsequent life- and limb-threatening infection. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Purulent or malodorous drainage may also be present. Signs that a systemic infection is developing and requires urgent medical management include the following[49]:
- Fever over 101 F (38 C)
- Overall malaise (lack of energy and not feeling well)
- Change in level of consciousness/increased confusion
- Increasing or continual pain in the wound
- Expanding redness or swelling around the wound
- Loss of movement or function of the wounded area
Dehiscence
Dehiscence refers to the separation of the edges of a surgical wound. A dehisced wound can appear fully open where the tissue underneath is visible, or it can be partial where just a portion of the wound has torn open. Wound dehiscence is always a risk in a surgical wound, but the risk increases if the patient is obese, smokes, or has other health conditions, such as diabetes, that impact wound healing. Additionally, the location of the wound and the amount of physical activity in that area also increase the chances of wound dehiscence.[50] See Figure 20.15[51] for an image of dehiscence in an abdominal surgical wound in a 50-year-old obese female with a history of smoking and malnutrition.
Wound dehiscence can occur suddenly, especially in abdominal wounds when the patient is coughing or straining. Evisceration is a rare but severe surgical complication when dehiscence occurs, and the abdominal organs protrude out of the incision. Signs of impending dehiscence include redness around the wound margins and increasing drainage from the incision. The wound will also likely become increasingly painful. Suture breakage can be a sign that the wound has minor dehiscence or is about to dehisce.[52]
To prevent wound dehiscence, surgical patients must follow all post-op instructions carefully. The patient must move carefully and protect the skin from being pulled around the wound site. They should also avoid tensing the muscles surrounding the wound and avoid heavy lifting as advised.[53]

Media Attributions
- DSC_1036
- DSC_0345
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “417 Tissue Repair.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Alhajj, Bansal, and Goyal and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- “Ventriculoperitoneal shunt - surgical wound healing - belly - day 12.jpg” by Hansmuller is licensed under CC BY-SA 4.0 ↵
- “Atrophied skin.png” by sansea2 is licensed under CC BY-SA 3.0 ↵
- “Wound closed with surgical sutures.jpg” by Wikip2011 is licensed under CC BY-SA 3.0 ↵
- “Surgical staples1.jpg” by Llywrch is licensed under CC BY-SA 2.5 ↵
- “Incision wound on child's arm, closed with Dermabond.jpg” by ragesoss is licensed under CC BY-SA 3.0 ↵
- “Not quite scissors - TROML - 1366” by Clint Budd is licensed under CC BY 2.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Úlceras_antes_da_cirurgia.JPG” by Nini00 is licensed under CC BY-SA 3.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Arterial ulcer peripheral vascular disease.jpg” by Jonathan Moore is licensed under CC BY 3.0 ↵
- “Diabetic Planta ulcer.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://journals.lww.com/jwocnonline/Fulltext/2016/11000/Revised_National_Pressure_Ulcer_Advisory_Panel.3.aspx ↵
- The Braden Scale, from Prevention Plus, is included on the basis of Fair Use. ↵
- “Wound stage.jpg” by Babagolzadeh is licensed under CC BY-SA 3.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "Inoculation_eschar_Rickettsia_sibirica_mongolitimonae_infection.jpg" by José M. Ramos, Isabel Jado, Sergio Padilla, Mar Masiá, Pedro Anda, and Félix Gutiérrez is licensed under CC0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- RegisteredNurseRN. (2018, March 7). Pressure ulcers (injuries) stages, prevention, assessment | Stage 1, 2, 3, 4 unstageable NCLEX [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/MDtPik1UE6k ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah is licensed under CC BY 4.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/won.0000000000000281 ↵
- “Ankle swell and internal bleeding” by Glen Bowman is licensed under CC BY-SA 2.0 ↵
- WoundSource. (2016, October 19). 8 signs of wound infection. https://www.woundsource.com/blog/8-signs-wound-infection ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- “Bogota bag.png” by Suarez-Grau, J. M., Guadalajara Jurado, J. F., Gómez Menchero, J., Bellido Luque, J. A. is licensed under CC BY 4.0 ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
Headache
A headache is a common type of pain that patients experience in everyday life and a major reason for missed time at work or school. Headaches range greatly in severity of pain and frequency of occurrence. For example, some patients experience mild headaches once or twice a year, whereas others experience disabling migraine headaches more than 15 days a month. Severe headaches such as migraines may be accompanied by symptoms of nausea or increased sensitivity to noise or light. Primary headaches occur independently and are not caused by another medical condition. Migraine, cluster, and tension-type headaches are types of primary headaches. Secondary headaches are symptoms of another health disorder that causes pain-sensitive nerve endings to be pressed on or pulled out of place. They may result from underlying conditions including fever, infection, medication overuse, stress or emotional conflict, high blood pressure, psychiatric disorders, head injury or trauma, stroke, tumors, and nerve disorders such as trigeminal neuralgia, a chronic pain condition that typically affects the trigeminal nerve on one side of the cheek.[1]
Not all headaches require medical attention, but some types of headaches can signify a serious disorder and require prompt medical care. Symptoms of headaches that require immediate medical attention include a sudden, severe headache unlike any the patient has ever had; a sudden headache associated with a stiff neck; a headache associated with convulsions, confusion, or loss of consciousness; a headache following a blow to the head; or a persistent headache in a person who was previously headache free.[2]
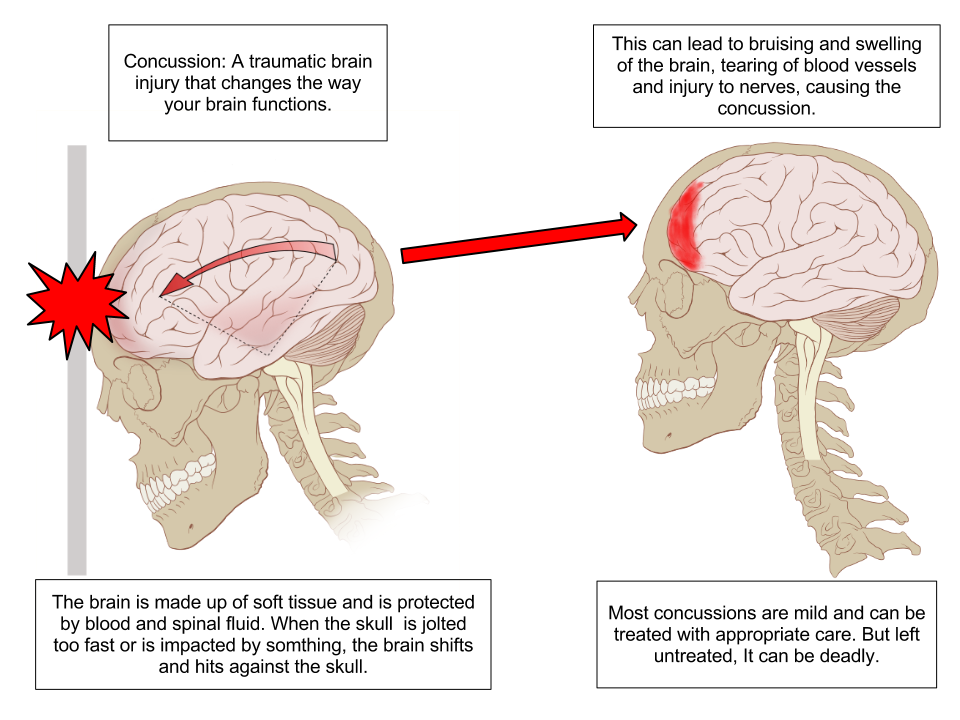
Concussion
A concussion is a type of traumatic brain injury caused by a blow to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement causes the brain to bounce around in the skull, creating chemical changes in the brain and sometimes damaging brain cells.[3] See Figure 7.14[4] for an illustration of a concussion.
Review of Concussions on YouTube[5]
A person who has experienced a concussion may report the following symptoms:
- Headache or “pressure” in head
- Nausea or vomiting
- Balance problems or dizziness or double or blurry vision
- Light or noise sensitivity
- Feeling sluggish, hazy, foggy, or groggy
- Confusion, concentration, or memory problems
- Just not “feeling right” or “feeling down”[6]
The following signs may be observed in someone who has experienced a concussion:
- Can’t recall events prior to or after a hit or fall
- Appears dazed or stunned
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent
- Moves clumsily
- Answers questions slowly
- Loses consciousness (even briefly)
- Shows mood, behavior, or personality changes[7]
Anyone suspected of experiencing a concussion should immediately be seen by a health care provider or go to the emergency department for further testing.
Read more information about concussion signs and symptoms on the CDC's Concussion Signs and Symptoms webpage.
Head Injury
Head and traumatic brain injuries are major causes of immediate death and disability. Falls are the most common cause of head injuries in young children (ages 0–4 years), adolescents (15–19 years), and the elderly (over 65 years). Strong blows to the brain case of the skull can produce fractures resulting in bleeding inside the skull. A blow to the lateral side of the head may fracture the bones of the pterion. If the underlying artery is damaged, bleeding can cause the formation of a hematoma (collection of blood) between the brain and interior of the skull. As blood accumulates, it will put pressure on the brain. Symptoms associated with a hematoma may not be apparent immediately following the injury, but if untreated, blood accumulation will continue to exert increasing pressure on the brain and can result in death within a few hours.[8]
See Figure 7.15[9] for an image of an epidural hematoma indicated by a red arrow associated with a skull fracture.

Sinusitis
Sinusitis is the medical diagnosis for inflamed sinuses that can be caused by a viral or bacterial infection. When the nasal membranes become swollen, the drainage of mucous is blocked and causes pain.
There are several types of sinusitis, including these types:
- Acute Sinusitis: Infection lasting up to 4 weeks
- Chronic Sinusitis: Infection lasting more than 12 weeks
- Recurrent Sinusitis: Several episodes of sinusitis within a year
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Health care providers diagnose sinusitis based on symptoms and an examination of the nose and face. Treatments include antibiotics, decongestants, and pain relievers.[10]
Pharyngitis
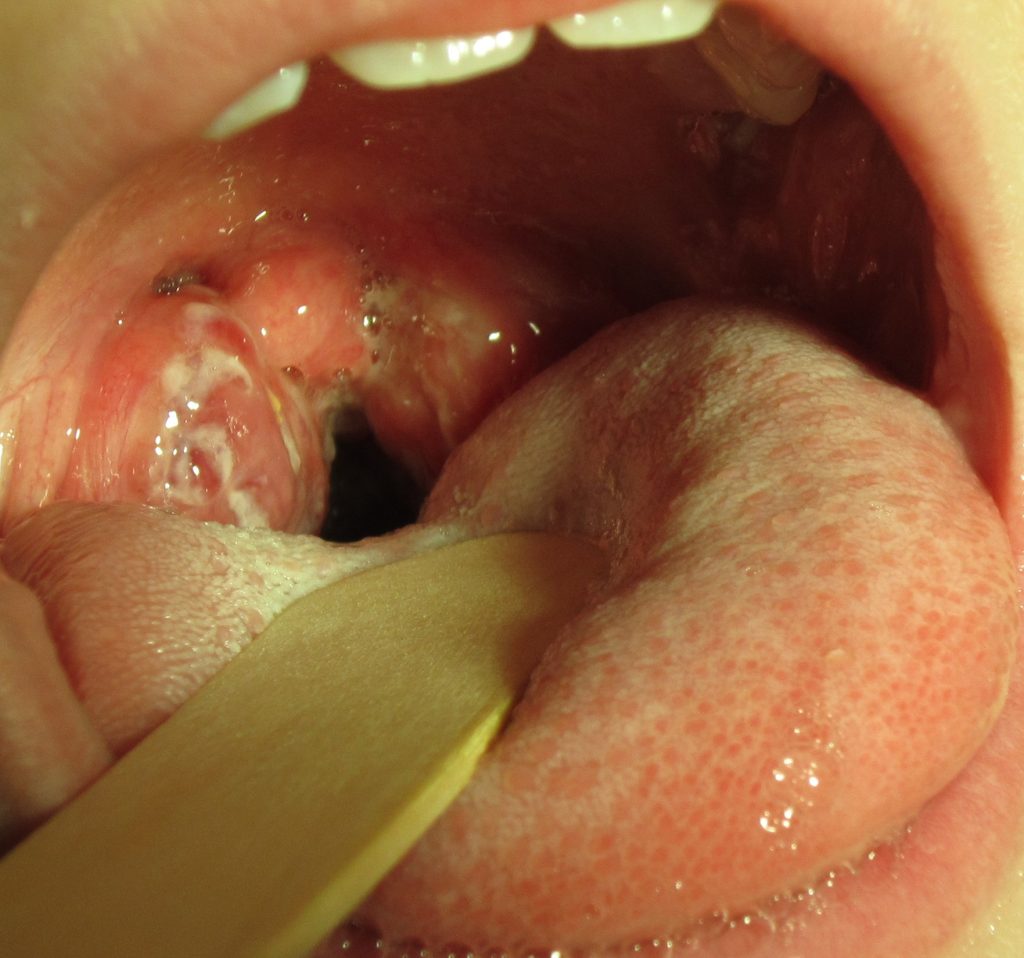
PharynPharyngitisgitis is the medical term used for infection and/or inflammation in the back of the throat (pharynx). Common causes of pharyngitis are the cold viruses, influenza, strep throat caused by group A streptococcus, and mononucleosis. Strep throat typically causes white patches on the tonsils with a fever and enlarged lymph nodes. It must be treated with antibiotics to prevent potential complications in the heart and kidneys. See Figure 7.16[11] for an image of strep throat in a child.
If not diagnosed as strep throat, most cases of pharyngitis are caused by viruses, and the treatment is aimed at managing the symptoms. Nurses can teach patients the following ways to decrease the discomfort of a sore throat:
- Drink soothing liquids such as lemon tea with honey or ice water.
- Gargle several times a day with warm salt water made of 1/2 tsp. of salt in 1 cup of water.
- Suck on hard candies or throat lozenges.
- Use a cool-mist vaporizer or humidifier to moisten the air.
- Try over-the-counter pain medicines, such as acetaminophen.[12]
Epistaxis, the medical term for a nosebleed, is a common problem affecting up to 60 million Americans each year. Although most cases of epistaxis are minor and manageable with conservative measures, severe cases can become life-threatening if the bleeding cannot be stopped.[13] See Figure 7.17[14] for an image of a severe case of epistaxis.

The most common cause of epistaxis is dry nasal membranes in winter months due to low temperatures and low humidity. Other common causes are picking inside the nose with fingers, trauma, anatomical deformity, high blood pressure, and clotting disorders. Medications associated with epistaxis are aspirin, clopidogrel, nonsteroidal anti-inflammatory drugs, and anticoagulants.[15]
To treat a nosebleed, have the victim lean forward at the waist and pinch the lateral sides of the nose with the thumb and index finger for up to 15 minutes while breathing through the mouth.[16] Continued bleeding despite this intervention requires urgent medical intervention such as nasal packing.
Cleft Lip and Palate
During embryonic development, the right and left maxilla bones come together at the midline to form the upper jaw. At the same time, the muscle and skin overlying these bones join together to form the upper lip. Inside the mouth, the palatine processes of the maxilla bones, along with the horizontal plates of the right and left palatine bones, join together to form the hard palate. If an error occurs in these developmental processes, a birth defect of cleft lip or cleft palate may result.
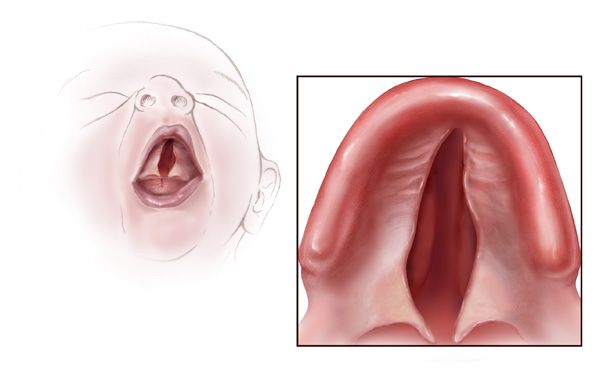
Cleft lip is a common developmental defect that affects approximately 1:1,000 births, most of which are male. This defect involves a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a cleft (gap). See Figure 7.18[17] for an image of an infant with a cleft lip.

A more severe developmental defect is a cleft palate that affects the hard palate, the bony structure that separates the nasal cavity from the oral cavity. See Figure 7.19[18] for an illustration of a cleft palate. Cleft palate affects approximately 1:2,500 births and is more common in females. It results from a failure of the two halves of the hard palate to completely come together and fuse at the midline, thus leaving a gap between the nasal and oral cavities. In severe cases, the bony gap continues into the anterior upper jaw where the alveolar processes of the maxilla bones also do not properly join together above the front teeth. If this occurs, a cleft lip will also be seen. Because of the communication between the oral and nasal cavities, a cleft palate makes it very difficult for an infant to generate the suckling needed for nursing, thus creating risk for malnutrition. Surgical repair is required to correct a cleft palate.[19]
Poor Oral Health
Despite major improvements in oral health for the population as a whole, oral health disparities continue to exist for many racial, ethnic, and socioeconomic groups in the United States. Healthy People 2020, a nationwide initiative geared to improve the health of Americans, identified improved oral health as a health care goal. A growing body of evidence has also shown that periodontal disease is associated with negative systemic health consequences. Periodontal diseases are infections and inflammation of the gums and bone that surround and support the teeth. Red, swollen, and bleeding gums are signs of periodontal disease. Other symptoms of periodontal disease include bad breath, loose teeth, and painful chewing.[20] In 2020, the Centers for Disease Control and Prevention (CDC) reported that 42% of U.S. adults have some form of periodontitis, and almost 60% of adults aged 65 and older have periodontitis. See Figure 7.20[21] for an image of a patient with periodontal disease. Nurses may encounter patients who complain of bleeding gums, or they may discover other signs of periodontal disease during a physical assessment.

Because many Americans lack access to oral care, it is important for nurses to perform routine oral assessment and identify needs for follow-up. If signs and/or symptoms indicate potential periodontal disease, the patient should be referred to a dental health professional for a more thorough evaluation.[22]
Thrush/Candidiasis
Candidiasis is a fungal infection caused by Candida. Candida normally lives on the skin and inside the body without causing any problems, but it can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages fungal growth.[23] See Figure 7.21[24] for an image of candidiasis.

Candidiasis in the mouth and throat can have many symptoms, including the following:
- White patches on the inner cheeks, tongue, roof of the mouth, and throat
- Redness or soreness
- Cotton-like feeling in the mouth
- Loss of taste
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth[25]
Candidiasis in the mouth or throat is common in babies but is uncommon in healthy adults. Risk factors for getting candidiasis as an adult include the following:
- Wearing dentures
- Diabetes
- Cancer
- HIV/AIDS
- Taking antibiotics or corticosteroids including inhaled corticosteroids for conditions like asthma
- Taking medications that cause dry mouth or have medical conditions that cause dry mouth
- Smoking
The treatment for mild to moderate cases of candidiasis infections in the mouth or throat is typically an antifungal medicine applied to the inside of the mouth for 7 to 14 days, such as clotrimazole, miconazole, or nystatin.
"Meth Mouth"
The use of methamphetamine (i.e., meth), a strong stimulant drug, has become an alarming public health issue in the United States. A common sign of meth abuse is extreme tooth and gum decay often referred to as “Meth Mouth.” See Figure 7.22[26] for an image of Meth Mouth.

Signs of Meth Mouth include the following:
- Dry Mouth. Methamphetamines dry out the salivary glands, and the acid content in the mouth will start to destroy the enamel on the teeth. Eventually this will lead to cavities.
- Cracked Teeth. Methamphetamine can make the user feel anxious, hyper, or nervous, so they clench or grind their teeth. You may see severe wear patterns on their teeth.
- Tooth Decay. Methamphetamine users crave beverages high in sugar while they are “high.” The bacteria that feed on the sugars in the mouth will secrete acid, which can lead to more tooth destruction. With methamphetamine users, tooth decay will start at the gum line and eventually spread throughout the tooth. The front teeth are usually destroyed first.
- Gum Disease. Methamphetamine users do not seek out regular dental treatment. Lack of oral health care can contribute to periodontal disease. Methamphetamines also cause the blood vessels that supply the oral tissues to shrink in size, reducing blood flow, causing the tissues to break down.
- Lesions. Users who smoke methamphetamine may present with lesions and/or burns on their lips or gingival inside the cheeks or on the hard palate. Users who snort may present with burns in the back of their throats.[27]
Nurses who notice possible signs of "Meth Mouth" should report their concerns to the health care provider, not only for a referral for dental care, but also for treatment of suspected substance abuse.
Dysphagia
Dysphagia is the medical term for difficulty swallowing that can be caused by many medical conditions. Nurses are often the first health care professionals to notice a patient’s difficulty swallowing as they administer medications or monitor food intake. Early identification of dysphagia, especially after a patient has experienced a cerebrovascular accident (i.e., stroke) or other head injury, helps to prevent aspiration pneumonia.[28]
Aspiration pneumonia is a type of lung infection caused by material from the stomach or mouth entering the lungs and can be life-threatening.
Signs of dysphagia include the following:
- Coughing during or right after eating or drinking
- Wet or gurgly sounding voice during or after eating or drinking
- Extra effort or time required to chew or swallow
- Food or liquid leaking from mouth
- Food getting stuck in the mouth
- Difficulty breathing after meals[29]
The Barnes-Jewish Hospital-Stroke Dysphagia Screen (BJH-SDS) is an example of a simple, evidence-based bedside screening tool that can be used by nursing staff to efficiently identify swallowing impairments in patients who have experienced a stroke. See internet resource below for an image of the dysphagia screening tool. The result of the screening test is recorded as a “fail” if any of the five items tested are abnormal (Glasgow Coma Scale < 13, facial/tongue/palatal asymmetry or weakness, or signs of aspiration on the 3-ounce water test) or “pass” if all five items tested were normal. Patients with a failed screening result are placed on nothing-by-mouth (NPO) status until further evaluation is completed by a speech therapist. For more information about using the Glasgow Coma Scale, see the "Assessing Mental Status" section in the “Neurological Assessment” chapter.
View a PDF sample of a Nursing Bedside Swallow Screen.
Enlarged Lymph Nodes
Lymphadenopathy is the medical term for swollen lymph nodes. In a child, a node is considered enlarged if it is more than 1 centimeter (0.4 inch) wide. See Figure 7.23[30] for an image of an enlarged cervical lymph node.

Common infections such as a cold, pharyngitis, sinusitis, mononucleosis, strep throat, ear infection, or infected tooth often cause swollen lymph nodes. However, swollen lymph nodes can also signify more serious conditions. Notify the health care provider if the patient’s lymph nodes have the following characteristics:
- Do not decrease in size after several weeks or continue to get larger
- Are red and tender
- Feel hard, irregular, or fixed in place
- Are associated with night sweats or unexplained weight loss
- Are larger than 1 centimeter in diameter
The health care provider may order blood tests, a chest X-ray, or a biopsy of the lymph node if these signs occur.[31]
Thyroid
The thyroid is a butterfly-shaped gland located at the front of the neck that controls many of the body’s important functions. The thyroid gland makes hormones that affect breathing, heart rate, digestion, and body temperature. If the thyroid makes too much or not enough thyroid hormone, many body systems are affected. In hypothyroidism, the thyroid gland doesn’t produce enough hormone and many body functions slow down. When the thyroid makes too much hormone, a condition called hyperthyroidism, many body systems speed up.[32]
A
- Evidence-based practice (EBP)
-
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies, theories, clinical expertise, health care resources, and patient preferences and values.
- ABCDE
-
A mnemonic for assessing melanoma developing in moles: Asymmetrical, Borders are irregular in shape, Color is various shades of brown or black, Diameter is larger than 6 mm., and the shape of the mole is Evolving.
- belief
- Cultural humility
-
Defined by the American Nurses Association as, "A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases" realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process
- dislocation
-
A joint injury that forces the ends of bones out of position; often caused by a fall or a blow to the joint.
- Inspection
- Kyphosis
-
Outward curvature of the back; often described as “hunchback”.
- Melanin
-
Skin pigment produced by melanocytes scattered throughout the epidermis.
- Mobility
- obstructive sleep apnea (OSA)
-
Cessation of breathing while sleeping and is caused by the partial or full collapse of the airway as muscles relax during sleep.
- Osteoporosis
-
A disease that thins and weakens bones, especially in the hip, spine, and wrist, causing them to become fragile and break easily.
- Scoliosis
-
A sideways curve of the spine that commonly develops in late childhood and the early teens.
- value
- [pb_glossary id="643"]Nursing Practice Act[/pb_glossary
-
The Nurse Practice Act is enacted by that state's legislature, defines the scope of practice for nurses in that state, and establishes regulations for nursing practice.
- ABCDE
-
A mnemonic for assessing melanoma developing in moles: Asymmetrical, Borders are irregular in shape, Color is various shades of brown or black, Diameter is larger than 6 mm., and the shape of the mole is Evolving.
- Abduction
-
Joint movement away from the midline of the body.
- accessory muscles
-
Muscles other than the diaphragm and intercostal muscles that may be used for labored breathing.
- Active assist range of motion
-
A patient’s joint receiving partial assistance in movement from an outside force.
- active listening
-
Process by which we are communicating verbally and nonverbally that we are interested in what the other person is saying while also actively verifying our understanding with the speaker.
- Active range of motion
-
Movement of a joint by the individual performing the exercise.
- Active transport
-
Movement of solutes and ions across a cell membrane against a concentration gradient from an area of lower concentration to an area of higher concentration using energy during the process.
- Acute grief
-
Grief that begins immediately after the death of a loved one and includes the separation response and response to stress.
- Acute pain
-
Pain that is limited in duration and is associated with a specific cause.
- Acute, self-limiting infections
-
Infections that develop rapidly and generally last only 10-14 days.
- Addiction
-
A term used in many countries to describe severe problems related to compulsive and habitual use of substances.
- Adduction
-
Joint movement toward the middle line of the body.
- adhesion
-
Capability of pathogenic microbes to attach to the cells of the body.
- adjuvant
-
Medication that is not classified as an analgesic but has been found in clinical practice to have either an independent analgesic effect or additive analgesic properties when administered with opioids.
- ADOPIE
-
An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
- Adult day centers
-
Care that offers people with dementia and other chronic illnesses the opportunity to be social and to participate in activities in a safe environment, while also giving their caregivers the opportunity to work, run errands, or take a much-needed break.
- Advance directives
-
Legal documents that direct care when the patient can no longer speak from themselves, including the living will and the health care power of attorney.
- Advanced Practice Nurses
-
An RN who has a graduate degree and advanced knowledge. There are four categories of APRNs: certified nurse-midwife (CNM), clinical nurse specialist (CNS), certified nurse practitioner (CNP), or certified registered nurse anesthetist (CRNA). These nurses can diagnose illnesses and prescribe treatments and medications.
- Advocacy
-
The act or process of pleading for, supporting, or recommending a cause or course of action.
- Ageism
-
The stereotyping and discrimination against individuals or groups on the basis of their age.
- airborne precautions
- Alzheimer’s disease
-
An irreversible, progressive brain disorder that slowly destroys memory and thinking skills and eventually the ability to carry out the simplest tasks.
- Ambulation
-
The ability of a patient to safely walk independently, with assistance from another person, or with an assistive device, such as a cane, walker, or crutches.
- ANA Standards of Professional Nursing Practice
-
Authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.
- ANA Standards of Professional Performance
-
12 additional standards that describe a nurse's professional behavior, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health.
- analgesics
-
Different types of pain medications
- angiogenesis
-
The process of wound healing when new capillaries begin to develop within the wound 24 hours after injury to bring in more oxygen and nutrients for healing.
- Anorexia
-
Loss of appetite or loss of desire to eat.
- antibodies
-
Y proteins created by B cells that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells.
- Anticipatory grief
-
Grief before a loss, associated with diagnosis of an acute, chronic, and/or terminal illness experienced by the patient, family, and caregivers.
- Anuria
-
Absence of urine output that is typically found during kidney failure. Can be defined as less than 50 mL of urine over a 24-hour period.
- Aphasia
-
A communication disorder that results from damage to portions of the brain that are responsible for language.
- Apocrine sweat glands
-
Sweat glands associated with hair follicles in densely hairy areas that release organic compounds subject to bacterial decomposition causing odor.
- approximated edges
-
The well-closed edges of a wound healing by primary intention.
- art of nursing
-
Defined as, "Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."
- Arterial insufficiency
-
A condition caused by lack of adequately oxygenated blood supply to specific tissues.
- Arthroplasty
-
Joint replacement surgery.
- Arthroscopic surgery
-
A surgical procedure involving a small incision and the insertion of an arthroscope, a pencil-thin instrument that allows for visualization of the joint interior. Small surgical instruments are inserted via additional incisions to remove or repair ligaments and other joint structures.
- Articular cartilage
-
Smooth, white tissue that covers the ends of bones where they come together at joints, allowing them to glide over each other with very little friction. Articular cartilage can be damaged by injury or normal wear and tear.
- asepsis
-
A state of being free of disease-causing microorganisms.
- Aseptic non-touch technique
-
A standardized technique, supported by evidence, to maintain asepsis and standardize practice.
- aseptic technique
-
The purposeful reduction of pathogens to prevent the transfer of microorganisms from one person or object to another during a medical procedure.
- Aspiration pneumonia
-
A type of lung infection caused by material from the stomach or mouth inadvertently entering the lungs that can be life-threatening.
- Assertive communication
-
A way to convey information that describes the facts, the sender’s feelings, and explanations without disrespecting the receiver’s feelings. This communication is often described as using “I” messages: “I feel…,” “I understand…,” or “Help me to understand…”.
- Assimilation
-
The process whereby a member of a cultural group adopts or conforms with the practices, habits, and norms of another group, usually a dominant group. As a result, the person gradually takes on a new cultural identity, often losing their original identity in the process.
- assistive device
-
An object or piece of equipment designed to help a patient with activities of daily living, such as a walker, cane, gait belt, or mechanical lift.
- Associated Conditions
-
Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis.
- At-risk behavior
-
According to the just culture model, an error that occurs when a behavioral choice is made that increases risk where risk is not recognized or is mistakenly believed to be justified.
- at-risk populations
-
Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
- Auscultation
- B cells
-
Immune cells that mature in the bone marrow and produce antibodies.
- bacteremia
-
The presence of bacteria in blood.
- barrel chest
-
An increased anterior-posterior chest diameter, resulting from air trapping in the alveoli, that occurs in chronic respiratory disease.
- barrel chest.
-
An increased anterior-posterior chest diameter, resulting from air trapping in the alveoli, that occurs in chronic respiratory disease.
- Basic Nursing Care
-
Care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
- Bed Mobility
-
The ability of a patient to move around in bed, including moving from lying to sitting and sitting to lying.
- bedside handoff reports
-
A handoff report in hospitals that involves patients, their family members, and both the off-going and the oncoming nurses. The report is performed face to face and conducted at the patient's bedside.
- behavioral restraints
-
Restraints used to manage violent, self-destructive behaviors such as hitting or kicking staff or other clients, physically harming themselves or others, or threatening to do so. Behavioral restraints are used in emergency situations where safety concerns need to be immediately addressed to prevent harm.
- Bereavement
-
grief (the inner feelings) and mourning (the outward reactions) after a loved one has died.
- Bias
-
To carry an attitude, opinion, or inclination (positive or negative) towards a group or members of a group. Bias can be a conscious attitude (explicit) or a person may not be aware of their bias (implicit).
- Black stools
-
Black-colored stools can be caused by iron supplements or bismuth subsalicylate (Pepto-Bismol) taken for an upset stomach.
- Board of Nursing
-
The state-specific licensing and regulatory body that sets the standards for safe nursing care, decides the scope of practice for nurses within its jurisdiction, and issues licenses to qualified candidates.
- Body mechanics
-
The coordinated effort of muscles, bones, and the nervous system to maintain balance, posture, and alignment during moving, transferring, and repositioning patients.
- Bowel incontinence
-
The loss of bowel control, causing the unexpected passage of stool.
- Bowel retraining
-
Involves teaching the body to have a bowel movement at a certain time of the day.
- Braden Scale
-
A standardized assessment tool used to assess and document a patient’s risk factors for developing pressure injuries.
- Broca's aphasia
-
A type of aphasia where patients understand speech and know what they want to say, but frequently speak in short phrases that are produced with great effort. People with Broca's aphasia typically understand the speech of others fairly well. Because of this, they are often aware of their difficulties and can become easily frustrated.
- Burnout
-
Can be triggered by workplace demands, lack of resources to do work professionally and safely, interpersonal relationship stressors, or work policies that can lead to diminished caring and cynicism.
- cachexia
-
Wasting of muscle and adipose tissue due to lack of nutrition.
- calorie-dense
-
Foods with a substantial amount of calories and few nutrients.
- Candidiasis
-
A fungal infection often referred to as “thrush” when it occurs in the oral cavity in children.
- Carbohydrates
-
Sugars and starches that provide an important energy source, providing 4 kcal/g of energy.
- cardiac output
-
The amount of blood the heart pumps in one minute.
- cardiopulmonary resuscitation (CPR)
-
Emergency treatment provided when a patient's blood flow or breathing stops that may involve chest compressions and mouth-to-mouth breathing, electric shocks to stop lethal cardiac rhythms, breathing tubes to open the airway, or cardiac medications.
- care relationship
-
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family.
- Cataracts
-
Opacity of the lens of the eye that causes clouded, blurred, or dim vision.
- Certification
-
The formal recognition of specialized knowledge, skills, and experience demonstrated by the achievement of standards identified by a nursing specialty.
- chain of command
-
A hierarchy of reporting relationships in an agency that establishes accountability and lays out lines of authority and decision-making power.
- chain of infection
-
Also referred to as the chain of transmission, describes how an infection spreads based on these six links of transmission: infectious agent, reservoirs, portal of exit, modes of transmission, portal of entry, and susceptible host.
- chaplains
-
Trained professionals in hospitals, nursing homes, assisted living facilities, and hospices that assist with the spiritual, religious, and emotional needs of patients, families, and staff.
- Charting by exception (CBE)
-
A type of documentation where a list of “normal findings” are provided and nurses document assessment findings by confirming normal findings and writing brief documentation notes for any abnormal findings.
- chemical digestion
-
Breakdown of food with stomach acids, bile, and pancreatic enzymes for nutrient release.
- chemical restraint
-
A drug used to manage a patient’s behavior, restrict the patient’s freedom of movement, or impair the patient’s ability to appropriately interact with their surroundings that is not a standard treatment or dosage for the patient’s condition.
- chronic infections
-
Infections that may persist for months.
- Chronic pain
-
Pain that is ongoing and persistent for longer than six months.
- Chvostek’s sign
-
An assessment sign of acute hypocalcemia characterized by involuntary facial muscle twitching when the facial nerve is tapped.
- Circadian rhythms
-
Body rhythms that direct a wide variety of functions including wakefulness, body temperature, metabolism, and the release of hormones.
- Cleft lip
-
A birth defect caused by a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a gap in the lip.
- Cleft palate
-
A birth defect caused when two halves of the hard palate fail to completely come together and fuse at the midline, leaving a gap between them, and making it very difficult for an infant to generate the suckling needed for nursing.
- client
-
Individual, family, or group which includes significant others and populations.
- Clinical judgment
-
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.
- clinical reasoning
-
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.
- Clubfoot
-
A congenital condition that causes the foot and lower leg to turn inward and downward.
- clustering data
-
Organizing data into similar domains or patterns.
- clusters
-
Grouping data into similar domains or patterns.
- Coarse crackles
-
Low-pitched, loud, continuous sounds frequently heard on expiration.
- Code of Ethics for Nurses.
-
A code that applies normative, moral guidance for nurses in terms of what they ought to do, be, and seek.
- Cognition
-
A term used to describe our ability to think.
- Cognitive impairment
-
Impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge.
- Collaborative nursing interventions
-
Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP).
- Colostrum
-
A thick yellowish-white fluid rich in proteins and immunoglobulin A (IgA) and lower in carbohydrates and fat than mature breast milk secreted within the first 2-3 days after giving birth.
- Comfort care
-
Care that occurs when the patient’s and medical team’s goals shift from curative interventions to symptom control, pain relief, and quality of life.
- Compassion fatigue
-
A state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being.
- complete blood count (CBC)
-
The red blood cell count (RBC), white blood cell count (WBC), platelets, hemoglobin, and hematocrit values.
- Complete proteins
-
Proteins with enough amino acids in enough quantities to perform necessary functions such as growth and tissue maintenance.
- Complex carbohydrates
-
Larger molecules of polysaccharides that break down more slowly and release sugar into the bloodstream more slowly than simple carbohydrates.
- Complicated grief
-
Chronic grief, delayed grief, exaggerated grief, and masked grief are types of complicated grief.
- congenital condition
-
A condition present at birth.
- Constipation
-
A decrease in normal frequency of defecation accompanied by difficult or incomplete passage of stool and/or passage of excessively hard, dry stool.
- contact precautions
-
Infection prevention and control interventions to be used in addition to standard precautions for diseases spread by contact with the patient, their body fluids, or their surroundings, such as C-diff, MRSA, VRE, and RSV.
- contracture
-
A contracture is the lack of full passive range of motion due to joint, muscle, or soft tissue limitations.
- contrast
-
A special dye administered to patients before some diagnostic tests so that certain areas show up better on the X-rays.
- convalescent period
-
The final period of disease.
- Coordination of care
-
While implementing interventions during the nursing process, includes competencies such as organizing the plan, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team.
- Coughing and deep breathing
-
A breathing technique where the patient is encouraged to take deep, slow breaths and then exhale slowly.
- cranium
-
Area that surrounds and protects the brain that occupies the cranial cavity.
- Critical thinking
-
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.
- Cues
-
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
- Cultural awareness
-
A deliberate, cognitive process in which health care providers become appreciative and sensitive to the values, beliefs, lifeways, practices, and problem-solving strategies of a patient’s culture.
- Cultural competence
-
The process of applying evidence-based nursing in agreement with the preferred cultural values, beliefs, worldview, and practices of patients to produce improved patient outcomes.
- Cultural competence
-
A lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of clients to produce improved client outcomes
- cultural desire
-
Refers to the intrinsic motivation and commitment on the part of a nurse to develop cultural awareness and cultural competency.
- Cultural diversity
-
Cultural differences in people.
- cultural encounter
-
A process where the nurse directly engages in face-to-face cultural interactions and other types of encounters with clients from culturally diverse backgrounds in order to modify existing beliefs about a cultural group and to prevent possible stereotyping
- cultural humility
-
A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.
- Cultural knowledge
-
Seeking information about cultural health beliefs and values to understand patients’ world views.
- Cultural negotiation
-
A process where the patient and nurse seek a mutually acceptable way to deal with competing interests of nursing care, prescribed medical care, and the patient’s cultural needs.
- Cultural sensitivity
-
Being tolerant and accepting of cultural practices and beliefs of people.
- Cultural skill
-
The ability to gather and synthesize relevant cultural information about their patients while planning care and using culturally sensitive communication skills while doing so.
- Culturally congruent practice
-
Describes nursing care that is in agreement with the preferred values, beliefs, worldview, and practices of the health care consumer
- Culturally responsive care
-
Nursing actions that integrate a person’s cultural beliefs into their care.
- culturally safe environment
-
A safe space for patients to interact with health professionals, without judgment or discrimination, where the patient is free to express their cultural beliefs, values, and identity.
- Culture
-
A set of beliefs, attitudes, and practices shared by a group of people or community that are accepted, followed, and passed down to other members of the group.
- culture of safety
-
The behaviors, beliefs, and values within and across all levels of an organization as they relate to safety and clinical excellence, with a focus on people.
- Cyanosis
-
Bluish discoloration of the skin and mucous membranes.
- cytokine storm
-
Severe immune reaction in which the body releases too many cytokines into the blood too quickly.
- Cytokines
-
Proteins that affect interaction and communication between cells.
- DAR
-
A type of documentation often used in combination with charting by exception. DAR stands for Data, Action, and Response. Focused DAR notes are brief and each note is focused on one patient problem for efficiency in documenting, as well as for reading.
- Deductive reasoning
-
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
- Deep tissue pressure injuries
-
Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or non-intact skin revealing a dark wound bed or blood filled blister.
- Defining characteristics
-
Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the patient/family tells us), touched, or smelled.
- dehiscence
-
Separation of the edges of a surgical wound.
- Delegation
-
The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel while retaining accountability for the outcome.
- Delirium
-
An acute state of cognitive impairment that typically occurs suddenly due to a physiological cause, such as infection, hypoxia, electrolyte imbalances, drug effects, or other acute brain injury.
- Dementia
-
A chronic condition of impaired cognition, caused by brain disease or injury, marked by personality changes, memory deficits, and impaired reasoning.
- Dependent nursing interventions
-
Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant.
- Depression
-
A brain disorder with a variety of causes, including genetic, biological, environmental, and psychological factors.
- dermis
-
The layer of skin underneath under the epidermis, containing hair follicles, sebaceous glands, blood vessels, endocrine sweat glands, and nerve endings.
- Development
-
Biological changes, as well as social and cognitive changes, that occur continuously throughout our lives.
- Diabetic retinopathy
-
A complication of diabetes mellitus due to damaged blood vessels in the retina. If found early, treatments, such as laser treatment that can help shrink blood vessels, injections that can reduce swelling, or surgery, can prevent permanent vision loss.
- Diarrhea
-
More than three unformed stools in 24 hours.
- Dietary Reference Intakes
-
Set requirements or limit amounts of a certain nutrient, including protein, carbohydrates, fats, vitamins, minerals, and fiber.
- Diffusion
-
The movement of solute particles from an area of higher concentration to an area of lower concentration.
- Dimensional analysis
-
Dimensional analysis is a problem-solving technique where measurements are converted to a different (but equivalent) unit of measure by multiplying with a fractional form of 1 to obtain a desired unit of administration.
- Direct care
-
Interventions that are carried out by having personal contact with a patient.
- Discrimination
-
Unfair and different treatment of another person or group, denying them opportunities and rights to participate fully in society.
- disease
-
Signs and symptoms resulting in a deviation from the normal structure or functioning of the host.
- Disenfranchised grief
-
Any loss that is not validated or recognized.
- Disinfection
-
Removal of organisms from inanimate objects and surfaces.
- do-not-resuscitate (DNR) order
-
A medical order that instructs health care professionals not to perform cardiopulmonary resuscitation.
- Doff
-
To take off or remove personal protective equipment, such as gloves or a gown.
- Don
-
To put on equipment for personal protection, such as gloves or a gown.
- drop factor
-
The number of drops in one mL of solution when fluids or medications are administered using gravity IV tubing.
- droplet precautions
-
Infection prevention and control interventions to be used in addition to standard precautions; used for diseases spread by large respiratory droplets such as influenza, COVID-19, or pertussis.
- dysphagia
-
Impaired swallowing.
- Dyspnea
-
A subjective feeling of not getting enough air. Depending on severity, dyspnea causes increased levels of anxiety.
- Dysuria
-
Painful or difficult urination.
- eccrine sweat gland
-
Sweat gland that produces hypotonic sweat for thermoregulation.
- edema
-
Swelling.
- electronic health record (EHR)
-
A digital version of a patient’s paper chart. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users.
- Electronic Medical Record (EMR)
-
An electronic version of the patient’s medical record.
- enhanced barrier precautions
-
Enhanced Barrier Precautions are an infection control intervention designed to reduce transmission of multidrug-resistant organisms (MDRO’S) in nursing homes.
- Enteral nutrition
-
Liquid nutrition given through the gastrointestinal tract via a tube while bypassing chewing and swallowing.
- Enuresis
-
Incontinence when sleeping (i.e., bedwetting).
- epidermis
-
The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft.
- Epistaxis
-
Nosebleed.
- Epithelialization
-
The development of new epidermis and granulation tissue in a healing wound.
- Equivalency
-
Two values or quantities that are the same amount. For example, one cup is equivalent to eight ounces.
- erythema
-
Redness.
- Eschar
-
Dark brown/black, dry, thick, and leathery dead tissue in wounds.
- Essential nutrients
-
Nutrients that must be ingested from dietary intake. Essential nutrients cannot be synthesized by the body.
- ethical principle
-
A general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action
- Ethnocentrism
-
The belief that one’s culture (or race, ethnicity, or country) is better and preferable than another’s.
- Evidence-based practice
-
A lifelong problem solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health consumer’s history and condition, as well as healthcare resources; and patient, family, group, community, and population preferences and values.
- Excoriation
-
Redness and removal of the surface of the topmost layer of skin, often due to maceration or itching.
- Expected outcome
-
Statements of measurable action for the patient within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame.
- Expected outcomes
-
Expected outcomes.
- exposure
-
An encounter with a potential pathogen.
- expressive aphasia
-
The impaired ability to form words and speak.
- Extension
-
Joint movement causing the straightening of limbs (increase in angle) at a joint.
- Extracellular fluids (ECF)
-
Fluids found outside cells in the intravascular or interstitial spaces.
- Exudate
-
Fluid that oozes from a wound.
- Fading away
-
A transition that families make when they realize their seriously ill family member is dying.
- Fat-soluble vitamins
-
Vitamins that dissolve in fats and oils and are stored in fat tissue and can build up in the liver, resulting in toxicity.
- Fats
-
Fatty acids and glycerol that are essential for tissue growth, insulation, an energy source, energy storage, and hormone production.
- Fecal impaction
-
A condition that occurs when stool accumulates in the rectum usually due to the patient not feeling the presence of stool or not using the toilet when the urge is felt.
- Filtration
-
Movement of fluids through a permeable membrane utilizing hydrostatic pressure.
- Flexion
-
Joint movement causing the bending of the limbs (reduction of angle) at a joint.
- Fowler’s positioning
-
A position where the patient is supine with the head of bed placed at a 45- to 90-degree angle.
- fracture
-
A broken bone.
- Frequency
-
Urinary frequency is the need to urinate many times during the day or at night (nocturia) in normal or less-than-normal volumes.
- Friction
-
The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage.
- Functional health
-
The patient’s physical and mental capacity to participate in activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
- Functional Health Patterns
-
An evidence-based assessment framework for identifying patient problems and risks during the assessment phase of the nursing process.
- Functional incontinence
-
Occurs in older adults who have normal bladder control but have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly.
- Functional mobility
-
The ability of a person to move around in their environment, including walking, standing up from a chair, sitting down from standing, and moving around in bed.
- Gait belts
-
A 2-inch-wide (5 mm) belt, with or without handles, that is fastened around a patient’s waist used to ensure stability when assisting patients to stand, ambulate, or to transfer from bed to chair.
- Gas exchange
-
Refers to the exchange of oxygen and carbon dioxide in the alveoli and the pulmonary capillaries; also called respiration.
- Gender expression
-
A person’s outward demonstration of gender in relation to societal norms, such as in style of dress, hairstyle, or other mannerisms.
- Gender identity
-
A person’s inner sensibility that they are a man, a woman, or perhaps neither.
- generalization
-
A judgment formed from a set of facts, cues, and observations.
- Gerontology
-
The study of the social, cultural, psychological, cognitive, and biological aspects of aging.
- Glaucoma
-
Gradual loss of peripheral vision caused by elevated intraocular pressure that leads to progressive damage to the optic nerve.
- Global aphasia
-
A type of aphasia that results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phrases over and over again. They may have trouble understanding even simple words and sentences.
- glycemic index
-
A measure of how quickly glucose levels increase in the bloodstream after carbohydrates are consumed.
- Goals
-
Broad statements of purpose that describe the aim of nursing care.
- goiter
-
An abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism.
- Gout
-
A type of arthritis that causes swollen, red, hot, and stiff joints due to the buildup of uric acid, commonly starting in the big toe.
- Granulation tissue
-
New connective tissue in a healing wound with new, fragile, thin-walled capillaries.
- Grief
-
The emotional response to a loss, defined as the individualized and personalized feelings and responses that an individual makes to real, perceived, or anticipated loss.
- Growth
-
Physical changes that occur during the development of an individual beginning at the time of conception.
- hand hygiene
-
A way of cleaning one’s hands to substantially reduce the number of pathogens and other contaminants (e.g., dirt, body fluids, chemicals, or other unwanted substances) to prevent disease transmission or integumentary harm, typically using soap, water, and friction.
- Handoff reports
-
A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.
- HCO3
-
Bicarbonate level of arterial blood indicated in an arterial blood gas (ABG) result. Normal range is 22-26.
- health care disparity
-
Differences in access to health care and insurance coverage.
- health care power of attorney
-
A legal document that identifies a trusted individual to serve as a decision maker for health issues when the patient is no longer able to speak for themselves.
- Health disparities
-
Differences in health outcomes resulting from entrenched economic, sociopolitical, or environmental disadvantages.
- Health Insurance Portability and Accountability Act (HIPAA)
-
Standards for ensuring privacy of patient information that are enforceable by law.
- health promotion-wellness nursing diagnosis
-
A clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.
- Health Teaching and Health Promotion
-
Employing strategies to teach and promote health and wellness.
- healthcare-associated infection (HAI)
-
Infection that is contracted in a healthcare facility or under medical care.
- healthy environment
-
A place of physical, mental, and social well-being supporting optimal health and safety.
- Hematuria
-
Blood in urine, either visualized or found during microscopic analysis.
- hemostasis phase
-
The first stage of wound healing when clotting factors are released to form clots to stop the bleeding.
- holism
-
Treatment of the whole person, including physical, mental, spiritual, and social needs.
- Hospice care
-
A type of care selected by clients who are terminally ill and whose health care provider has determined they are expected to live six months or less that focuses on providing comfort and dignity at the end of life. It involves care and support services that can be of great benefit to people in the final stages of dementia and to their families.
- huffing technique
-
A technique helpful for patients who have difficulty coughing. Teach the patient to inhale with a medium-sized breath, and then make a sound like “ha” to push the air out quickly with the mouth slightly open.
- Human factors
-
A science that focuses on the interrelationships between humans, the tools and equipment they use in the workplace, and the environment in which they work.
- Hydrostatic pressure
-
The pressure that a contained fluid exerts on what is confining it.
- Hypercapnia
-
Elevated level of carbon dioxide in the blood.
- Hypertonic solutions
-
Intravenous fluids with a higher concentration of dissolved particles than blood plasma.
- hypervolemia
-
Excessive fluid volume
- hypodermis
-
The bottom layer of skin, also referred to as the subcutaneous layer, consisting mainly of adipose tissue or fat, along with some blood vessels and nerve endings. Beneath this layer lies muscle, tendons, ligaments, and bones.
- hypothesis
-
A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring.
- Hypotonic solutions
-
Intravenous fluids with a lower concentration of dissolved particles than blood plasma.
- hypovolemia
-
Intravascular fluid loss. Used interchangeably with “deficient fluid volume” and “dehydration.”
- Impaired skin integrity
-
Altered epidermis and/or dermis.
- impaired tissue integrity
-
Damage to deeper layers of the skin or other integumentary structures. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
- incentive spiromete
-
A medical device commonly prescribed after surgery to reduce the build up of fluid in the lungs and to prevent pneumonia. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for 5 seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient 10 times every hour while awake.
- incentive spirometer
-
A medical device commonly prescribed after surgery to reduce the build up of fluid in the lungs and to prevent pneumonia.
- Incident reports
-
A specific type of documentation that is completed when there is an unexpected occurrence, such as a medication error, client injury, client fall, or a near miss, where an error did not actually occur, but was prevented from occurring.
- Incomplete proteins
-
Proteins that do not contain enough amino acids to sustain life.
- incubation period
-
The period of a disease after the initial entry of the pathogen into the host but before symptoms develop.
- independent nursing intervention
-
Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else.
- Indirect care
-
Interventions performed by the nurse in a setting other than directly with the patient. An example of indirect care is creating a nursing care plan.
- Inductive reasoning
-
A type of reasoning that involves forming generalizations based on specific incidents.
- infection
-
The invasion and growth of a microorganism within the body.
- Infectious Agent
-
Microorganisms, such as bacteria, viruses, fungi, or parasites, that can cause infectious disease.
- inferences
-
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
- Inflammation
-
A response triggered by a cascade of chemical mediators that occur when pathogens successfully breach the nonspecific physical defenses of the immune system or when an injury occurs.
- inflammatory phase
-
The second stage of healing when vasodilation occurs to move white blood cells into the wound to start cleaning the wound bed.
- Insomnia
-
A common sleep disorder that causes trouble falling asleep, staying asleep, or getting good quality sleep.
- Inspection
- Intellectual disability
-
A diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period prior to the age 18.
- intersectionality
-
The many ways in which a person expresses their cultural identity are closely intertwined and not separated.
- interstitial fluid
-
Fluids found between the cells and outside of the vascular system.
- Intestinal obstruction
-
A partial or complete blockage of the intestines so that contents of the intestine cannot pass through it.
- Intimate partner violence (IPV)
-
Physical or sexual violence, stalking, and psychological or coercive aggression by current or former intimate partners.
- Intracellular fluids (ICF)
-
Fluids found inside cells consisting of protein, water, and electrolytes.
- Intravascular fluid
-
Fluids found in the vascular system consisting of the body’s arteries, veins, and capillary networks.
- Invasion
-
Means the spread of a pathogen throughout local tissues or the body.
- Involuntary guarding
-
The reflexive contraction of overlying abdominal muscules as the result of peritoneal inflammation.
- ISBARR
-
A mnemonic for the format of professional communication among health care team members that includes Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
- Isotonic solutions
-
Intravenous fluids with a similar concentration of dissolved particles as blood plasma.
- Joints
-
The location where bones come together.
- Just Culture
-
A quality of an institutional culture of safety where people are encouraged, even rewarded, for providing essential safety-related information, but clear lines are drawn between human error and at-risk or reckless behaviors.
- Justice
-
A principle and moral obligation to act on the basis of equality and equity, is a standard linked to fairness for all in society.
- key part
-
A key part is any sterile part of equipment used during an aseptic procedure, such as needle hubs, syringe tips, dressings, etc.
- key site
-
A key site is the site contacted during an aseptic procedure, such as non-intact skin, a potential insertion site, or an access site used for medical devices connected to the patients.
- kinesthetic impairment
-
An altered sense of touch that can cause difficulty in performing fine motor tasks.
- lactation
-
Breast milk production.
- lateral positioning
-
A position where the client lies on one side of the body with the top leg over the bottom leg.
- Learning culture
-
A quality of an institutional culture of safety that demonstrates the willingness and the competence to draw the right conclusions from safety information systems, and the will to implement major reforms when their need is indicated.
- lesion
-
An area of abnormal tissue.
- LGBTQ
-
Lesbian, gay, bisexual, transgender, queer, or questioning in reference to sexual orientation.
- licenced practical nurse
-
“An individual who has completed a state-approved practical or vocational nursing program, passed the NCLEX-PN examination, and is licensed by a state board of nursing to provide patient care.”
- Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs)
-
Nurses that have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of a LPN/LVN is determined by the facility and the state’s Nurse Practice Act.
- Ligaments
-
Strong bands of fibrous connective tissue that connect bones and strengthen and support joints by anchoring bones together and preventing their separation.
- living will
-
A legal document that describes the patient’s wishes if they are no longer able to speak for themselves due to injury, illness, or a persistent vegetative state.
- local infection
-
Infection confined to a small area of the body, typically near the portal of entry, and usually presents with signs of redness, warmth, swelling, prulent drainage, and pain.
- Lordosis
-
An inward curve of the lumbar spine just above the buttocks. A small degree of lordosis is normal, but too much curving is called swayback.
- Loss
-
The absence of a possession or future possession with the response of grief and the expression of mourning.
- Lymphadenopathy
-
Enlarged lymph nodes.
- maceration
-
A condition that occurs when skin has been exposed to moisture for too long causing it to appear soggy, wrinkled, or whiter than usual.
- Macrodrip tubing
-
Gravity IV tubing with drop factors of 10, 15, or 20 drops per minute that are typically used to deliver general IV solutions for adults.
- Macrominerals
-
Minerals needed in larger amounts and measured in milligrams, grams, and milliequivalents.
- Macronutrients
-
Nutrients needed in larger amounts due to energy needs. Macronutrients include carbohydrates, proteins, and fats.
- Macular degeneration
-
Loss of central vision with symptoms such as blurred central vision, distorted vision that causes difficulty driving and reading, and the requirement for brighter lights and magnification for close-up visual activities.
- malaise
-
Not feeling well.
- Malpractice
-
A specific term that looks at a standard of care, as well as the professional status of the caregiver.
- Maslow’s Hierarchy of Needs
-
A theory used to prioritize the most urgent client needs to address first. The bottom levels of the pyramid represent the most important physiological needs intertwined with safety.
- Mastication
-
The chewing of food in the mouth.
- maturation phase
-
The final stage of wound healing when collagen continues to be created to strengthen the wound and prevent it from reopening.
- mechanical digestion
-
Breaking food down into small chunks through chewing prior to swallowing.
- mechanical lift
-
A hydraulic lift with a sling used to move patients who cannot bear weight or have a medical condition that does not allow them to stand or assist with moving.
- Meconium
-
The black to dark green, sticky first bowel movement of a newborn.
- medical diagnoses
-
A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual.
- medical restraints
-
Restraints used to manage nonviolent, non-self-destructive behaviors such as the client attempting to remove life-sustaining tubes, drains, IV catheters, urinary catheters, or endotracheal tubes.
- medication cup
-
A small plastic or paper cup used to dispense oral medications.
- microbiome
-
Individual suite of microorganisms in and on the body.
- Microdrip tubing
-
Gravity IV tubing with a drop factor of 60 drops per minute.
- Microsleep
-
Brief moments of sleep that occur when a person is awake.
- Military time
-
A method of measuring the time based on the full twenty-four hours of the day rather than two groups of twelve hours indicated by AM and PM.
- Minimum Data Set (MDS)
-
A federally mandated assessment tool used in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life.
- Misuse
-
Taking prescription pain medications in a manner or dose other than prescribed; taking someone else’s prescription, even if for a medical complaint such as pain; or taking a medication to feel euphoria (i.e., to get high).
- Mixed urinary incontinence
-
Urinary frequency, urgency, and stress incontinence.
- Mobility
-
The ability of a patient to change and control body position.
- Moments for Hand Hygiene
-
Hand hygiene should be performed during select moments of patient care: immediately before touching a patient; before performing an aseptic task or handling invasive devices; before moving from a soiled body site to a clean body site on a patient; after touching a patient or their immediate environment; after contact with blood, body fluids, or contaminated surfaces (with or without glove use); and immediately after glove removal.
- Morality
-
Personal values, character, or conduct of individuals within communities and societies.
- Mourning
-
The outward, social expression of loss. Individuals outwardly express loss based on their cultural norms, customs, and practices, including rituals and traditions.
- Muscle atrophy
-
The thinning or loss of muscle tissue that can be caused by disuse, aging, or neurological damage.
- Narcolepsy
-
An uncommon sleep disorder that causes periods of extreme daytime sleepiness and sudden, brief episodes of deep sleep during the day.
- Narrative notes
-
A type of documentation that chronicles all of the patient’s assessment findings and nursing activities that occurred throughout the shift.
- National Patient Safety Goals
-
Annual patient safety goals and recommendations tailored for seven different types of health care agencies based on patient safety data from experts and stakeholders.
- Near misses
-
An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.
- necrosis
-
Tissue death.
- necrotic
-
Dead tissue that is black.
- Negligence
-
A general term that denotes conduct lacking in due care, carelessness; and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances.
- Never events
-
Adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable.
- nitrogen balance
-
The net loss or gain of nitrogen excreted compared to nitrogen taken into the body in the form of protein consumption; an indicator of protein status where a negative nitrogen balance equates to a protein deficit in the diet and a positive nitrogen balance equates to a protein excess in the diet.
- nociceptor
-
A sensory receptor for painful stimuli.
- Nocturia
-
The need for a patient to get up at night on a regular basis to urinate.
- non-REM
-
Slow-wave sleep when restoration takes place and the body’s temperature, heart rate, and oxygen consumption decrease.
- nonblanchable erythema
-
Skin redness that does not turn white when pressed.
- Nonspecific innate immunity
-
A system of defenses in the body that targets invading pathogens in a nonspecific manner that is present from the moment we are born.
- nontherapeutic responses
-
Responses to patients that block communication, expression of emotion, or problem solving.
- nonverbal communication
-
Facial expressions, tone of voice, pace of the conversation, and body language.
- normal flora
-
Microorganisms that live on our skin and in the nasopharynx and gastrointestinal tracts and don’t cause an infection unless the host becomes susceptible.
- Normal grief
-
The common feelings, behaviors, and reactions to loss.
- Nurse Licensure Compact
-
Allows a nurse to have one multistate license with the ability to practice in the home state and other compact states.
- Nurse Practice Act (NPA)
- nursing
-
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.
- nursing care plan
-
Specific documentation of the planning and delivery of nursing care that is required by the Joint Commission.
- nursing diagnosis
-
Defined as a “clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community.
- Nursing interventions
-
Evidence-based actions that the nurse performs to achieve patient outcomes.
- Nursing Practice Act
-
Legislation enacted by each state that establishes regulations for nursing practice within that state by defining the requirements for licensure as well as the scope of nursing practice.
- nursing process
-
A systematic approach to patient-centered care with five steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation, otherwise known by the mnemonic “ADOPIE.”
- Nutrient dense
-
Foods with a high proportion of nutritional value relative to calories contained in the food.
- Obstructive sleep apnea (OSA)
-
A common sleep condition that occurs when the upper airway becomes repeatedly blocked during sleep, reducing or completely stopping airflow.
- occult blood
-
Hidden blood in the stool not visible to the naked eye.
- Oliguria
-
Decreased urine output, defined as less than 500 mL urine in adults in a 24-hour period.
- oncotic pressure
-
Pressure inside the vascular compartment created by protein content of the blood (in the form of albumin) that holds water inside the blood vessels.
- open fracture
-
A type of fracture when the broken bone punctures the skin.
- Opioid intoxication
-
refers to significant behavioral or psychological changes (e.g., apathy, dysphoria, psychomotor agitation or retardation, or impaired judgment) that occur during or shortly after opioid use
- opportunistic pathogen
-
A pathogen that only causes disease in situations that compromise the host’s defenses, such as the body’s protective barriers, immune system, or normal microbiota.
- Oppression
-
The disadvantages (i.e., exclusion, marginalization, and inequality) experienced by people because of their membership in a cultural group.
- Oral syringes
-
A specific type of syringe used to measure and/or administer medications via the oral route.
- order
-
An intervention, remedy, or treatment as directed by an authorized primary health care provider
- Orthopnea
-
Difficulty in breathing that occurs when lying down and is relieved upon changing to an upright position.
- Orthostatic hypotension
-
Low blood pressure that occurs when a patient changes position from lying to sitting or sitting to standing that causes symptoms of dizziness or light-headedness.
- osmolality
-
Proportion of dissolved particles in a specific weight of fluid.
- Osmolarity
-
Proportion of dissolved particles or solutes in a specific volume of fluid.
- Osmosis
-
Movement of fluid through a semipermeable membrane from an area of lesser solute concentration to an area of greater solute concentration.
- Osteoarthritis
-
A most common type of arthritis associated with aging and wear and tear of the articular cartilage that covers the surfaces of bones at the synovial joint.
- outcome
-
A measurable behavior demonstrated by the client's response to nursing interventions
- Overdose
-
The biological response of the human body when too much of a substance is ingested.
- Overflow incontinence
-
Occurs when small amounts of urine leak from a bladder that is always full.
- PaCO2
-
Partial pressure of carbon dioxide level in arterial blood indicated in an ABG result. Normal range is 35-45 mmHg.
- Pain
-
An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.
- Palliative care
-
A broad philosophy of care defined by the World Health Organization as improving the quality of life of clients, as well as their family members, who are facing problems associated with life-threatening illness
- Palpation
- paralytic ileus
-
A condition where peristalsis is not propelling the contents through the intestines.
- Parenteral nutrition
-
An intravenous solution containing glucose, amino acids, minerals, electrolytes, and vitamins, along with supplemental lipids.
- Partially complete proteins
-
Proteins that have enough amino acids to sustain life, but not enough for tissue growth and maintenance.
- PASS
-
A mnemonic for actions to take when using a fire extinguisher, including Pull, Aim, Squeeze, and Sweep.
- Passive range of motion
-
Movement applied to a joint solely by another person or a passive motion machine.
- passive transport
-
Movement of fluids or solutes down a concentration gradient where no energy is used during the process.
- pathogenicity
-
The ability of a microorganism to cause disease.
- pathogens
-
Microorganisms that cause disease.
- Patient confidentiality
-
Keeping your patient’s Protected Health Information (PHI) protected and known only by those health care team members directly providing care for the patient.
- Patient-controlled analgesia (PCA)
-
A method of pain management that allows hospitalized patients with severe pain to safely self-administer opioid medications using a programmed pump according to their level of discomfort.
- Perception
-
The interpretation of sensation during the sensory process.
- Percussion
- peristalsis
-
Involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.
- Personal Protective Equipment (PPE)
-
Gloves, gowns, face shields, goggles, and masks used to prevent the spread of infection to and from patients and health care providers.
- PES
-
The format of a nursing diagnosis statement that includes:
Problem (P) - statement of the patient problem (i.e., the nursing diagnosis)
Etiology (E) - related factors (etiology) contributing to the cause of the nursing diagnosis
Signs and Symptoms (S) - defining characteristics (signs and symptoms) manifested by the patient of that nursing diagnosis. - PES format
-
Creating nursing diagnosis statements utilizing a problem, etiology, and sign and symptoms format.
- Ph level
-
A measurement of acidity or alkalinity of the blood
- Pharyngitis
-
Infection and/or inflammation in the back of the throat (pharynx).
- Physical dependence
-
Withdrawal symptoms that occur when chronic pain medication is suddenly reduced or stopped because of physiological adaptations that occur from chronic exposure to the medication.
- Physical examination
-
A systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion.
- Pleural rub
-
Sounds like the rubbing together of leather and can be heard on inspiration and expiration. It is caused by inflammation of the pleura membranes that results in friction as the surfaces rub against each other.
- Polyuria
-
Greater than 2.5 liters of urine output over 24 hours; also referred to as diuresis. Urine is typically clear with no color.
- portal of entry
-
An anatomic site through which pathogens can pass into a host, such as mucous membranes, skin, respiratory, or digestive systems.
- Postvoid residual
-
A measurement of urine left in the bladder after a patient has voided by using a bladder scanner or straight catheterization.
- Prejudice
-
To “pre-judge;” a preconceived idea, often unfavorable, about a person or group of people.
- presbycusis
-
Age-related hearing loss.
- Prescriptions
-
Interventions specifically related to medication as directed by an authorized primary health care provider
- Pressure injuries
-
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
- Primary care
-
Care that is provided to patients to promote wellness and prevent disease from occurring. This includes health promotion, education, protection (such as immunizations), early disease screening, and environmental considerations.
- Primary data
-
Information collected from the patient.
- primary health care provider
-
Member of the healthcare team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client.
- primary intention
-
A type of wound that is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure.
- primary pathogen
-
A pathogen that can cause disease in a host regardless of the host’s resident microbiota or immune system.
- Prioritization
-
The skillful process of deciding which actions to complete first for client safety and optimal client outcomes
- problem-focused nursing diagnosis
-
A “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.
- prodromal period
-
The disease stage after the incubation period when the pathogen continues to multiply and the host begins to experience general signs and symptoms of illness that result from activation of the immune system, such as fever, pain, soreness, swelling, or inflammation.
- progressive relaxation
-
Types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness.
- proliferative phase
-
The third stage of wound healing that begins a few days after injury and includes four processes: epithelialization, angiogenesis, collagen formation, and contraction.
- prone positioning
-
A position where the patient lies on their stomach with their head turned to the side.
- proprioception
-
The sense of the position of our bones, joints, and muscles.
- Proteins
-
Peptides and amino acids that provide 4 kcal/g of energy
- protocol
-
A precise and detailed written plan for a regimen of therapy.
- provider
-
A physician, podiatrist, dentist, optometrist, or advanced practice nurse provider.
- Pursed-lip breathing
-
A breathing technique that encourages a person to inhale through the nose and exhale through the mouth at a slow, controlled flow.
- Purulent
-
Drainage that is thick; opaque; tan, yellow, green, or brown in color. New purulent drainage should always be reported to the health care provider.
- purulent sputum
-
Yellow, green, or brown sputum that often indicates a respiratory infection.
- Pyuria
-
At least 10 white blood cells in each cubic millimeter of urine in a urine sample that typically indicates infection. In some cases, pus may be visible in the urine.
- Quality
-
The degree to which health services for patients, families, groups, communities, or populations increase the likelihood of desired outcomes and are consistent with current professional knowledge.
- Quality improvement
-
Combined and unceasing efforts of everyone–healthcare professionals, patients and their families, researchers, payers, planners and educators–to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development (learning).
- R.A.C.E.
-
A mnemonic for actions to immediately take during a fire, standing for Rescue, Activate, Confine, and Extinguish.
- Race
-
A socially constructed idea; there are no truly genetically or biologically distinct races. Humans are biologically similar to each other, not different.
- Racism
-
The presumption that races are distinct from one another and there is a hierarchy to race, implying that races are unequal. In racism, expression of one’s cultural beliefs are viewed as a heritable trait.
- Rales
-
Also called fine crackles, are popping or crackling sounds heard on inspiration. They are associated with medical conditions that cause fluid accumulation within the alveolar and interstitial spaces, such as heart failure or pneumonia. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- range of motion (ROM) exercises
-
Activities aimed to facilitate movement of specific joints and promote mobility of extremities.
- rapport
-
Developing a relationship of mutual trust and understanding.
- Reaction
-
The response that individuals have to a perception of a received stimulus.
- Reception
-
The initial part of the sensory process when a nerve cell or sensory receptor is stimulated by a sensation.
- Receptive aphasia
-
Difficulty in understanding what is being communicated
- Reckless behavior
-
According to the Just Culture model, an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.
- Rectal bleeding
-
Bright red blood in the stools; also referred to as hematochezia.
- Referred pain
-
Pain perceived at a location other than the site of the painful stimulus. For example, pain from retained gas in the colon can cause pain to be perceived in the shoulder.
- Refined grains
-
Grains that have been processed to remove parts of the grain kernel and supply little fiber.
- Registered Nurse
-
An individual who has graduated from a state-approved school of nursing, passed the NCLEX-RN examination, and is licensed by a state board of nursing to provide patient care.
- Registered Nurses (RNs)
-
A nurse who has had a designated amount of education and training in nursing and is licensed by the State Board of Nursing.
- Related factors
-
The underlying cause (etiology) of a nursing diagnosis
- relaxation breathing
-
A breathing technique used to reduce anxiety and control the stress response.
- Religion
-
A unified system of beliefs, values, and practices that a person holds sacred or considers to be spiritually significant.
- REM
-
Rapid eye movement (REM) sleep when heart rate and respiratory rate increase, eyes twitch, and brain activity increases.
- Renin-Angiotensin-Aldosterone System (RAAS)
-
A body system that regulates extracellular fluids and blood pressure by regulating fluid output and electrolyte excretion.
- Reporting culture
-
A quality of an institutional culture of safety where people report errors and near misses.
- respiration
-
Gas exchange occurs at the alveolar level where blood is oxygenated and carbon dioxide is removed.
- Respite care
-
Care provided at home (by a volunteer or paid service) or in a care setting, such as adult day care or residential facility, that allows the caregiver to take a much-needed break.
- Restraints
-
A device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement without the permission of the person.
- Rheumatoid Arthritis
-
A type of arthritis that causes pain, swelling, stiffness, and loss of function in joints due to inflammation caused by an autoimmune disease.
- Rhonchi
-
Also referred to as coarse crackles, are low-pitched, continuous sounds heard on expiration that are a sign of turbulent airflow through mucus in the large airways
- right to self-determination
-
Patients have the right to determine what will be done with and to their own person.
- risk nursing diagnosis
-
A clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.
- root cause analysis
-
A structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals.
- Rotation
-
Circular movement of a joint around a fixed point.
- Rule of Double Effect.
-
If the intent is good (i.e., relief of pain and suffering), then the act is morally justifiable even if it causes an unintended result of hastening death.
- safety culture
-
A culture established within healthcare agencies that empowers nurses, nursing students and other staff members to speak up about risks to patients and to report errors and near misses, all of which drive improvement in patient care and reduce the incident of patient harm.
- Safety Data Sheets (SDS)
-
Are hazardous communication sheets that let workers know certain information about chemicals they encounter in the workplace.
- Sanguineous
-
Drainage from a wound that is fresh bleeding.
- Saturated fats
-
Fats derived from animal products, such as butter, tallow, and lard for cooking or meat products such as steak.
- Scheduled hourly rounds
-
Scheduled hourly visits to each patient’s room to integrate fall prevention activities with the rest of a patient's care.
- Scope of practice
-
Defined as “services that a qualified health professional is deemed competent to perform, and permitted to undertake – in keeping with the terms of their professional license.”
- Seclusion
-
The confinement of a client in a locked room from which they cannot exit on their own. It is generally used as a method of discipline for behavior that can cause harm to themselves or others, or as a way to decrease environmental stimulation.
- Secondary care
-
Care that occurs when a person has contracted an illness or injury and is in need of medical care.
- secondary data
-
Information collected from sources other than the patient.
- secondary infection,
-
A localized pathogen that spreads to a secondary location.
- Secondary intention
-
A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure injury.
- Self-determination
-
A person's right to determine what will be done with and to their own body.
- self-limiting infections
-
Infections that develop rapidly and generally last only 10-14 days.
- Semi-Fowler’s positioning
-
A position where the head of the bed is placed at a 30- to 45-degree angle.
- sensory deprivation
-
When there is a lack of sensations that can occur due to sensory impairments or when the environment has few quality stimuli.
- Sensory impairment
-
Any type of difficulty that an individual has with one of their five senses. When an individual experiences loss of a sensory function, such as vision, the way they interact with the environment is affected.
- sensory overload
-
A condition that occurs when an individual receives too many stimuli or cannot selectively filter meaningful stimuli.
- Sentinel events
-
A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life.
- Sepsis
-
An existing infection that triggers an exaggerated inflammatory reaction called SIRS throughout the body.
- septic shock
-
Severe sepsis that leads to a life-threatening decrease in blood pressure (systolic pressure <90 mm Hg), preventing cells and other organs from receiving enough oxygen and nutrients. It can cause multi organ failure and death.
- septicemia
-
Bacteria that are both present and multiplying in the blood.
- Serosanguinous
-
Serous drainage with small amounts of blood present.
- Serous
-
Drainage from a wound that is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage.
- Sexual orientation
-
A person’s physical and emotional interest or desire for others. Sexual orientation is on a continuum and is manifested in one’s self-identity and behaviors.
- Sexuality
-
Encompasses sex, sexual orientation, gender identity, gender roles, among other topics.
- Shear
-
Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
- Simple carbohydrates
-
Small molecules of monosaccharides or disaccharides and break down quickly and raise blood glucose levels quickly.
- Simple human error
-
According to the Just Culture model, an error that occurs when an individual inadvertently does something other than what should have been done.
- Sims positioning
-
A position where the patient is positioned halfway between the supine and prone positions with their legs flexed.
- Sit to Stand Lifts
-
Mobility devices that assist weight-bearing patients who are unable to transition from a sitting position to a standing position by using their own strength.
- Skeletal muscles
-
Voluntary muscle that produces movement, assists in maintaining posture, protects internal organs, and generates body heat.
- Sleep apnea
-
a common sleep condition that occurs when the upper airway becomes repeatedly blocked during sleep, reducing or completely stopping airflow.
- sleep diary
-
A record of the time a person goes to sleep, wakes up, and takes naps each day for 1-2 weeks.
- sleep study
-
A diagnostic test that monitors and records data during a patient’s full night of sleep.
- Sleep-wake homeostasis
-
The homeostatic sleep drive keeps track of the need for sleep, reminds the body to sleep after a certain time, and regulates sleep intensity.
- slider board
-
A board (also called a transfer board) used to transfer an immobile patient from one surface to another while the patient is lying supine (e.g., from a stretcher to hospital bed).
- Slough
-
Inflammatory exudate in wounds that is usually light yellow, soft, and moist.
- SOAPIE
-
A mnemonic for a type of documentation that is organized by six categories: Subjective, Objective, Assessment, Plan, Interventions, and Evaluation.
- Social determinants of health
-
Nonmedical factors that influence health outcomes, including conditions in which people are born, grow, work, live, and age, and the wider sets of forces and systems shaping the conditions of daily life.
- social justice
-
Equal rights, equal treatment, and equitable opportunities for all.
- Somatosensation
-
Sensory receptors that respond to specific stimuli such as pain, pressure, temperature, and vibration; includes vestibular sensation and proprioception.
- Specific adaptive immunity
-
The immune response that is activated when the nonspecific innate immune response is insufficient to control an infection.
- SPICES tool
-
A tool that focuses on areas of common problems for aging individuals and can lead to early intervention and treatment.
- Spiritual distress
-
A state of suffering related to the impaired ability to experience meaning in life through connections with self, others, the world, or a superior being.
- Spirituality
-
A dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence and experience relationships to self, family, others, community, society, nature, and the significant or sacred.
- Sputum
-
Mucus and other secretions that are coughed up and expelled from the mouth.
- Stage 1 pressure injuries
-
Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred.
- Stage 2 pressure injuries
-
Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister.
- Stage 3 pressure injuries
-
Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed.
- Stage 4 pressure injuries
-
Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone.
- standard precautions
-
The minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where healthcare is delivered.
- Stereotyping
-
Assuming that a person has the attributes, traits, beliefs, and values of a group because they are a member of that group.
- Sterile technique
-
A process, also called surgical asepsis, used to eliminate every potential microorganism in and around a sterile field while also maintaining objects as free from microorganisms as possible.
- sterilization
-
A process used to destroy all pathogens from inanimate objects, including spores and viruses.
- Stress urinary incontinence
-
The involuntary loss of urine on intra-abdominal pressure (e.g., laughing and coughing) or physical exertion (e.g., jumping).
- subculture
-
A smaller group of people within a larger culture, often based on a person’s occupation, hobbies, interests, or place of origin.
- Substance abuse
-
A maladaptive pattern of continued use of alcohol or a drug despite it causing persistent social, occupational, psychological, or physical problems that can be physically hazardous.
- Substance abuse disorder
-
An illness caused by repeated misuse of substances (including opioids). When taken in excess, these substances have a common effect of directly activating the brain reward system and producing such an intense activation of the reward system that normal life activities may be neglected.
- Sundowning
-
Increased confusion, anxiety, agitation, pacing, and disorientation in patients with dementia that typically begins at dusk and continues throughout the night.
- supine positioning
-
A position where the patient lies flat on their back.
- syndrome
-
A “clinical judgment concerning a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions.”
- synovial fluid
-
A thick fluid that provides lubrication in joints to reduce friction between the bones.
- Synovial joints
-
A fluid-filled joint cavity where the articulating surfaces of the bones contact and move smoothly against each other. The elbow and knee are examples of synovial joints.
- Syringes
-
A medical device used to administer parenteral medication into tissue or into the bloodstream.
- systemic infection
-
An infection that becomes disseminated throughout the body.
- Systemic infections
-
An infection that becomes disseminated throughout the body.
- Systemic inflammatory response syndrome (SIRS)
-
An exaggerated inflammatory response to a noxious stressor (including, but not limited to, infection and acute inflammation) that affects the entire body.
- Systemic racism
-
The purposeful abuse of power by the dominant cultural group to deny equal rights and opportunities on the basis of one’s race. Systemic racism prevents less powerful groups from participating as equals in social, political, legislative, and economic areas of society.
- T cells
-
Immune cells that mature in the thymus.
- Tachypnea
-
Elevated respiratory rate above normal range according to the patient’s age.
- Tarry stools
-
Stools that are black and sticky that appear like tar; also referred to as melena.
- tendons
-
Strong bands of dense, regular connective tissue that connect muscles to bones.
- Tertiary care
-
A type of care that deals with the long-term effects from chronic illness or condition, with the purpose to restore physical and mental function that may have been lost. The goal is to achieve the highest level of functioning possible with this chronic illness.
- Tertiary intention
-
The healing of a wound that has had to remain open or has been reopened, often due to severe infection.
- The Timed Get Up and Go Test
-
A mobility assessment by nurses that begins by having the patient stand up from an armchair, walk three yards, turn, walk back to the chair, and sit down.
- Therapeutic communication
-
The purposeful, interpersonal information transmitting process through words and behaviors based on both parties’ knowledge, attitudes, and skills, which leads to patient understanding and participation.
- Therapeutic communication techniques
-
Techniques that encourage patients to explore feelings, problem solve, and cope with responses to medical conditions and life events.
- Tolerance
-
A diminished effect with continued use of the same amount of an opioid, or a need for increased amounts of opioids to achieve the desired effect or intoxication.
- Trace minerals
-
Minerals needed in tiny amounts.
- Trans fats
-
Fats that have been altered through hydrogenation and as such are not in their natural state.
- transcellular fluid
-
Fluid in areas such as cerebrospinal, synovial, intrapleural, and gastrointestinal system.
- Transcendance
-
An understanding of being part of a greater picture or of something greater than oneself, such as the awe one can experience when walking in nature.
- transcultural nursing
-
Incorporating cultural beliefs and practices of people to help them maintain and regain health or to face death in a meaningful way.
- Transferring:
-
The action of a patient moving from one surface to another.
- transmission-based precautions
-
Used for clients with documented or suspected infection of highly transmissible pathogens, such as C. difficile (C-diff), Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory Syncytial Virus (RSV), measles, and tuberculosis (TB).
- Trendelenburg positioning
-
A position where the head of the bed is placed lower than the patient’s feet.
- tripod position
-
A position that enhances air exchange when a patient sits up and leans over by resting their arms on their legs or on a bedside table, also referred to as a three-point position.
- Trousseau’s sign
-
A sign associated with hypocalcemia that causes a spasm of the hand when a blood pressure cuff is inflated.
- Tunneling
-
Passageways underneath the surface of the skin that extend from a wound and can take twists and turns.
- Undermining
-
A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge.
- Universal fall precautions
-
A set of interventions to reduce the risk of falls for all patients and focus on keeping the environment safe and comfortable.
- Unlicensed Assistive Personnel
-
Any unlicensed person, regardless of title, who performs tasks delegated by a nurse. This includes certified nursing aides/assistants (CNAs), patient care assistants (PCAs), patient care technicians (PCTs), state tested nursing assistants (STNAs), nursing assistants-registered (NA/Rs) or certified medication aides/assistants (MA-Cs). Certification of UAPs varies between jurisdictions.
- Unlicensed Assistive Personnel (UAP)
-
Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated.
- Unsaturated fats
-
Fats derived from oils and plants, though chicken and fish contain some unsaturated fats as well.
- Unstageable pressure injuries
-
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
- Urge urinary incontinence
-
Also referred to as “overactive bladder”; urine leakage accompanied by a strong desire to void.
- Urgency
-
A sensation of an urgent need to void.
- Urinary retention
-
A condition when the patient cannot empty all of the urine from their bladder.
- Urine specific gravity
-
A measurement of hydration status that measures the concentration of particles in urine.
- Venous insufficiency
-
A condition that occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart.
- verbal communication
-
Exchange of information using words understood by the receiver.
- vertigo
-
A sensation of dizziness as if the room is spinning.
- vestibular sensation
-
A sense of spatial orientation and balance.
- Vibratory Positive Expiratory Pressure (PEP) Therapy
-
Handheld devices such as flutter valves or Acapella devices are used with patients who need assistance in clearing mucus from their airways.
- Virulence
-
The degree to which a microorganism is likely to become a disease.
- Water-soluble vitamins
-
Vitamins that are not stored in the body and include vitamin C and B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin), B6 (pyridoxine), B12 (cyanocobalamin), and B9 (folic acid, biotin, and pantothenic acid).
- Whole grains
-
Grains with the entire grain kernel that supply more fiber than refined grains.
- withdrawal
-
Symptoms that cause significant distress after stopping or reducing the use of substances (including opioids), with symptoms such as dysphoric mood, nausea, vomiting, muscle aches, rhinorrhea or lacrimation, pupillary dilation, piloerection, sweating, diarrhea, yawning, fever, or insomnia.
is an abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism. If you find a goiter when assessing a patient’s neck, notify the health care provider for additional testing and treatment. See Figure 7.24[33] for an image of a goiter.

Headache
A headache is a common type of pain that patients experience in everyday life and a major reason for missed time at work or school. Headaches range greatly in severity of pain and frequency of occurrence. For example, some patients experience mild headaches once or twice a year, whereas others experience disabling migraine headaches more than 15 days a month. Severe headaches such as migraines may be accompanied by symptoms of nausea or increased sensitivity to noise or light. Primary headaches occur independently and are not caused by another medical condition. Migraine, cluster, and tension-type headaches are types of primary headaches. Secondary headaches are symptoms of another health disorder that causes pain-sensitive nerve endings to be pressed on or pulled out of place. They may result from underlying conditions including fever, infection, medication overuse, stress or emotional conflict, high blood pressure, psychiatric disorders, head injury or trauma, stroke, tumors, and nerve disorders such as trigeminal neuralgia, a chronic pain condition that typically affects the trigeminal nerve on one side of the cheek.[34]
Not all headaches require medical attention, but some types of headaches can signify a serious disorder and require prompt medical care. Symptoms of headaches that require immediate medical attention include a sudden, severe headache unlike any the patient has ever had; a sudden headache associated with a stiff neck; a headache associated with convulsions, confusion, or loss of consciousness; a headache following a blow to the head; or a persistent headache in a person who was previously headache free.[35]
Concussion
A concussion is a type of traumatic brain injury caused by a blow to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement causes the brain to bounce around in the skull, creating chemical changes in the brain and sometimes damaging brain cells.[36] See Figure 7.14[37] for an illustration of a concussion.
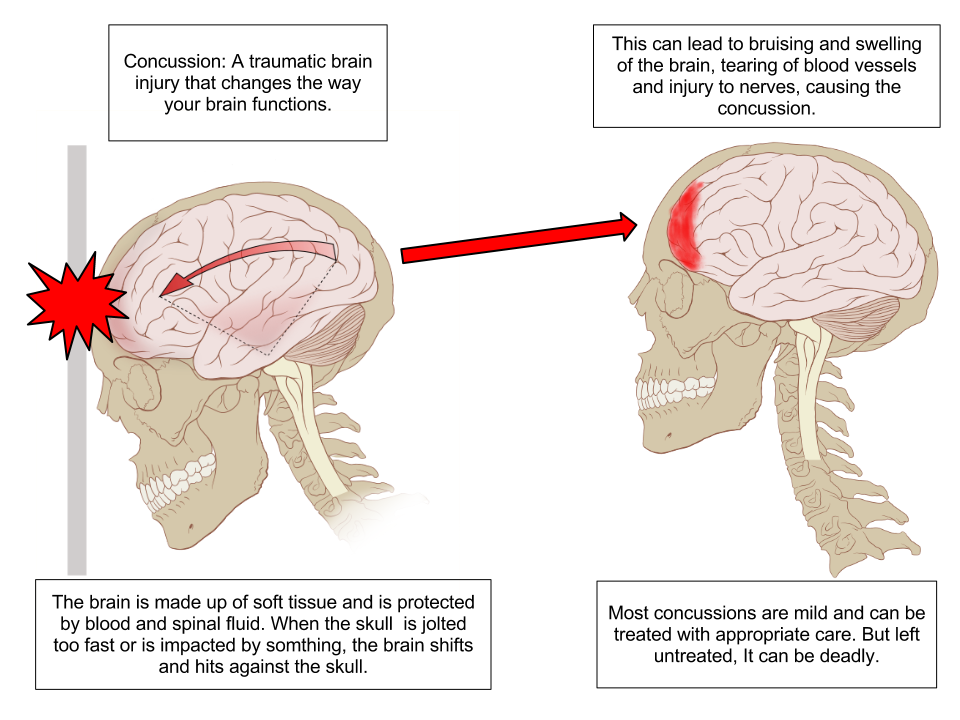
Review of Concussions on YouTube[38]
A person who has experienced a concussion may report the following symptoms:
- Headache or “pressure” in head
- Nausea or vomiting
- Balance problems or dizziness or double or blurry vision
- Light or noise sensitivity
- Feeling sluggish, hazy, foggy, or groggy
- Confusion, concentration, or memory problems
- Just not “feeling right” or “feeling down”[39]
The following signs may be observed in someone who has experienced a concussion:
- Can’t recall events prior to or after a hit or fall
- Appears dazed or stunned
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent
- Moves clumsily
- Answers questions slowly
- Loses consciousness (even briefly)
- Shows mood, behavior, or personality changes[40]
Anyone suspected of experiencing a concussion should immediately be seen by a health care provider or go to the emergency department for further testing.
Read more information about concussion signs and symptoms on the CDC's Concussion Signs and Symptoms webpage.
Head Injury
Head and traumatic brain injuries are major causes of immediate death and disability. Falls are the most common cause of head injuries in young children (ages 0–4 years), adolescents (15–19 years), and the elderly (over 65 years). Strong blows to the brain case of the skull can produce fractures resulting in bleeding inside the skull. A blow to the lateral side of the head may fracture the bones of the pterion. If the underlying artery is damaged, bleeding can cause the formation of a hematoma (collection of blood) between the brain and interior of the skull. As blood accumulates, it will put pressure on the brain. Symptoms associated with a hematoma may not be apparent immediately following the injury, but if untreated, blood accumulation will continue to exert increasing pressure on the brain and can result in death within a few hours.[41]
See Figure 7.15[42] for an image of an epidural hematoma indicated by a red arrow associated with a skull fracture.

Sinusitis
Sinusitis is the medical diagnosis for inflamed sinuses that can be caused by a viral or bacterial infection. When the nasal membranes become swollen, the drainage of mucous is blocked and causes pain.
There are several types of sinusitis, including these types:
- Acute Sinusitis: Infection lasting up to 4 weeks
- Chronic Sinusitis: Infection lasting more than 12 weeks
- Recurrent Sinusitis: Several episodes of sinusitis within a year
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Health care providers diagnose sinusitis based on symptoms and an examination of the nose and face. Treatments include antibiotics, decongestants, and pain relievers.[43]
Pharyngitis
PharynPharyngitisgitis is the medical term used for infection and/or inflammation in the back of the throat (pharynx). Common causes of pharyngitis are the cold viruses, influenza, strep throat caused by group A streptococcus, and mononucleosis. Strep throat typically causes white patches on the tonsils with a fever and enlarged lymph nodes. It must be treated with antibiotics to prevent potential complications in the heart and kidneys. See Figure 7.16[44] for an image of strep throat in a child.
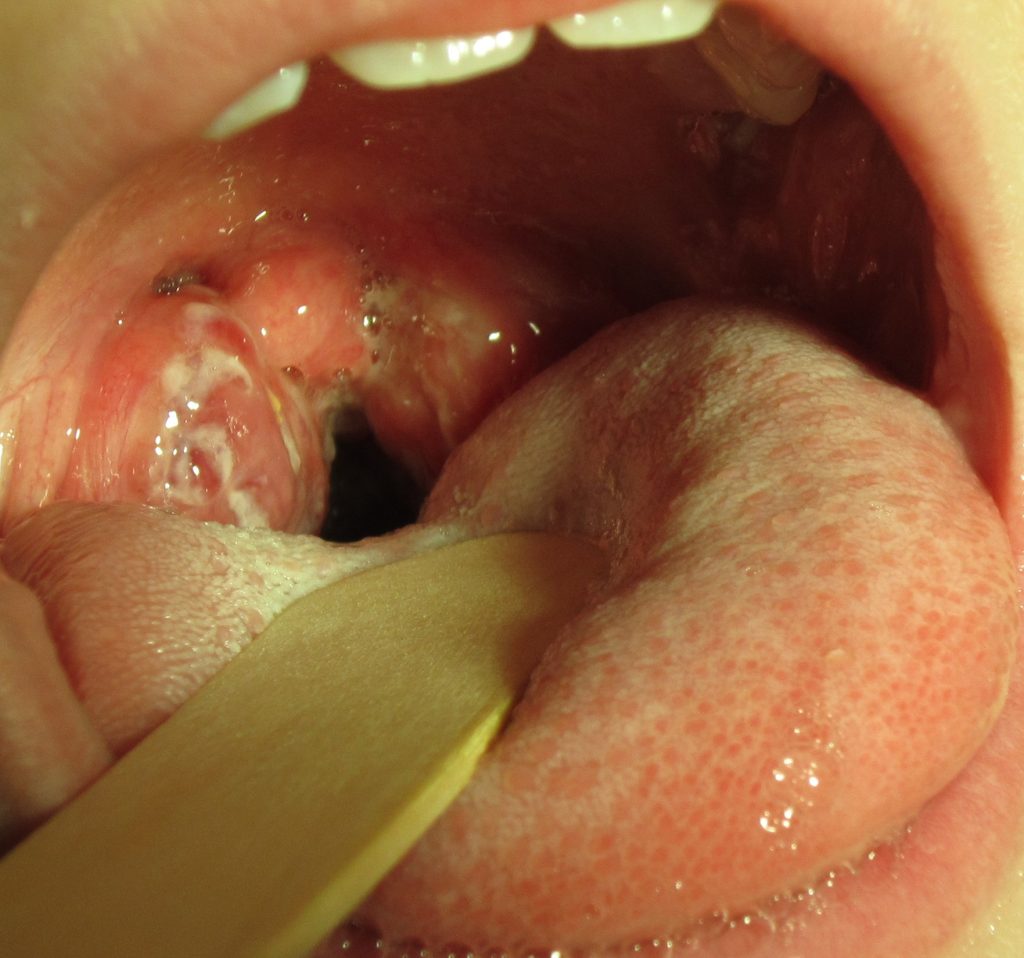
If not diagnosed as strep throat, most cases of pharyngitis are caused by viruses, and the treatment is aimed at managing the symptoms. Nurses can teach patients the following ways to decrease the discomfort of a sore throat:
- Drink soothing liquids such as lemon tea with honey or ice water.
- Gargle several times a day with warm salt water made of 1/2 tsp. of salt in 1 cup of water.
- Suck on hard candies or throat lozenges.
- Use a cool-mist vaporizer or humidifier to moisten the air.
- Try over-the-counter pain medicines, such as acetaminophen.[45]
Epistaxis
Epistaxis, the medical term for a nosebleed, is a common problem affecting up to 60 million Americans each year. Although most cases of epistaxis are minor and manageable with conservative measures, severe cases can become life-threatening if the bleeding cannot be stopped.[46] See Figure 7.17[47] for an image of a severe case of epistaxis.

The most common cause of epistaxis is dry nasal membranes in winter months due to low temperatures and low humidity. Other common causes are picking inside the nose with fingers, trauma, anatomical deformity, high blood pressure, and clotting disorders. Medications associated with epistaxis are aspirin, clopidogrel, nonsteroidal anti-inflammatory drugs, and anticoagulants.[48]
To treat a nosebleed, have the victim lean forward at the waist and pinch the lateral sides of the nose with the thumb and index finger for up to 15 minutes while breathing through the mouth.[49] Continued bleeding despite this intervention requires urgent medical intervention such as nasal packing.
Cleft Lip and Palate
During embryonic development, the right and left maxilla bones come together at the midline to form the upper jaw. At the same time, the muscle and skin overlying these bones join together to form the upper lip. Inside the mouth, the palatine processes of the maxilla bones, along with the horizontal plates of the right and left palatine bones, join together to form the hard palate. If an error occurs in these developmental processes, a birth defect of cleft lip or cleft palate may result.
Cleft lip is a common developmental defect that affects approximately 1:1,000 births, most of which are male. This defect involves a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a cleft (gap). See Figure 7.18[50] for an image of an infant with a cleft lip.

A more severe developmental defect is a cleft palate that affects the hard palate, the bony structure that separates the nasal cavity from the oral cavity. See Figure 7.19[51] for an illustration of a cleft palate. Cleft palate affects approximately 1:2,500 births and is more common in females. It results from a failure of the two halves of the hard palate to completely come together and fuse at the midline, thus leaving a gap between the nasal and oral cavities. In severe cases, the bony gap continues into the anterior upper jaw where the alveolar processes of the maxilla bones also do not properly join together above the front teeth. If this occurs, a cleft lip will also be seen. Because of the communication between the oral and nasal cavities, a cleft palate makes it very difficult for an infant to generate the suckling needed for nursing, thus creating risk for malnutrition. Surgical repair is required to correct a cleft palate.[52]
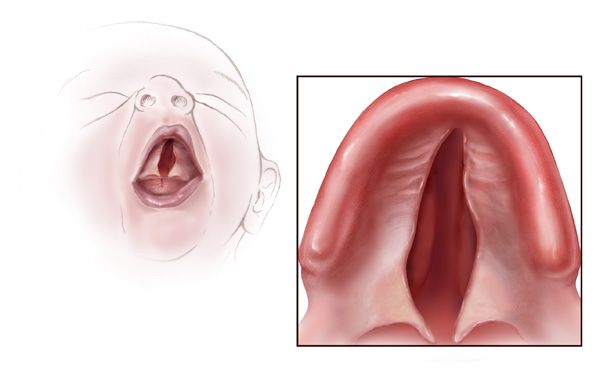
Poor Oral Health
Despite major improvements in oral health for the population as a whole, oral health disparities continue to exist for many racial, ethnic, and socioeconomic groups in the United States. Healthy People 2020, a nationwide initiative geared to improve the health of Americans, identified improved oral health as a health care goal. A growing body of evidence has also shown that periodontal disease is associated with negative systemic health consequences. Periodontal diseases are infections and inflammation of the gums and bone that surround and support the teeth. Red, swollen, and bleeding gums are signs of periodontal disease. Other symptoms of periodontal disease include bad breath, loose teeth, and painful chewing.[53] In 2020, the Centers for Disease Control and Prevention (CDC) reported that 42% of U.S. adults have some form of periodontitis, and almost 60% of adults aged 65 and older have periodontitis. See Figure 7.20[54] for an image of a patient with periodontal disease. Nurses may encounter patients who complain of bleeding gums, or they may discover other signs of periodontal disease during a physical assessment.

Because many Americans lack access to oral care, it is important for nurses to perform routine oral assessment and identify needs for follow-up. If signs and/or symptoms indicate potential periodontal disease, the patient should be referred to a dental health professional for a more thorough evaluation.[55]
Thrush/Candidiasis
Candidiasis is a fungal infection caused by Candida. Candida normally lives on the skin and inside the body without causing any problems, but it can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages fungal growth.[56] See Figure 7.21[57] for an image of candidiasis.

Candidiasis in the mouth and throat can have many symptoms, including the following:
- White patches on the inner cheeks, tongue, roof of the mouth, and throat
- Redness or soreness
- Cotton-like feeling in the mouth
- Loss of taste
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth[58]
Candidiasis in the mouth or throat is common in babies but is uncommon in healthy adults. Risk factors for getting candidiasis as an adult include the following:
- Wearing dentures
- Diabetes
- Cancer
- HIV/AIDS
- Taking antibiotics or corticosteroids including inhaled corticosteroids for conditions like asthma
- Taking medications that cause dry mouth or have medical conditions that cause dry mouth
- Smoking
The treatment for mild to moderate cases of candidiasis infections in the mouth or throat is typically an antifungal medicine applied to the inside of the mouth for 7 to 14 days, such as clotrimazole, miconazole, or nystatin.
"Meth Mouth"
The use of methamphetamine (i.e., meth), a strong stimulant drug, has become an alarming public health issue in the United States. A common sign of meth abuse is extreme tooth and gum decay often referred to as “Meth Mouth.” See Figure 7.22[59] for an image of Meth Mouth.

Signs of Meth Mouth include the following:
- Dry Mouth. Methamphetamines dry out the salivary glands, and the acid content in the mouth will start to destroy the enamel on the teeth. Eventually this will lead to cavities.
- Cracked Teeth. Methamphetamine can make the user feel anxious, hyper, or nervous, so they clench or grind their teeth. You may see severe wear patterns on their teeth.
- Tooth Decay. Methamphetamine users crave beverages high in sugar while they are “high.” The bacteria that feed on the sugars in the mouth will secrete acid, which can lead to more tooth destruction. With methamphetamine users, tooth decay will start at the gum line and eventually spread throughout the tooth. The front teeth are usually destroyed first.
- Gum Disease. Methamphetamine users do not seek out regular dental treatment. Lack of oral health care can contribute to periodontal disease. Methamphetamines also cause the blood vessels that supply the oral tissues to shrink in size, reducing blood flow, causing the tissues to break down.
- Lesions. Users who smoke methamphetamine may present with lesions and/or burns on their lips or gingival inside the cheeks or on the hard palate. Users who snort may present with burns in the back of their throats.[60]
Nurses who notice possible signs of "Meth Mouth" should report their concerns to the health care provider, not only for a referral for dental care, but also for treatment of suspected substance abuse.
Dysphagia
Dysphagia is the medical term for difficulty swallowing that can be caused by many medical conditions. Nurses are often the first health care professionals to notice a patient’s difficulty swallowing as they administer medications or monitor food intake. Early identification of dysphagia, especially after a patient has experienced a cerebrovascular accident (i.e., stroke) or other head injury, helps to prevent aspiration pneumonia.[61] Aspiration pneumonia is a type of lung infection caused by material from the stomach or mouth entering the lungs and can be life-threatening.
Signs of dysphagia include the following:
- Coughing during or right after eating or drinking
- Wet or gurgly sounding voice during or after eating or drinking
- Extra effort or time required to chew or swallow
- Food or liquid leaking from mouth
- Food getting stuck in the mouth
- Difficulty breathing after meals[62]
The Barnes-Jewish Hospital-Stroke Dysphagia Screen (BJH-SDS) is an example of a simple, evidence-based bedside screening tool that can be used by nursing staff to efficiently identify swallowing impairments in patients who have experienced a stroke. See internet resource below for an image of the dysphagia screening tool. The result of the screening test is recorded as a “fail” if any of the five items tested are abnormal (Glasgow Coma Scale < 13, facial/tongue/palatal asymmetry or weakness, or signs of aspiration on the 3-ounce water test) or “pass” if all five items tested were normal. Patients with a failed screening result are placed on nothing-by-mouth (NPO) status until further evaluation is completed by a speech therapist. For more information about using the Glasgow Coma Scale, see the "Assessing Mental Status" section in the “Neurological Assessment” chapter.
View a PDF sample of a Nursing Bedside Swallow Screen.
Enlarged Lymph Nodes
Lymphadenopathy is the medical term for swollen lymph nodes. In a child, a node is considered enlarged if it is more than 1 centimeter (0.4 inch) wide. See Figure 7.23[63] for an image of an enlarged cervical lymph node.

Common infections such as a cold, pharyngitis, sinusitis, mononucleosis, strep throat, ear infection, or infected tooth often cause swollen lymph nodes. However, swollen lymph nodes can also signify more serious conditions. Notify the health care provider if the patient’s lymph nodes have the following characteristics:
- Do not decrease in size after several weeks or continue to get larger
- Are red and tender
- Feel hard, irregular, or fixed in place
- Are associated with night sweats or unexplained weight loss
- Are larger than 1 centimeter in diameter
The health care provider may order blood tests, a chest X-ray, or a biopsy of the lymph node if these signs occur.[64]
Thyroid
The thyroid is a butterfly-shaped gland located at the front of the neck that controls many of the body’s important functions. The thyroid gland makes hormones that affect breathing, heart rate, digestion, and body temperature. If the thyroid makes too much or not enough thyroid hormone, many body systems are affected. In hypothyroidism, the thyroid gland doesn’t produce enough hormone and many body functions slow down. When the thyroid makes too much hormone, a condition called hyperthyroidism, many body systems speed up.[65]
A goiter is an abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism. If you find a goiter when assessing a patient’s neck, notify the health care provider for additional testing and treatment. See Figure 7.24[66] for an image of a goiter.

Swelling in tissues caused by fluid retention.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Mr. Jones is a 76-year-old patient admitted to the medical surgical floor with complications of a nonhealing foot ulcer. Mr. Jones has a history of diabetes, hypertension, and COPD. He has a BMI of 29. His daily medications include metformin, Lisinopril, and prednisone. His wife has recently passed away and he lives alone.
- Based upon what is known about Mr. Jones, what factors might be contributing to his nonhealing wound?
- What other factors that influence wound healing might be important to assess with Mr. Jones?
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 3.
A birth defect caused when two halves of the hard palate fail to completely come together and fuse at the midline, leaving a gap between them, and making it very difficult for an infant to generate the suckling needed for nursing.
Nosebleed.
A birth defect caused by a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a gap in the lip.
A fungal infection often referred to as “thrush” when it occurs in the oral cavity in children.
A type of lung infection caused by material from the stomach or mouth inadvertently entering the lungs that can be life-threatening.
Enlarged lymph nodes.
An abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism.
Subjective Assessment
Begin the head and neck assessment by asking focused interview questions to determine if the patient is currently experiencing any symptoms or has a previous medical history related to head and neck issues.
Table 7.4a Interview Questions for Subjective Assessment of the Head and Neck
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a medical condition related to your head such as headaches, a concussion, a stroke, or a head injury? | Please describe. |
| Have you ever been diagnosed with a medical condition related to your neck such as a thyroid or swallowing issue? | Please describe. |
| Are you currently taking any medications, herbs, or supplements for headaches or for your thyroid? | Please describe. |
| Have you had any symptoms such as headaches, nosebleeds, nasal drainage, sinus pressure, sore throat, or swollen lymph nodes? | If yes, use the PQRSTU method to gather additional information regarding each symptom. |
Specific oral assessment questions[67]:
|
Life Span Considerations
Infants and Children
For infants, observe head control and muscle strength. Palpate the skull and fontanelles for smoothness. Ask the parents or guardians if the child has had frequent throat infections or a history of cleft lip or cleft palate. Observe head shape, size, and symmetry.
Older Adults
Ask older adults if they have experienced any difficulties swallowing or chewing. Document if dentures are present. Muscle atrophy and loss of fat often cause neck shortening. Fat accumulation in the back of the neck causes a condition referred to as "Dowager's hump."
Objective Assessment
Use any information obtained during the subjective interview to guide your physical assessment.
Inspection
- Begin by inspecting the head for skin color and symmetry of facial movements, noting any drooping. If drooping is noted, ask the patient to smile, frown, and raise their eyebrows and observe for symmetrical movement. Note the presence of previous injuries or deformities.
- Inspect the nose for patency and note any nasal drainage.
- Inspect the oral cavity and ask the patient to open their mouth and say “Ah.” Inspect the patient's mouth using a good light and tongue blade.
- Note oral health of the teeth and gums.
- If the patient wears dentures, remove them so you can assess the underlying mucosa.
- Assess the oral mucosa for color and the presence of any abnormalities.
- Note the color of the gums, which are normally pink. Inspect the gum margins for swelling, bleeding, or ulceration.
- Inspect the teeth and note any missing, discolored, misshapen, or abnormally positioned teeth. Assess for loose teeth with a gloved thumb and index finger, and document halitosis (bad breath) if present.[68]
- Assess the tongue. It should be midline and with no sores or coatings present.
- Assess the uvula. It should be midline and should rise symmetrically when the patient says “Ah.”
- Is the patient able to swallow their own secretions? If the patient has had a recent stroke or you have any concerns about their ability to swallow, perform a brief bedside swallow study according to agency policy before administering any food, fluids, or medication by mouth.
- Note oral health of the teeth and gums.
- Inspect the neck. The trachea should be midline, and there should not be any noticeable enlargement of lymph nodes or the thyroid gland.
- Note the patient’s speech. They should be able to speak clearly with no slurring or garbled words.
If any neurological concerns are present, a cranial nerve assessment may be performed. Read more about a cranial nerve assessment in the “Neurological Assessment” chapter.
Auscultation
Auscultation is not typically performed by registered nurses during a routine neck assessment. However, advanced practice nurses and other health care providers may auscultate the carotid arteries for the presence of a swishing sound called a bruit.
Palpation
Palpate the neck for masses and tenderness. Lymph nodes, if palpable, should be round and movable and should not be enlarged or tender. See the figure illustrating the location of lymph nodes in the head and neck in the "Head and Neck Basic Concepts" section earlier in this chapter. Advanced practice nurses and other health care providers palpate the thyroid for enlargement, further evaluate lymph nodes, and assess the presence of any masses.
See Table 7.4b for a comparison of expected versus unexpected findings when assessing the head and neck.
Table 7.4b Expected Versus Unexpected Findings on Adult Assessment of the Head and Neck
| Assessment | Expected Findings | Unexpected Findings (to document and notify provider if new finding*) |
|---|---|---|
| Inspection | Skin tone is appropriate for ethnicity, and skin is dry.
Facial movements are symmetrical. Nares are patent and no drainage is present. Uvula and tongue are midline. Teeth and gums are in good condition. Patient is able to swallow their own secretions. Trachea is midline. If dentures are present, there is a good fit, and the patient is able to appropriately chew food. |
Skin is pale, cyanotic, or diaphoretic (inappropriately perspiring).
New asymmetrical facial expressions or drooping is present. Nares are occluded or nasal drainage is present. Uvula and/or tongue is deviated to one side. White coating or lesions on the tongue or buccal membranes (inner cheeks) are present. Teeth are missing or decay is present that impacts the patient’s ability to chew. After swallowing, the patient coughs, drools, chokes, or speaks in a gurgly/wet voice. Trachea is deviated to one side. Dentures have poor fit and/or the patient is unable to chew food contained in a routine diet. |
| Palpation | No unusual findings regarding lymph nodes are present. | Cervical lymph nodes are enlarged, tender, or nonmovable. Report any concerns about lymph nodes to the health care provider. |
| *CRITICAL CONDITIONS to report immediately | New asymmetry of facial expressions, tracheal deviation to one side, slurred or garbled speech, signs of impaired swallowing, coughing during or after swallowing, or a “wet” voice after swallowing. |
Anatomy of the Eye
Our sense of vision occurs due to transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. See Figure 8.1[69] for an illustration of the eye. The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye. The inner surface of each lid is a thin membrane known as the conjunctiva. The conjunctiva extends over the white areas of the eye called the sclera, connecting the eyelids to the eyeball. The iris is the colored part of the eye. The iris is a smooth muscle that opens and closes the pupil, the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light. The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. The cornea, with the anterior chamber and lens, refracts light and contributes to vision. The cornea can be reshaped by surgical procedures such as LASIK. The innermost layer of the eye is the retina that contains the nervous tissue and specialized cells called photoreceptors for the initial processing of visual stimuli. Two types of photoreceptors within the retina are the rods and the cones. The cones are sensitive to different wavelengths of light and provide color vision. These nerve cells of the retina leave the eye and enter the brain via the optic nerve (cranial nerve II).[70]
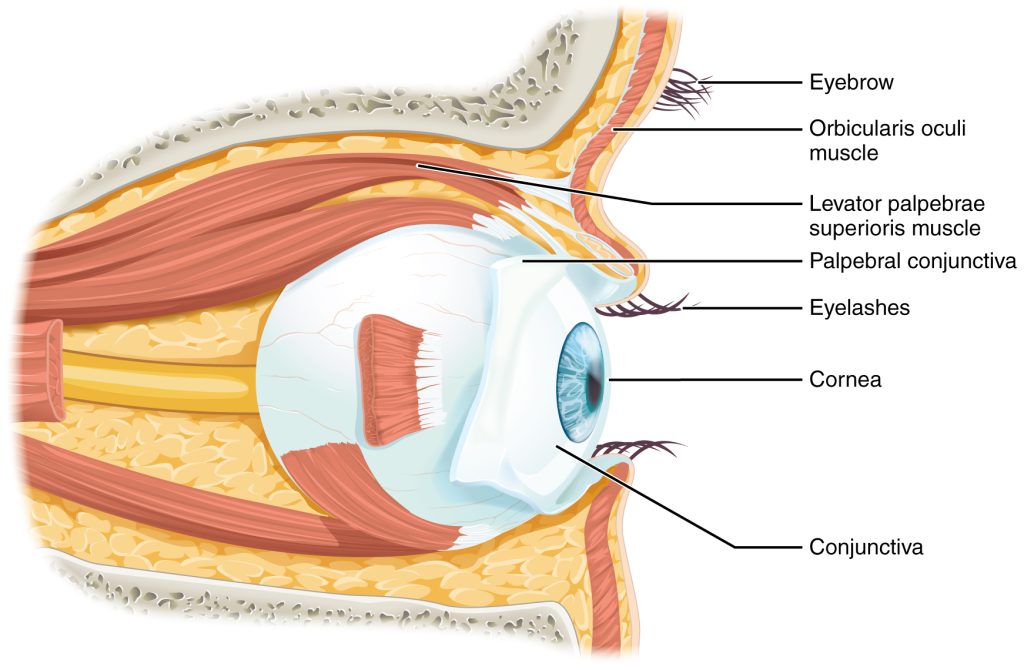
Tears are produced by the lacrimal gland that is located beneath the lateral edges of the nose. Tears flow through the lacrimal duct to the medial corner of the eye and flow over the conjunctiva to wash away foreign particles. Movement of the eye within the orbit occurs by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. The extraocular muscles are innervated by the abducens nerve, the trochlear nerve, and the oculomotor nerve (cranial nerves III, IV, and V).[71] See the illustration of the extraocular muscles in Figure 8.2.[72]
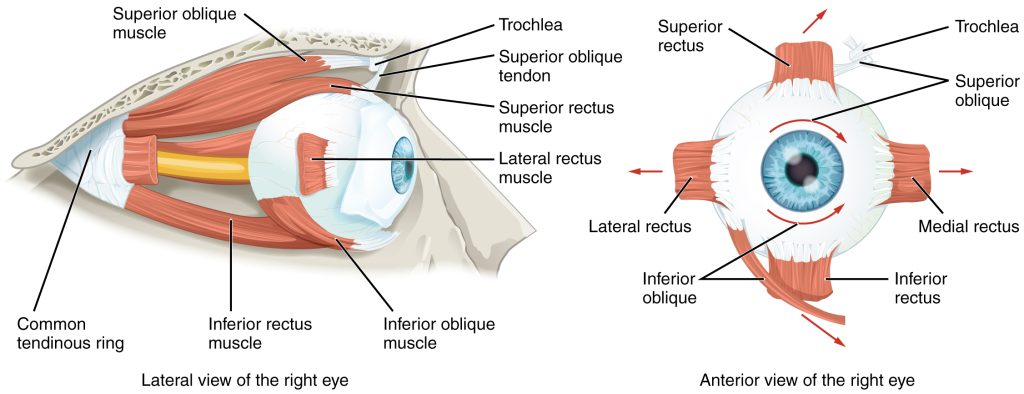
Review for Anatomy of the Eye on YouTube[73]
Common Disorders of the Eye
Eye disorders that nurses commonly see in practice include myopia, presbyopia, color blindness, dry eye, conjunctivitis, styes, cataracts, macular degeneration, and glaucoma.
Myopia
Myopia is impaired vision, also known as nearsightedness that makes far-away objects look blurry. It happens when the eyeball grows too long from front to back or when there are problems with the shape of the cornea or the lens. These problems make light focus in front of the retina, instead of on it, causing blurriness. See Figure 8.3[74] for a simulated image of a person’s vision with myopia. Nearsightedness usually becomes apparent between ages 6 and 14. It is corrected with glasses, contacts, or LASIK surgery.[75]

Presbyopia
Presbyopia is impaired near vision. It commonly occurs in middle-aged and older adults, making it difficult to clearly see objects up close. As people age, the lens in the eye gets harder and less flexible and stops focusing light correctly on the retina.[76] Presbyopia can be corrected with glasses and/or contacts. See Figure 8.4[77] for a simulated image of a person’s vision with presbyopia.
Color Blindness
Color blindness makes it difficult to differentiate between certain colors. Color blindness can occur due to damage to the eye or to the brain. There’s no cure for color blindness, but special glasses and contact lenses can help people differentiate between colors. Most people who have color blindness are able to use visual strategies related to color selection and don’t have problems participating in everyday activities.[78]
Dry Eye
Dry eye is a very common eye condition that occurs when the eyes don’t make enough tears to stay wet or the tears don’t work correctly. Symptoms of dry eye include a scratchy feeling, stinging, and burning. Treatment includes over-the-counter and prescription eye drops, as well as lifestyle changes to decrease the dryness of the eyes.[79]
Conjunctivitis
Conjunctivitis is a viral or bacterial infection that causes swelling and redness in the conjunctiva and sclera. See Figure 8.5[80] for an image of conjunctivitis. The eye may feel itchy and painful with crusty yellow drainage present. Conjunctivitis is very contagious, so the nurse should educate the patient and family caregivers to wash hands frequently. Additionally, the patient should not share items like pillowcases, towels, or makeup. Bacterial conjunctivitis is treated with antibiotic eye drops.[81]

Stye
A stye is a bacterial infection of an oil gland in the eyelid, causing a red, tender bump at the edge of the eyelid. See Figure 8.6[82] for an image of a stye. Treatment includes applying warm compresses to the eyelid and prescription eyedrops.[83]
Cataracts
A cataract is a cloudy area on the lens of the eye. Cataracts are very common in older adults. Over half of all Americans age 80 or older either have cataracts or have had surgery to remove cataracts. See Figure 8.7[84] for an image of a cataract. Cataracts develop slowly and symptoms include faded colors, blurred or double vision, halos around light, and trouble seeing at night. See Figure 8.8[85] for a simulated image of a person’s vision with cataracts. Decreased vision due to cataracts may result in trouble reading and driving and increases the risk of falling. Patients often undergo surgery for cataracts. During cataract surgery, the doctor removes the clouded lens and replaces it with a new, artificial lens.[86]
Macular Degeneration
Age-related macular degeneration is a common condition that causes blurred central vision. It is the leading cause of vision loss for people 50 and older. See Figure 8.9[87] for a simulated image of a person’s vision with macular degeneration. There are two types of macular degeneration: dry (nonexudative) and wet (exudative). During dry macular degeneration, cellular debris called drusen accumulates and scars the retina. In the wet (exudative) form, which is more severe, blood vessels grow behind the retina that leak exudate fluid, causing hemorrhaging and scarring. There is no treatment for dry macular degeneration, but laser therapy can be used to help treat wet (exudative) macular degeneration.[88]

Glaucoma
Glaucoma is a group of eye diseases that causes vision loss by damaging the optic nerve due to increased intraocular pressure. Treatment includes prescription eye drops to lower the pressure inside the eye and slow the progression of the disease. If not treated appropriately, glaucoma can cause blindness. Symptoms of glaucoma include gradual loss of peripheral vision. See Figure 8.10[89] for a simulated image of a person’s vision with glaucoma. Because the loss of vision occurs so slowly, many people don’t realize they have symptoms until the disease is well-progressed or it is discovered during an eye exam.[90]
Screening Tools for Eye Exams
Common screening tools used during an eye exam are the Snellen chart, a near vision chart, and Ishihara plates. Nurses working in outpatient settings or school settings use these tools when screening patients for vision problems. If a vision problem is identified, the patient is referred to an optometrist for further testing. When performing a vision assessment, be sure to provide adequate lighting.
Snellen Chart
Distant vision is tested by using the Snellen chart. See Figure 8.11[91] for an image of the Snellen chart. Place the patient 20 feet away from the Snellen chart. Ask them to cover one eye and read the letters from the lowest line they can see clearly. Record the corresponding fraction in the furthermost right-hand column. Repeat with the other eye. If the patient is wearing glasses or contact lens during this assessment, document the results as “corrected vision” when wearing these assistive devices.
A person with no visual impairment is documented as having 20/20 vision. A person with impaired vision has a different lower denominator of this fraction. For example, a vision measurement of 20/30 indicates the patient can see letters clearly at 20 feet that a person with normal vision can see clearly at 30 feet.[92] Alternative charts are also available for children or adults who can’t read letters in English. See Figure 8.12[93]for an alternative eye chart.

Near Vision
Near vision is assessed by having a patient read from a prepared card that is held 14 inches away from the eyes. If a card is not available, the patient can be asked to read from a newspaper as an alternative quick screening tool. See Figure 8.13[94] for an image of a prepared card used to assess near vision.
Ishihara Plates
Ishihara plates are commonly used to assess color vision. Each of the colored dotted plates shows either a number or a path. See Figure 8.14[95] for an example of Ishihara plates. A person with color blindness is not able to distinguish the numbers or paths from the other colored dots on the plate.
Anatomy of the Ear
Hearing is the transduction of sound waves into a neural signal by the structures of the ear. See Figure 8.15[96] for an image of the anatomy of the ear. The large, fleshy structure on the lateral aspect of the head is known as the auricle. The C-shaped curves of the auricle direct sound waves toward the ear canal. At the end of the ear canal is the tympanic membrane, commonly referred to as the eardrum, that vibrates after it is struck by sound waves. The auricle, ear canal, and tympanic membrane are referred to as the external ear. The middle ear consists of a space with three small bones called the malleus, incus, and stapes, the Latin names that roughly translate to “hammer,” “anvil,” and “stirrup.” The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is attached to the inner ear, where the sound waves are transduced into a neural signal. The middle ear is also connected to the pharynx through the Eustachian tube that helps equilibrate air pressure across the tympanic membrane. The Eustachian tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning. The inner ear is often described as a bony labyrinth because it is composed of a series of semicircular canals. The semicircular canals have two separate regions, the cochlea and the vestibule, that are responsible for hearing and balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, they travel together from the inner ear to the brain stem as the vestibulocochlear nerve (cranial nerve VIII).[97]
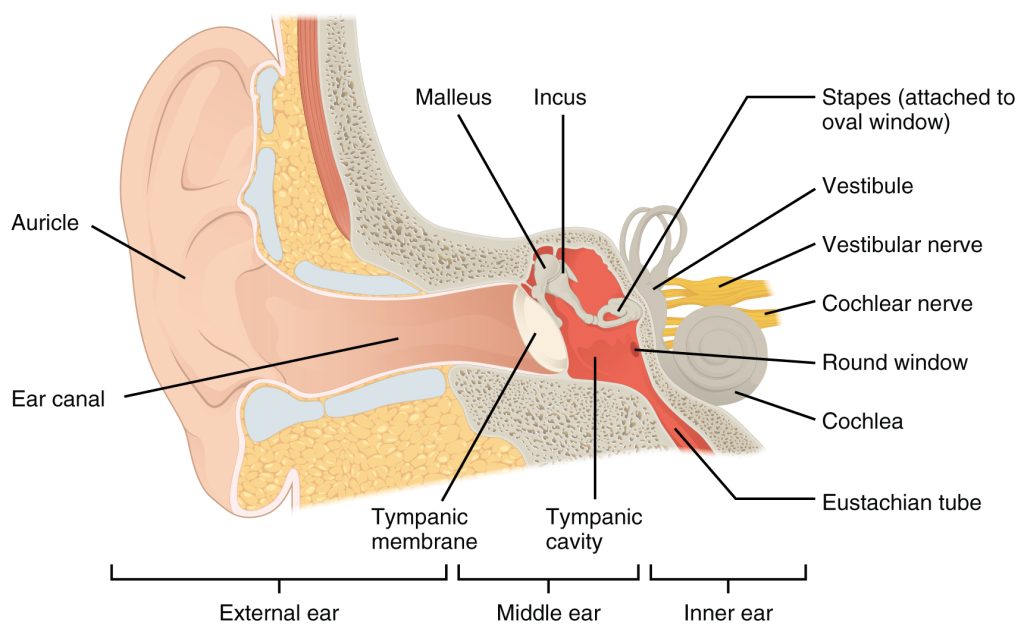
Hearing
Sound waves cause the tympanic membrane to vibrate. This vibration is amplified as it moves across the malleus, incus, and stapes and into the cochlea. Within the inner ear, the cochlear duct contains sound-transducing neurons. As the frequency of a sound changes, different hair cells within the cochlear duct are sensitive to a particular frequency. In this manner, the cochlea separates auditory stimuli by frequency and sends impulses to the brain stem via the cochlear nerve. The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 Hz, the range of sound that human ears can detect.[98]
Balance
Along with hearing, the inner ear is also responsible for the sense of balance. Semicircular canals in the vestibule have three ring-like extensions. One extension is oriented in the horizontal plane, and the other two are oriented in the vertical plane. Hair cells within the vestibule sense head position, head movement, and body motion. By comparing the relative movements of both the horizontal and vertical planes, the vestibular system can detect the direction of most head movements within three-dimensional space. However, medical conditions affecting the semicircular canals cause incorrect signals to be sent to the brain, resulting in a spinning type of dizziness called vertigo.
Review of Anatomy of the Ear on YouTube[99]
Common Ear Disorders
Hearing Loss
Hearing loss is classified as conductive hearing loss or sensorineural hearing loss. Conductive hearing loss occurs when something in the external or middle ear is obstructing the transmission of sound. For example, cerumen impaction or a perforated tympanic membrane can cause conductive hearing loss. Sensorineural hearing loss is caused by pathology of the inner ear, cranial nerve VIII, or auditory areas of the cerebral cortex. Presbycusis is sensorineural hearing loss that occurs with aging due to gradual nerve degeneration. Ototoxic medications can also cause sensorineural hearing loss by affecting the hair cells in the cochlea.
Acute Otitis Media
Acute otitis media is the medical diagnosis for a middle ear infection. Ear infections are a common illness in the pediatric population. Children between the ages of 6 months and 2 years are more susceptible to ear infections because of the size and shape of their Eustachian tubes. Acute otitis media typically occurs after an upper respiratory infection when the Eustachian tube becomes inflamed and the middle ear fills with fluid, causing ear pain and irritability. This fluid can become infected, causing purulent fluid and low-grade fever. Acute otitis media is diagnosed by a health care provider using an otoscope to examine the tympanic membrane for bulging and purulent fluid. If not treated, acute otitis media can potentially cause perforation of the tympanic membrane. Treating early acute otitis media with antibiotics is controversial in the United States due to the effort to prevent antibiotic resistance. However, the treatment goals are to control pain and treat infection with antibiotics if a bacterial infection is present.[100]
Some children develop recurrent ear infections that can cause hearing loss affecting their language development. For children experiencing recurring cases, a surgery called myringotomy surgery is performed by an otolaryngologist. During myringotomy surgery, a tympanostomy tube is placed in the tympanic membrane to drain fluid from the middle ear and prevent infection from developing. If a child has a tympanostomy tube in place, it is expected to see clear fluid in their ear canal as it drains out of the tube. See Figure 8.16[101] for an image of a tympanostomy tube in the ear.[102]
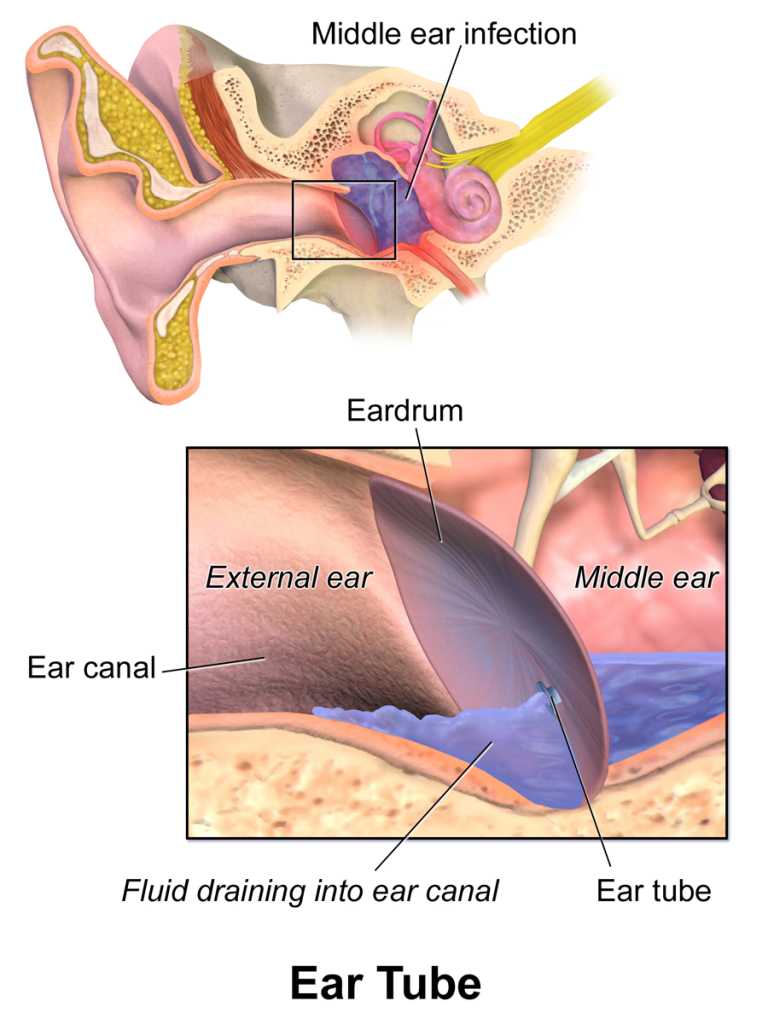
Otitis Externa
Otitis externa is the medical diagnosis for external ear inflammation and/or infection. See Figure 8.17[103] for an image of otitis externa. It is commonly known as “swimmer’s ear” because it commonly occurs in swimmers, especially in summer months. Otitis externa can occur in all age groups and causes an erythematous and edematous ear canal with associated yellow, white, or grey debris. Patients often report itching in the ear canal with pain that is worsened by pulling upwards and outwards on the auricle. Otitis externa is treated with antibiotic drops placed in the ear canals.[104]

Cerumen Impaction
Cerumen impaction refers to a buildup of earwax causing occlusion of the ear canal. This occlusion often causes symptoms such as hearing loss, ear fullness, and itching. See Figure 8.18[105] for an image of cerumen impaction. Cerumen can be removed via irrigation of the ear canal, ear drops to dissolve the wax, or manual removal.[106] In outpatient settings, nurses often assist with ear irrigation to remove cerumen impaction according to agency policy. See Figure 8.19[107] for an image of an ear irrigation procedure.


Tinnitus
Tinnitus is a ringing, buzzing, roaring, hissing, or whistling sound in the ears. The noise may be intermittent or continuous. Tinnitus can be caused by cerumen impaction, noise trauma, or ototoxic medications, such as diuretics or high doses of aspirin. Military personnel have a high incidence of tinnitus due to noise trauma from loud explosions and gunfire. There are no medications to treat tinnitus, but patients can be referred to an otolaryngologist for treatment such as cognitive therapy or noise masking.[108]
Vertigo
Vertigo is a type of dizziness that is often described by patients as, “the room feels as if it is spinning.” Benign positional vertigo (BPV) is a common condition caused by crystals becoming lodged in the semicircular canals in the vestibule of the inner ear that send false movement signals to the brain. BPV can be treated by trained professionals using a specific set of maneuvers that guide the crystals back to the chamber where they are supposed to be in the inner ear.[109]
Anatomy of the Eye
Our sense of vision occurs due to transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. See Figure 8.1[110] for an illustration of the eye. The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye. The inner surface of each lid is a thin membrane known as the conjunctiva. The conjunctiva extends over the white areas of the eye called the sclera, connecting the eyelids to the eyeball. The iris is the colored part of the eye. The iris is a smooth muscle that opens and closes the pupil, the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light. The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. The cornea, with the anterior chamber and lens, refracts light and contributes to vision. The cornea can be reshaped by surgical procedures such as LASIK. The innermost layer of the eye is the retina that contains the nervous tissue and specialized cells called photoreceptors for the initial processing of visual stimuli. Two types of photoreceptors within the retina are the rods and the cones. The cones are sensitive to different wavelengths of light and provide color vision. These nerve cells of the retina leave the eye and enter the brain via the optic nerve (cranial nerve II).[111]
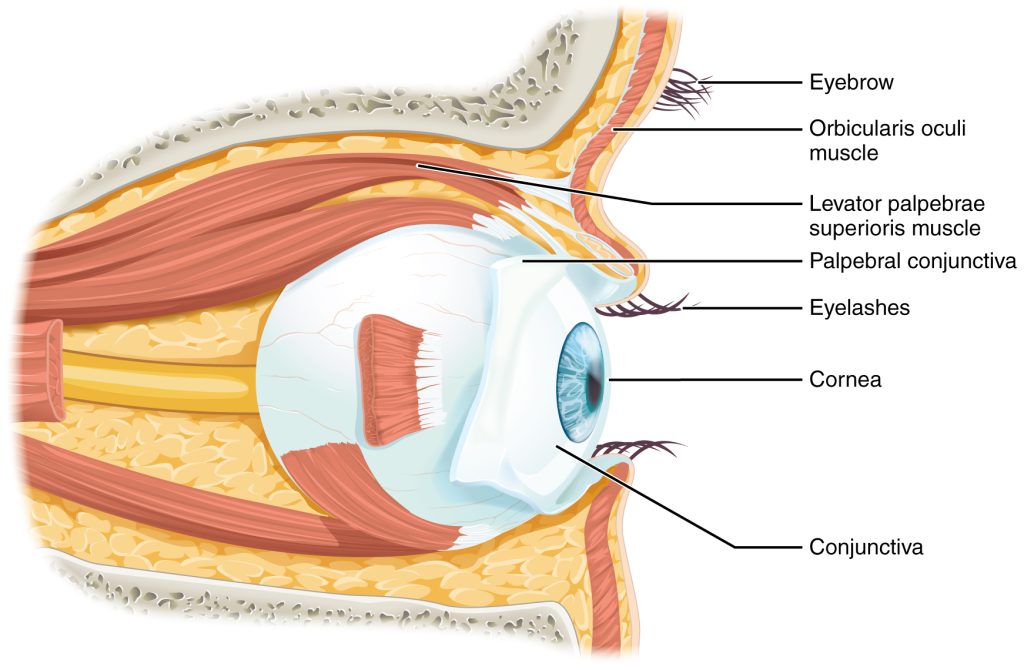
Tears are produced by the lacrimal gland that is located beneath the lateral edges of the nose. Tears flow through the lacrimal duct to the medial corner of the eye and flow over the conjunctiva to wash away foreign particles. Movement of the eye within the orbit occurs by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. The extraocular muscles are innervated by the abducens nerve, the trochlear nerve, and the oculomotor nerve (cranial nerves III, IV, and V).[112] See the illustration of the extraocular muscles in Figure 8.2.[113]
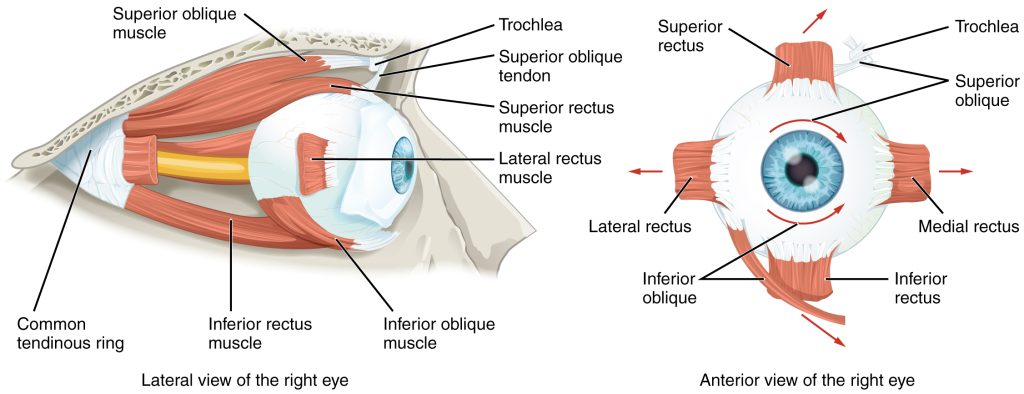
Review for Anatomy of the Eye on YouTube[114]
Common Disorders of the Eye
Eye disorders that nurses commonly see in practice include myopia, presbyopia, color blindness, dry eye, conjunctivitis, styes, cataracts, macular degeneration, and glaucoma.
Myopia
Myopia is impaired vision, also known as nearsightedness that makes far-away objects look blurry. It happens when the eyeball grows too long from front to back or when there are problems with the shape of the cornea or the lens. These problems make light focus in front of the retina, instead of on it, causing blurriness. See Figure 8.3[115] for a simulated image of a person’s vision with myopia. Nearsightedness usually becomes apparent between ages 6 and 14. It is corrected with glasses, contacts, or LASIK surgery.[116]

Presbyopia
Presbyopia is impaired near vision. It commonly occurs in middle-aged and older adults, making it difficult to clearly see objects up close. As people age, the lens in the eye gets harder and less flexible and stops focusing light correctly on the retina.[117] Presbyopia can be corrected with glasses and/or contacts. See Figure 8.4[118] for a simulated image of a person’s vision with presbyopia.
Color Blindness
Color blindness makes it difficult to differentiate between certain colors. Color blindness can occur due to damage to the eye or to the brain. There’s no cure for color blindness, but special glasses and contact lenses can help people differentiate between colors. Most people who have color blindness are able to use visual strategies related to color selection and don’t have problems participating in everyday activities.[119]
Dry Eye
Dry eye is a very common eye condition that occurs when the eyes don’t make enough tears to stay wet or the tears don’t work correctly. Symptoms of dry eye include a scratchy feeling, stinging, and burning. Treatment includes over-the-counter and prescription eye drops, as well as lifestyle changes to decrease the dryness of the eyes.[120]
Conjunctivitis
Conjunctivitis is a viral or bacterial infection that causes swelling and redness in the conjunctiva and sclera. See Figure 8.5[121] for an image of conjunctivitis. The eye may feel itchy and painful with crusty yellow drainage present. Conjunctivitis is very contagious, so the nurse should educate the patient and family caregivers to wash hands frequently. Additionally, the patient should not share items like pillowcases, towels, or makeup. Bacterial conjunctivitis is treated with antibiotic eye drops.[122]

Stye
A stye is a bacterial infection of an oil gland in the eyelid, causing a red, tender bump at the edge of the eyelid. See Figure 8.6[123] for an image of a stye. Treatment includes applying warm compresses to the eyelid and prescription eyedrops.[124]
Cataracts
A cataract is a cloudy area on the lens of the eye. Cataracts are very common in older adults. Over half of all Americans age 80 or older either have cataracts or have had surgery to remove cataracts. See Figure 8.7[125] for an image of a cataract. Cataracts develop slowly and symptoms include faded colors, blurred or double vision, halos around light, and trouble seeing at night. See Figure 8.8[126] for a simulated image of a person’s vision with cataracts. Decreased vision due to cataracts may result in trouble reading and driving and increases the risk of falling. Patients often undergo surgery for cataracts. During cataract surgery, the doctor removes the clouded lens and replaces it with a new, artificial lens.[127]
Macular Degeneration
Age-related macular degeneration is a common condition that causes blurred central vision. It is the leading cause of vision loss for people 50 and older. See Figure 8.9[128] for a simulated image of a person’s vision with macular degeneration. There are two types of macular degeneration: dry (nonexudative) and wet (exudative). During dry macular degeneration, cellular debris called drusen accumulates and scars the retina. In the wet (exudative) form, which is more severe, blood vessels grow behind the retina that leak exudate fluid, causing hemorrhaging and scarring. There is no treatment for dry macular degeneration, but laser therapy can be used to help treat wet (exudative) macular degeneration.[129]

Glaucoma
Glaucoma is a group of eye diseases that causes vision loss by damaging the optic nerve due to increased intraocular pressure. Treatment includes prescription eye drops to lower the pressure inside the eye and slow the progression of the disease. If not treated appropriately, glaucoma can cause blindness. Symptoms of glaucoma include gradual loss of peripheral vision. See Figure 8.10[130] for a simulated image of a person’s vision with glaucoma. Because the loss of vision occurs so slowly, many people don’t realize they have symptoms until the disease is well-progressed or it is discovered during an eye exam.[131]
Screening Tools for Eye Exams
Common screening tools used during an eye exam are the Snellen chart, a near vision chart, and Ishihara plates. Nurses working in outpatient settings or school settings use these tools when screening patients for vision problems. If a vision problem is identified, the patient is referred to an optometrist for further testing. When performing a vision assessment, be sure to provide adequate lighting.
Snellen Chart
Distant vision is tested by using the Snellen chart. See Figure 8.11[132] for an image of the Snellen chart. Place the patient 20 feet away from the Snellen chart. Ask them to cover one eye and read the letters from the lowest line they can see clearly. Record the corresponding fraction in the furthermost right-hand column. Repeat with the other eye. If the patient is wearing glasses or contact lens during this assessment, document the results as “corrected vision” when wearing these assistive devices.
A person with no visual impairment is documented as having 20/20 vision. A person with impaired vision has a different lower denominator of this fraction. For example, a vision measurement of 20/30 indicates the patient can see letters clearly at 20 feet that a person with normal vision can see clearly at 30 feet.[133] Alternative charts are also available for children or adults who can’t read letters in English. See Figure 8.12[134]for an alternative eye chart.
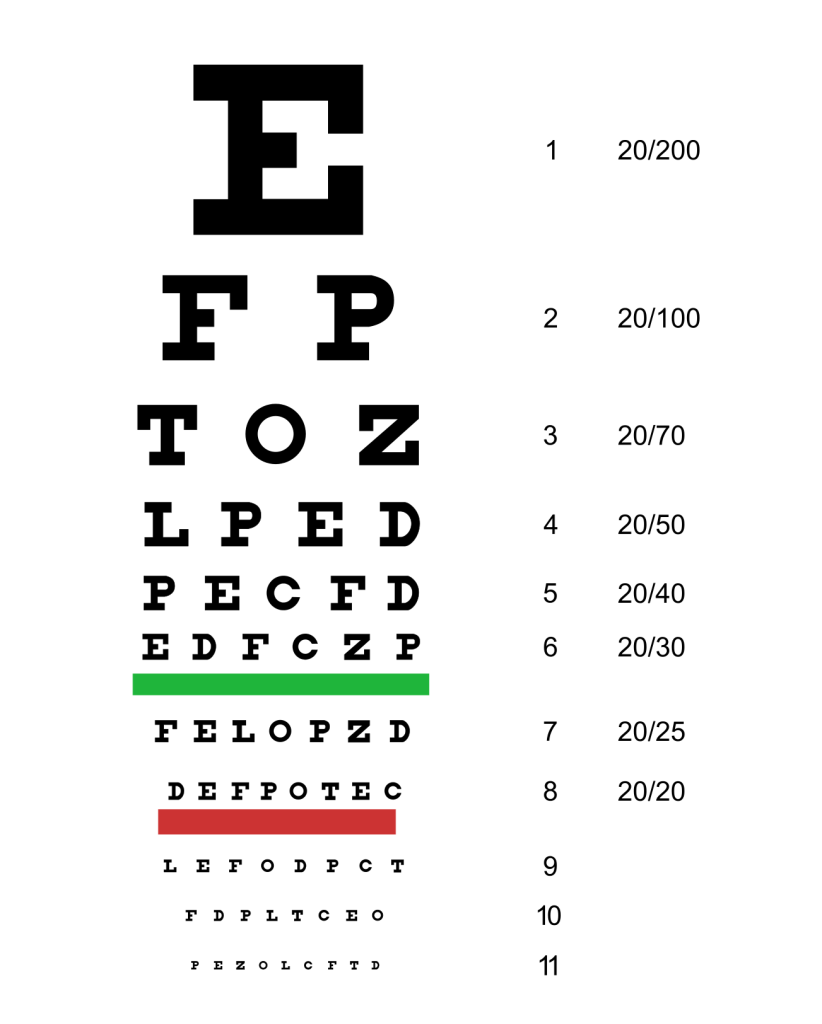

Near Vision
Near vision is assessed by having a patient read from a prepared card that is held 14 inches away from the eyes. If a card is not available, the patient can be asked to read from a newspaper as an alternative quick screening tool. See Figure 8.13[135] for an image of a prepared card used to assess near vision.
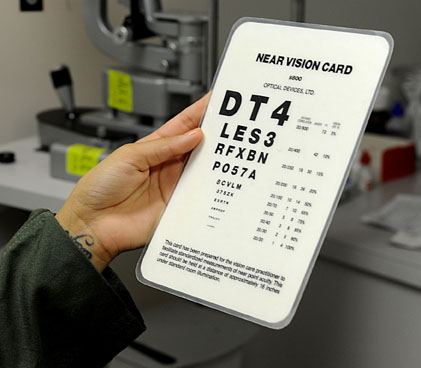
Ishihara Plates
Ishihara plates are commonly used to assess color vision. Each of the colored dotted plates shows either a number or a path. See Figure 8.14[136] for an example of Ishihara plates. A person with color blindness is not able to distinguish the numbers or paths from the other colored dots on the plate.
Anatomy of the Ear
Hearing is the transduction of sound waves into a neural signal by the structures of the ear. See Figure 8.15[137] for an image of the anatomy of the ear. The large, fleshy structure on the lateral aspect of the head is known as the auricle. The C-shaped curves of the auricle direct sound waves toward the ear canal. At the end of the ear canal is the tympanic membrane, commonly referred to as the eardrum, that vibrates after it is struck by sound waves. The auricle, ear canal, and tympanic membrane are referred to as the external ear. The middle ear consists of a space with three small bones called the malleus, incus, and stapes, the Latin names that roughly translate to “hammer,” “anvil,” and “stirrup.” The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is attached to the inner ear, where the sound waves are transduced into a neural signal. The middle ear is also connected to the pharynx through the Eustachian tube that helps equilibrate air pressure across the tympanic membrane. The Eustachian tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning. The inner ear is often described as a bony labyrinth because it is composed of a series of semicircular canals. The semicircular canals have two separate regions, the cochlea and the vestibule, that are responsible for hearing and balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, they travel together from the inner ear to the brain stem as the vestibulocochlear nerve (cranial nerve VIII).[138]
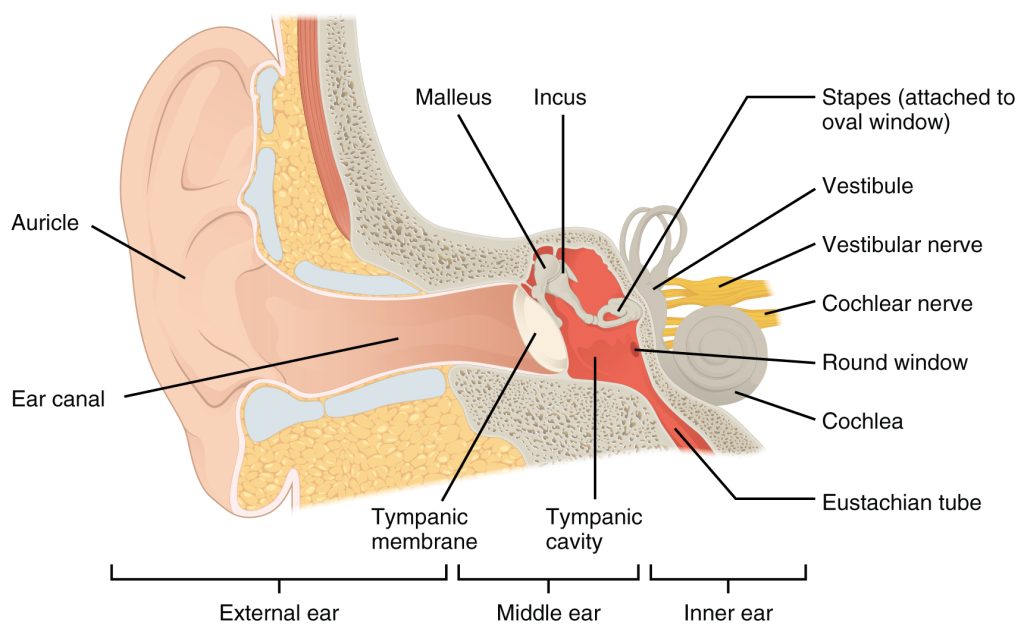
Hearing
Sound waves cause the tympanic membrane to vibrate. This vibration is amplified as it moves across the malleus, incus, and stapes and into the cochlea. Within the inner ear, the cochlear duct contains sound-transducing neurons. As the frequency of a sound changes, different hair cells within the cochlear duct are sensitive to a particular frequency. In this manner, the cochlea separates auditory stimuli by frequency and sends impulses to the brain stem via the cochlear nerve. The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 Hz, the range of sound that human ears can detect.[139]
Balance
Along with hearing, the inner ear is also responsible for the sense of balance. Semicircular canals in the vestibule have three ring-like extensions. One extension is oriented in the horizontal plane, and the other two are oriented in the vertical plane. Hair cells within the vestibule sense head position, head movement, and body motion. By comparing the relative movements of both the horizontal and vertical planes, the vestibular system can detect the direction of most head movements within three-dimensional space. However, medical conditions affecting the semicircular canals cause incorrect signals to be sent to the brain, resulting in a spinning type of dizziness called vertigo.
Review of Anatomy of the Ear on YouTube[140]
Common Ear Disorders
Hearing Loss
Hearing loss is classified as conductive hearing loss or sensorineural hearing loss. Conductive hearing loss occurs when something in the external or middle ear is obstructing the transmission of sound. For example, cerumen impaction or a perforated tympanic membrane can cause conductive hearing loss. Sensorineural hearing loss is caused by pathology of the inner ear, cranial nerve VIII, or auditory areas of the cerebral cortex. Presbycusis is sensorineural hearing loss that occurs with aging due to gradual nerve degeneration. Ototoxic medications can also cause sensorineural hearing loss by affecting the hair cells in the cochlea.
Acute Otitis Media
Acute otitis media is the medical diagnosis for a middle ear infection. Ear infections are a common illness in the pediatric population. Children between the ages of 6 months and 2 years are more susceptible to ear infections because of the size and shape of their Eustachian tubes. Acute otitis media typically occurs after an upper respiratory infection when the Eustachian tube becomes inflamed and the middle ear fills with fluid, causing ear pain and irritability. This fluid can become infected, causing purulent fluid and low-grade fever. Acute otitis media is diagnosed by a health care provider using an otoscope to examine the tympanic membrane for bulging and purulent fluid. If not treated, acute otitis media can potentially cause perforation of the tympanic membrane. Treating early acute otitis media with antibiotics is controversial in the United States due to the effort to prevent antibiotic resistance. However, the treatment goals are to control pain and treat infection with antibiotics if a bacterial infection is present.[141]
Some children develop recurrent ear infections that can cause hearing loss affecting their language development. For children experiencing recurring cases, a surgery called myringotomy surgery is performed by an otolaryngologist. During myringotomy surgery, a tympanostomy tube is placed in the tympanic membrane to drain fluid from the middle ear and prevent infection from developing. If a child has a tympanostomy tube in place, it is expected to see clear fluid in their ear canal as it drains out of the tube. See Figure 8.16[142] for an image of a tympanostomy tube in the ear.[143]
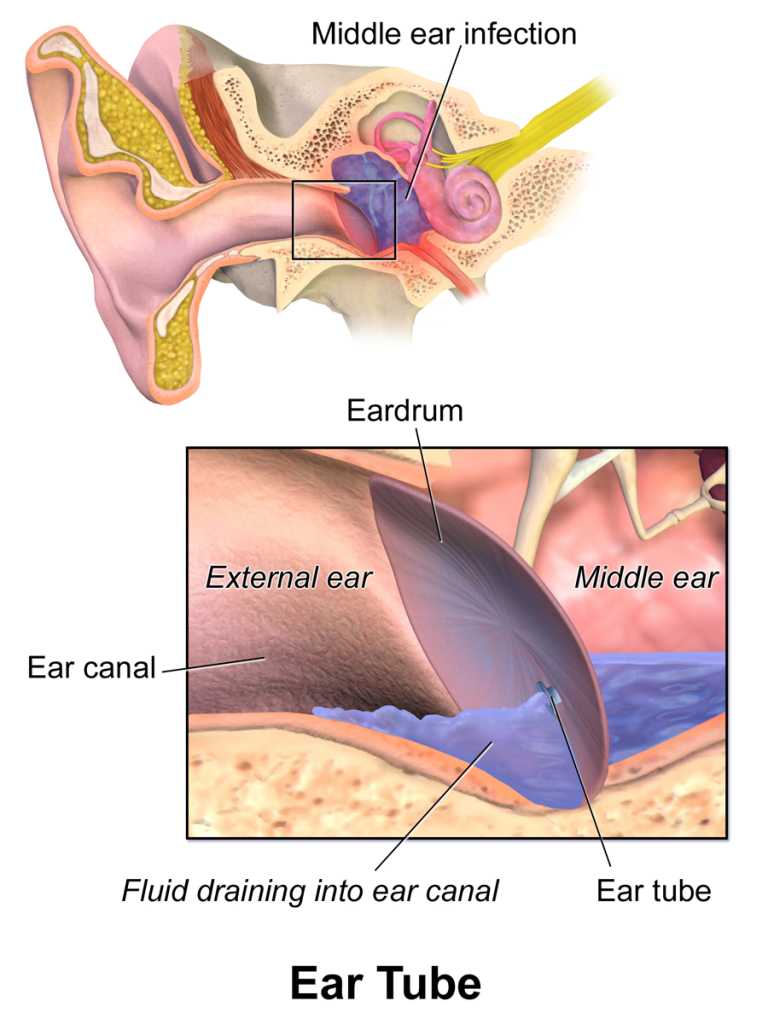
Otitis Externa
Otitis externa is the medical diagnosis for external ear inflammation and/or infection. See Figure 8.17[144] for an image of otitis externa. It is commonly known as “swimmer’s ear” because it commonly occurs in swimmers, especially in summer months. Otitis externa can occur in all age groups and causes an erythematous and edematous ear canal with associated yellow, white, or grey debris. Patients often report itching in the ear canal with pain that is worsened by pulling upwards and outwards on the auricle. Otitis externa is treated with antibiotic drops placed in the ear canals.[145]

Cerumen Impaction
Cerumen impaction refers to a buildup of earwax causing occlusion of the ear canal. This occlusion often causes symptoms such as hearing loss, ear fullness, and itching. See Figure 8.18[146] for an image of cerumen impaction. Cerumen can be removed via irrigation of the ear canal, ear drops to dissolve the wax, or manual removal.[147] In outpatient settings, nurses often assist with ear irrigation to remove cerumen impaction according to agency policy. See Figure 8.19[148] for an image of an ear irrigation procedure.


Tinnitus
Tinnitus is a ringing, buzzing, roaring, hissing, or whistling sound in the ears. The noise may be intermittent or continuous. Tinnitus can be caused by cerumen impaction, noise trauma, or ototoxic medications, such as diuretics or high doses of aspirin. Military personnel have a high incidence of tinnitus due to noise trauma from loud explosions and gunfire. There are no medications to treat tinnitus, but patients can be referred to an otolaryngologist for treatment such as cognitive therapy or noise masking.[149]
Vertigo
Vertigo is a type of dizziness that is often described by patients as, “the room feels as if it is spinning.” Benign positional vertigo (BPV) is a common condition caused by crystals becoming lodged in the semicircular canals in the vestibule of the inner ear that send false movement signals to the brain. BPV can be treated by trained professionals using a specific set of maneuvers that guide the crystals back to the chamber where they are supposed to be in the inner ear.[150]
Muscles other than the diaphragm and intercostal muscles that may be used for labored breathing.
With an understanding of the basic structures and primary functions of the respiratory system, the nurse collects subjective and objective data to perform a focused respiratory assessment.
Subjective Assessment
Collect data using interview questions, paying particular attention to what the patient is reporting. The interview should include questions regarding any current and past history of respiratory health conditions or illnesses, medications, and reported symptoms. Consider the patient’s age, gender, family history, race, culture, environmental factors, and current health practices when gathering subjective data. The information discovered during the interview process guides the physical exam and subsequent patient education. See Table 10.3a for sample interview questions to use during a focused respiratory assessment.[151]
Table 10.3a Interview Questions for Subjective Assessment of the Respiratory System
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a respiratory condition, such as asthma, COPD, pneumonia, or allergies?
Do you use oxygen or peak flow meter? Do you use home respiratory equipment like CPAP, BiPAP, or nebulizer devices? |
Please describe the conditions and treatments. |
| Are you currently taking any medications, herbs, or supplements for respiratory concerns? | Please identify what you are taking and the purpose of each. |
| Have you had any feelings of breathlessness
(dyspnea)? |
Note: If the shortness of breath is severe or associated with chest pain, discontinue the interview and obtain emergency assistance.
Are you having any shortness of breath now? If yes, please rate the shortness of breath from 0-10 with "0" being none and "10" being severe? Does anything bring on the shortness of breath (such as activity, animals, food, or dust)? If activity causes the shortness of breath, how much exertion is required to bring on the shortness of breath? When did the shortness of breath start? Is the shortness of breath associated with chest pain or discomfort? How long does the shortness of breath last? What makes the shortness of breath go away? Is the shortness of breath related to a position, like lying down? Do you sleep in a recliner or upright in bed? Do you wake up at night feeling short of breath? How many pillows do you sleep on? How does the shortness of breath affect your daily activities? |
| Do you have a cough? | When you cough, do you bring up anything? What color is the phlegm?
Do you cough up any blood (hemoptysis)? Do you have any associated symptoms with the cough such as fever, chills, or night sweats? How long have you had the cough? Does anything bring on the cough (such as activity, dust, animals, or change in position)? What have you used to treat the cough? Has it been effective? |
| Do you smoke or vape? | What products do you smoke/vape? If cigarettes are smoked, how many packs a day do you smoke?
How long have you smoked/vaped? Have you ever tried to quit smoking/vaping? What strategies gave you the best success? Are you interested in quitting smoking/vaping? If the patient is ready to quit, the five successful interventions are the "5 A's": Ask, Advise, Assess, Assist, and Arrange. Ask - Identify and document smoking status for every patient at every visit. Advise - In a clear, strong, and personalized manner, urge every user to quit. Assess - Is the user willing to make a quitting attempt at this time? Assist - For the patient willing to make a quitting attempt, use counseling and pharmacotherapy to help them quit. Arrange - Schedule follow-up contact, in person or by telephone, preferably within the first week after the quit date.[152] |
Life Span Considerations
Depending on the age and capability of the child, subjective data may also need to be retrieved from a parent and/or legal guardian.
Pediatric
- Is your child up-to-date with recommended immunizations?
- Is your child experiencing any cold symptoms (such as runny nose, cough, or nasal congestion)?
- How is your child’s appetite? Is there any decrease or change recently in appetite or wet diapers?
- Does your child have any hospitalization history related to respiratory illness?
- Did your child have any history of frequent ear infections as an infant?
Older Adult
- Have you noticed a change in your breathing?
- Do you get short of breath with activities that you did not before?
- Can you describe your energy level? Is there any change from previous?
Objective Assessment
A focused respiratory objective assessment includes interpretation of vital signs; inspection of the patient’s breathing pattern, skin color, and respiratory status; palpation to identify abnormalities; and auscultation of lung sounds using a stethoscope. For more information regarding interpreting vital signs, see the “General Survey” chapter. The nurse must have an understanding of what is expected for the patient’s age, gender, development, race, culture, environmental factors, and current health condition to determine the meaning of the data that is being collected.
Evaluate Vital Signs
The vital signs may be taken by the nurse or delegated to unlicensed assistive personnel such as a nursing assistant or medical assistant. Evaluate the respiratory rate and pulse oximetry readings to verify the patient is stable before proceeding with the physical exam. The normal range of a respiratory rate for an adult is 12-20 breaths per minute at rest, and the normal range for oxygen saturation of the blood is 94–98% (SpO₂).[153] Bradypnea is less than 12 breaths per minute, and tachypnea is greater than 20 breaths per minute.
Inspection
Inspection during a focused respiratory assessment includes observation of level of consciousness, breathing rate, pattern and effort, skin color, chest configuration, and symmetry of expansion.
- Assess the level of consciousness. The patient should be alert and cooperative. Hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide) can cause a decreased level of consciousness, irritability, anxiousness, restlessness, or confusion.
- Obtain the respiratory rate over a full minute. The normal range for the respiratory rate of an adult is 12-20 breaths per minute.
- Observe the breathing pattern, including the rhythm, effort, and use of accessory muscles. Breathing effort should be nonlabored and in a regular rhythm. Observe the depth of respiration and note if the respiration is shallow or deep. Pursed-lip breathing, nasal flaring, audible breathing, intercostal retractions, anxiety, and use of accessory muscles are signs of respiratory difficulty. Inspiration should last half as long as expiration unless the patient is active, in which case the inspiration-expiration ratio increases to 1:1.
- Observe the pattern of expiration and patient position. Patients who experience difficulty expelling air, such as those with emphysema, may have prolonged expiration cycles. Some patients may experience difficulty with breathing specifically when lying down. This symptom is known as orthopnea. Additionally, patients who are experiencing significant breathing difficulty may experience most relief while in a “tripod” position. This can be achieved by having the patient sit at the side of the bed with legs dangling toward the floor. The patient can then rest their arms on an overbed table to allow for maximum lung expansion. This position mimics the same position you might take at the end of running a race when you lean over and place your hands on your knees to “catch your breath.”
- Observe the patient’s color in their lips, face, hands, and feet. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctivae, or inner aspect of the lower lip. Cyanosis is a bluish discoloration of the skin, lips, and nail beds, which may indicate decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes and usually the result of reduced blood flow, oxygenation, or decreased number of red blood cells.
- Inspect the chest for symmetry and configuration. The trachea should be midline, and the clavicles should be symmetrical. See Figure 10.2[154] for visual landmarks when inspecting the thorax anteriorly, posteriorly, and laterally. Note the location of the ribs, sternum, clavicle, and scapula, as well as the underlying lobes of the lungs.
- Chest movement should be symmetrical on inspiration and expiration.
- Observe the anterior-posterior diameter of the patient’s chest and compare to the transverse diameter. The expected anteroposterior-transverse ratio should be 1:2. A patient with a 1:1 ratio is described as barrel-chested. This ratio is often seen in patients with chronic obstructive pulmonary disease due to hyperinflation of the lungs. See Figure 10.3[155] for an image of a patient with a barrel chest.
- Older patients may have changes in their anatomy, such as kyphosis, an outward curvature of the spine.
- Inspect the fingers for clubbing if the patient has a history of chronic respiratory disease. Clubbing is a bulbous enlargement of the tips of the fingers due to chronic hypoxia. See Figure 10.4[156] for an image of clubbing.
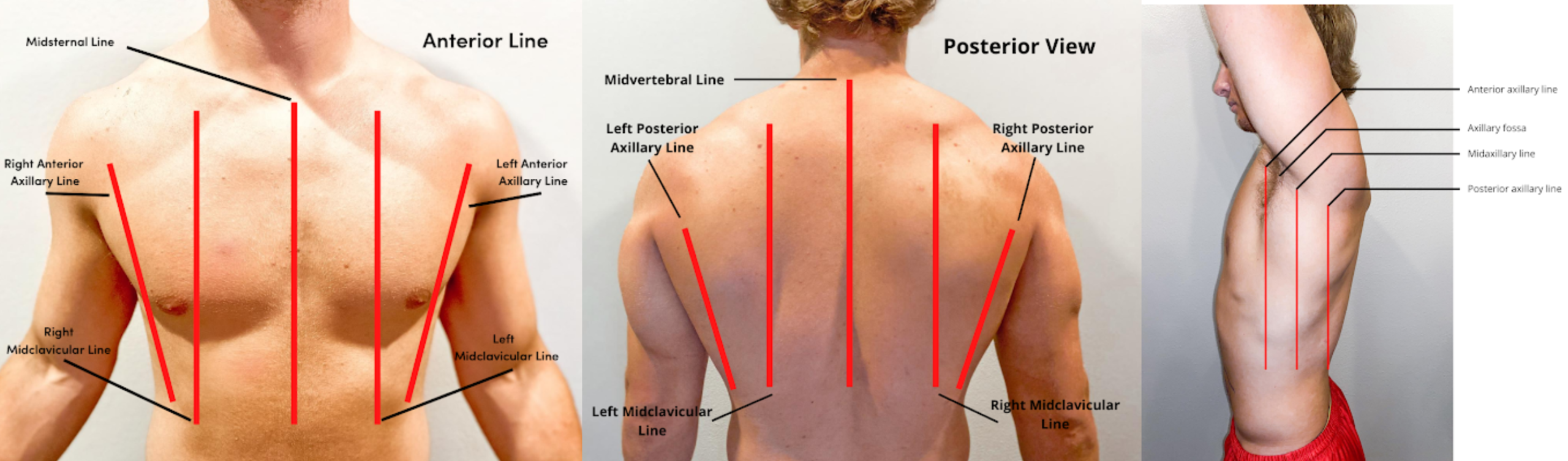


Palpation
- Palpation of the chest may be performed to investigate for areas of abnormality related to injury or procedural complications. For example, if a patient has a chest tube or has recently had one removed, the nurse may palpate near the tube insertion site to assess for areas of air leak or crepitus. Crepitus feels like a popping or crackling sensation when the skin is palpated and is a sign of air trapped under the subcutaneous tissues. If palpating the chest, use light pressure with the fingertips to examine the anterior and posterior chest wall. Chest palpation may be performed to assess specifically for growths, masses, crepitus, pain, or tenderness.
- Confirm symmetric chest expansion by placing your hands on the anterior or posterior chest at the same level, with thumbs over the sternum anteriorly or the spine posteriorly. As the patient inhales, your thumbs should move apart symmetrically. Unequal expansion can occur with pneumonia, thoracic trauma, such as fractured ribs, or pneumothorax.
Auscultation
Using the diaphragm of the stethoscope, listen to the movement of air through the airways during inspiration and expiration. Instruct the patient to take deep breaths through their mouth. Listen through the entire respiratory cycle because different sounds may be heard on inspiration and expiration. Allow the patient to rest between respiratory cycles, if needed, to avoid fatigue with deep breathing during auscultation. As you move across the different lung fields, the sounds produced by airflow vary depending on the area you are auscultating because the size of the airways change.
Correct placement of the stethoscope during auscultation of lung sounds is important to obtain a quality assessment. The stethoscope should not be placed over clothes or hair because these may create inaccurate sounds from friction. The best position to listen to lung sounds is with the patient sitting upright; however, if the patient is acutely ill or unable to sit upright, turn them side to side in a lying position. Avoid listening over bones, such as the scapulae or clavicles or over the female breasts to ensure you are hearing adequate sound transmission. Listen to sounds from side to side rather than down one side and then down the other side. This side-to-side pattern allows you to compare sounds in symmetrical lung fields. See Figures 10.5[157] and 10.6[158] for landmarks of stethoscope placement over the anterior and posterior chest wall.
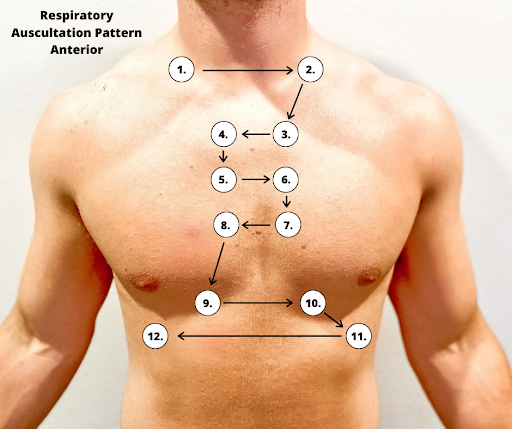
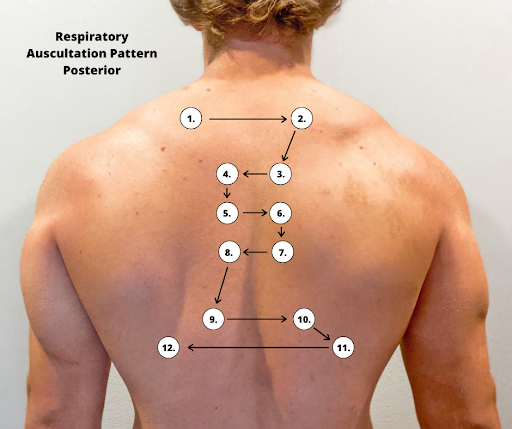
Expected Breath Sounds
It is important upon auscultation to have awareness of expected breath sounds in various anatomical locations.
- Bronchial breath sounds are heard over the trachea and larynx and are high-pitched and loud.
- Bronchovesicular sounds are medium-pitched and heard over the major bronchi.
- Vesicular breath sounds are heard over the lung surfaces, are lower-pitched, and often described as soft, rustling sounds.
Adventitious Lung Sounds
Adventitious lung sounds are sounds heard in addition to normal breath sounds. They most often indicate an airway problem or disease, such as accumulation of mucus or fluids in the airways, obstruction, inflammation, or infection. These sounds include rales/crackles, rhonchi/wheezes, stridor, and pleural rub:
- Coarse crackles, also called rhonchi, are low-pitched, loud, continuous sounds frequently heard on expiration. They are a sign of turbulent airflow through secretions in the large airways.
Rhonchi Lung Sounds on YouTube [159]
- Fine crackles, also called rales, are popping or crackling sounds heard on inspiration. They occur in association with conditions that cause fluid to accumulate within the alveolar and interstitial spaces, such as heart failure or pneumonia. Fine crackles are soft, high-pitched, and very brief. For this reason, it is essential to listen to lung sounds with the stethoscope placed on the patient's skin and not over their clothing or hospital gown. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling-type noises produced during expiration (and sometimes inspiration) when air is forced through airways narrowed by bronchoconstriction or associated mucosal edema. For example, patients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with mechanical obstruction at the level of the trachea/upper airway.
- Pleural rub may be heard on either inspiration or expiration and sounds like the rubbing together of leather. A pleural rub is heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other.[160]
Life Span Considerations
Children
There are various respiratory assessment considerations that should be noted with assessment of children.
- The respiratory rate in children less than 12 months of age can range from 30-60 breaths per minute, depending on whether the infant is asleep or active.
- Infants have irregular or periodic newborn breathing in the first few weeks of life; therefore, it is important to count the respirations for a full minute. During this time, you may notice periods of apnea lasting up to 10 seconds. This is not abnormal unless the infant is showing other signs of distress. Signs of respiratory distress in infants and children include nasal flaring and sternal or intercostal retractions.
- Up to three months of age, infants are considered “obligate” nose-breathers, meaning their breathing is primarily through the nose.
- The anteroposterior-transverse ratio is typically 1:1 until the thoracic muscles are fully developed around six years of age.
Older Adults
As the adult person ages, the cartilage and muscle support of the thorax becomes weakened and less flexible, resulting in a decrease in chest expansion. Older adults may also have weakened respiratory muscles, and breathing may become shallower. The anteroposterior-transverse ratio may be 1:1 if there is significant curvature of the spine (kyphosis).
Percussion
Percussion is an advanced respiratory assessment technique that is used by advanced practice nurses and other health care providers to gather additional data in the underlying lung tissue. By striking the fingers of one hand over the fingers of the other hand, a sound is produced over the lung fields that helps determine if fluid is present. Dull sounds are heard with high-density areas, such as pneumonia or atelectasis, whereas clear, low-pitched, hollow sounds are heard in normal lung tissue.
![]()
- Because infants breathe primarily through the nose, nasal congestion can limit the amount of air getting into the lungs.
- Attempt to assess an infant’s respiratory rate while the infant is at rest and content rather than when the infant is crying. Counting respirations by observing abdominal breathing movements may be easier for the novice nurse than counting breath sounds, as it can be difficult to differentiate lung and heart sounds when auscultating newborns.
- Auscultation of lungs during crying is not a problem. It will enhance breath sounds.
- The older patient may have a weakening of muscles that support respiration and breathing. Therefore, the patient may report tiring easily during the assessment when taking deep breaths. Break up the assessment by listening to the anterior lung sounds and then the heart sounds and allowing the patient to rest before listening to the posterior lung sounds.
- Patients with end-stage COPD may have diminished lung sounds due to decreased air movement. This abnormal assessment finding may be the patient’s baseline or normal and might also include wheezes and fine crackles as a result of chronic excess secretions and/or bronchoconstriction.[161],[162]
Expected Versus Unexpected Findings
See Table 10.3b for a comparison of expected versus unexpected findings when assessing the respiratory system.[163]
Table 10.3b Expected Versus Unexpected Respiratory Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if a new finding*) |
|---|---|---|
| Inspection | Work of breathing effortless
Regular breathing pattern Respiratory rate within normal range for age Chest expansion symmetrical Absence of cyanosis or pallor Absence of accessory muscle use, retractions, and/or nasal flaring Anteroposterior: transverse diameter ratio 1:2 |
Labored breathing
Irregular rhythm Increased or decreased respiratory rate Accessory muscle use, pursed-lip breathing, nasal flaring (infants), and/or retractions Presence of cyanosis or pallor Asymmetrical chest expansion Clubbing of fingernails |
| Palpation | No pain or tenderness with palpation. Skin warm and dry; no crepitus or masses | Pain or tenderness with palpation, crepitus, palpable masses, or lumps |
| Percussion | Clear, low-pitched, hollow sound in normal lung tissue | Dull sounds heard with high-density areas, such as pneumonia or atelectasis |
| Auscultation | Bronchovesicular and vesicular sounds heard over appropriate areas
Absence of adventitious lung sounds |
Diminished lung sounds
Adventitious lung sounds, such as fine crackles/rales, wheezing, stridor, or pleural rub |
| *CRITICAL CONDITIONS to report immediately | Decreased oxygen saturation <92%[164]
Pain Worsening dyspnea Decreased level of consciousness, restlessness, anxiousness, and/or irritability |
With an understanding of the basic structures and primary functions of the respiratory system, the nurse collects subjective and objective data to perform a focused respiratory assessment.
Subjective Assessment
Collect data using interview questions, paying particular attention to what the patient is reporting. The interview should include questions regarding any current and past history of respiratory health conditions or illnesses, medications, and reported symptoms. Consider the patient’s age, gender, family history, race, culture, environmental factors, and current health practices when gathering subjective data. The information discovered during the interview process guides the physical exam and subsequent patient education. See Table 10.3a for sample interview questions to use during a focused respiratory assessment.[165]
Table 10.3a Interview Questions for Subjective Assessment of the Respiratory System
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a respiratory condition, such as asthma, COPD, pneumonia, or allergies?
Do you use oxygen or peak flow meter? Do you use home respiratory equipment like CPAP, BiPAP, or nebulizer devices? |
Please describe the conditions and treatments. |
| Are you currently taking any medications, herbs, or supplements for respiratory concerns? | Please identify what you are taking and the purpose of each. |
| Have you had any feelings of breathlessness
(dyspnea)? |
Note: If the shortness of breath is severe or associated with chest pain, discontinue the interview and obtain emergency assistance.
Are you having any shortness of breath now? If yes, please rate the shortness of breath from 0-10 with "0" being none and "10" being severe? Does anything bring on the shortness of breath (such as activity, animals, food, or dust)? If activity causes the shortness of breath, how much exertion is required to bring on the shortness of breath? When did the shortness of breath start? Is the shortness of breath associated with chest pain or discomfort? How long does the shortness of breath last? What makes the shortness of breath go away? Is the shortness of breath related to a position, like lying down? Do you sleep in a recliner or upright in bed? Do you wake up at night feeling short of breath? How many pillows do you sleep on? How does the shortness of breath affect your daily activities? |
| Do you have a cough? | When you cough, do you bring up anything? What color is the phlegm?
Do you cough up any blood (hemoptysis)? Do you have any associated symptoms with the cough such as fever, chills, or night sweats? How long have you had the cough? Does anything bring on the cough (such as activity, dust, animals, or change in position)? What have you used to treat the cough? Has it been effective? |
| Do you smoke or vape? | What products do you smoke/vape? If cigarettes are smoked, how many packs a day do you smoke?
How long have you smoked/vaped? Have you ever tried to quit smoking/vaping? What strategies gave you the best success? Are you interested in quitting smoking/vaping? If the patient is ready to quit, the five successful interventions are the "5 A's": Ask, Advise, Assess, Assist, and Arrange. Ask - Identify and document smoking status for every patient at every visit. Advise - In a clear, strong, and personalized manner, urge every user to quit. Assess - Is the user willing to make a quitting attempt at this time? Assist - For the patient willing to make a quitting attempt, use counseling and pharmacotherapy to help them quit. Arrange - Schedule follow-up contact, in person or by telephone, preferably within the first week after the quit date.[166] |
Life Span Considerations
Depending on the age and capability of the child, subjective data may also need to be retrieved from a parent and/or legal guardian.
Pediatric
- Is your child up-to-date with recommended immunizations?
- Is your child experiencing any cold symptoms (such as runny nose, cough, or nasal congestion)?
- How is your child’s appetite? Is there any decrease or change recently in appetite or wet diapers?
- Does your child have any hospitalization history related to respiratory illness?
- Did your child have any history of frequent ear infections as an infant?
Older Adult
- Have you noticed a change in your breathing?
- Do you get short of breath with activities that you did not before?
- Can you describe your energy level? Is there any change from previous?
Objective Assessment
A focused respiratory objective assessment includes interpretation of vital signs; inspection of the patient’s breathing pattern, skin color, and respiratory status; palpation to identify abnormalities; and auscultation of lung sounds using a stethoscope. For more information regarding interpreting vital signs, see the “General Survey” chapter. The nurse must have an understanding of what is expected for the patient’s age, gender, development, race, culture, environmental factors, and current health condition to determine the meaning of the data that is being collected.
Evaluate Vital Signs
The vital signs may be taken by the nurse or delegated to unlicensed assistive personnel such as a nursing assistant or medical assistant. Evaluate the respiratory rate and pulse oximetry readings to verify the patient is stable before proceeding with the physical exam. The normal range of a respiratory rate for an adult is 12-20 breaths per minute at rest, and the normal range for oxygen saturation of the blood is 94–98% (SpO₂).[167] Bradypnea is less than 12 breaths per minute, and tachypnea is greater than 20 breaths per minute.
Inspection
Inspection during a focused respiratory assessment includes observation of level of consciousness, breathing rate, pattern and effort, skin color, chest configuration, and symmetry of expansion.
- Assess the level of consciousness. The patient should be alert and cooperative. Hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide) can cause a decreased level of consciousness, irritability, anxiousness, restlessness, or confusion.
- Obtain the respiratory rate over a full minute. The normal range for the respiratory rate of an adult is 12-20 breaths per minute.
- Observe the breathing pattern, including the rhythm, effort, and use of accessory muscles. Breathing effort should be nonlabored and in a regular rhythm. Observe the depth of respiration and note if the respiration is shallow or deep. Pursed-lip breathing, nasal flaring, audible breathing, intercostal retractions, anxiety, and use of accessory muscles are signs of respiratory difficulty. Inspiration should last half as long as expiration unless the patient is active, in which case the inspiration-expiration ratio increases to 1:1.
- Observe the pattern of expiration and patient position. Patients who experience difficulty expelling air, such as those with emphysema, may have prolonged expiration cycles. Some patients may experience difficulty with breathing specifically when lying down. This symptom is known as orthopnea. Additionally, patients who are experiencing significant breathing difficulty may experience most relief while in a “tripod” position. This can be achieved by having the patient sit at the side of the bed with legs dangling toward the floor. The patient can then rest their arms on an overbed table to allow for maximum lung expansion. This position mimics the same position you might take at the end of running a race when you lean over and place your hands on your knees to “catch your breath.”
- Observe the patient’s color in their lips, face, hands, and feet. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctivae, or inner aspect of the lower lip. Cyanosis is a bluish discoloration of the skin, lips, and nail beds, which may indicate decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes and usually the result of reduced blood flow, oxygenation, or decreased number of red blood cells.
- Inspect the chest for symmetry and configuration. The trachea should be midline, and the clavicles should be symmetrical. See Figure 10.2[168] for visual landmarks when inspecting the thorax anteriorly, posteriorly, and laterally. Note the location of the ribs, sternum, clavicle, and scapula, as well as the underlying lobes of the lungs.
- Chest movement should be symmetrical on inspiration and expiration.
- Observe the anterior-posterior diameter of the patient’s chest and compare to the transverse diameter. The expected anteroposterior-transverse ratio should be 1:2. A patient with a 1:1 ratio is described as barrel-chested. This ratio is often seen in patients with chronic obstructive pulmonary disease due to hyperinflation of the lungs. See Figure 10.3[169] for an image of a patient with a barrel chest.
- Older patients may have changes in their anatomy, such as kyphosis, an outward curvature of the spine.
- Inspect the fingers for clubbing if the patient has a history of chronic respiratory disease. Clubbing is a bulbous enlargement of the tips of the fingers due to chronic hypoxia. See Figure 10.4[170] for an image of clubbing.
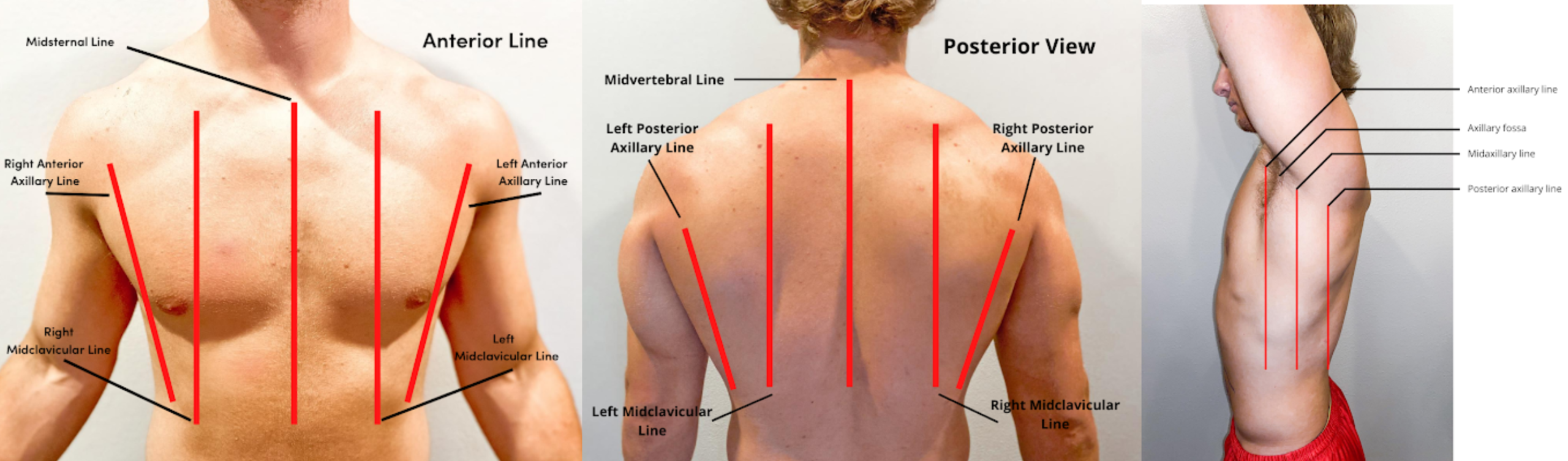


Palpation
- Palpation of the chest may be performed to investigate for areas of abnormality related to injury or procedural complications. For example, if a patient has a chest tube or has recently had one removed, the nurse may palpate near the tube insertion site to assess for areas of air leak or crepitus. Crepitus feels like a popping or crackling sensation when the skin is palpated and is a sign of air trapped under the subcutaneous tissues. If palpating the chest, use light pressure with the fingertips to examine the anterior and posterior chest wall. Chest palpation may be performed to assess specifically for growths, masses, crepitus, pain, or tenderness.
- Confirm symmetric chest expansion by placing your hands on the anterior or posterior chest at the same level, with thumbs over the sternum anteriorly or the spine posteriorly. As the patient inhales, your thumbs should move apart symmetrically. Unequal expansion can occur with pneumonia, thoracic trauma, such as fractured ribs, or pneumothorax.
Auscultation
Using the diaphragm of the stethoscope, listen to the movement of air through the airways during inspiration and expiration. Instruct the patient to take deep breaths through their mouth. Listen through the entire respiratory cycle because different sounds may be heard on inspiration and expiration. Allow the patient to rest between respiratory cycles, if needed, to avoid fatigue with deep breathing during auscultation. As you move across the different lung fields, the sounds produced by airflow vary depending on the area you are auscultating because the size of the airways change.
Correct placement of the stethoscope during auscultation of lung sounds is important to obtain a quality assessment. The stethoscope should not be placed over clothes or hair because these may create inaccurate sounds from friction. The best position to listen to lung sounds is with the patient sitting upright; however, if the patient is acutely ill or unable to sit upright, turn them side to side in a lying position. Avoid listening over bones, such as the scapulae or clavicles or over the female breasts to ensure you are hearing adequate sound transmission. Listen to sounds from side to side rather than down one side and then down the other side. This side-to-side pattern allows you to compare sounds in symmetrical lung fields. See Figures 10.5[171] and 10.6[172] for landmarks of stethoscope placement over the anterior and posterior chest wall.
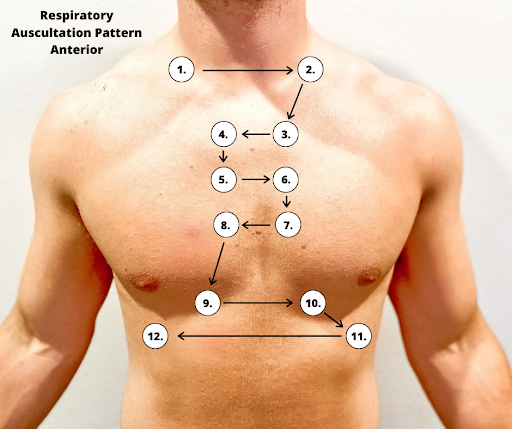
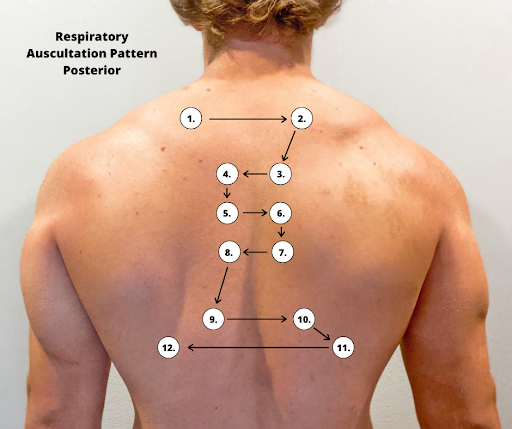
Expected Breath Sounds
It is important upon auscultation to have awareness of expected breath sounds in various anatomical locations.
- Bronchial breath sounds are heard over the trachea and larynx and are high-pitched and loud.
- Bronchovesicular sounds are medium-pitched and heard over the major bronchi.
- Vesicular breath sounds are heard over the lung surfaces, are lower-pitched, and often described as soft, rustling sounds.
Adventitious Lung Sounds
Adventitious lung sounds are sounds heard in addition to normal breath sounds. They most often indicate an airway problem or disease, such as accumulation of mucus or fluids in the airways, obstruction, inflammation, or infection. These sounds include rales/crackles, rhonchi/wheezes, stridor, and pleural rub:
- Coarse crackles, also called rhonchi, are low-pitched, loud, continuous sounds frequently heard on expiration. They are a sign of turbulent airflow through secretions in the large airways.
Rhonchi Lung Sounds on YouTube [173]
- Fine crackles, also called rales, are popping or crackling sounds heard on inspiration. They occur in association with conditions that cause fluid to accumulate within the alveolar and interstitial spaces, such as heart failure or pneumonia. Fine crackles are soft, high-pitched, and very brief. For this reason, it is essential to listen to lung sounds with the stethoscope placed on the patient's skin and not over their clothing or hospital gown. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling-type noises produced during expiration (and sometimes inspiration) when air is forced through airways narrowed by bronchoconstriction or associated mucosal edema. For example, patients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with mechanical obstruction at the level of the trachea/upper airway.
- Pleural rub may be heard on either inspiration or expiration and sounds like the rubbing together of leather. A pleural rub is heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other.[174]
Life Span Considerations
Children
There are various respiratory assessment considerations that should be noted with assessment of children.
- The respiratory rate in children less than 12 months of age can range from 30-60 breaths per minute, depending on whether the infant is asleep or active.
- Infants have irregular or periodic newborn breathing in the first few weeks of life; therefore, it is important to count the respirations for a full minute. During this time, you may notice periods of apnea lasting up to 10 seconds. This is not abnormal unless the infant is showing other signs of distress. Signs of respiratory distress in infants and children include nasal flaring and sternal or intercostal retractions.
- Up to three months of age, infants are considered “obligate” nose-breathers, meaning their breathing is primarily through the nose.
- The anteroposterior-transverse ratio is typically 1:1 until the thoracic muscles are fully developed around six years of age.
Older Adults
As the adult person ages, the cartilage and muscle support of the thorax becomes weakened and less flexible, resulting in a decrease in chest expansion. Older adults may also have weakened respiratory muscles, and breathing may become shallower. The anteroposterior-transverse ratio may be 1:1 if there is significant curvature of the spine (kyphosis).
Percussion
Percussion is an advanced respiratory assessment technique that is used by advanced practice nurses and other health care providers to gather additional data in the underlying lung tissue. By striking the fingers of one hand over the fingers of the other hand, a sound is produced over the lung fields that helps determine if fluid is present. Dull sounds are heard with high-density areas, such as pneumonia or atelectasis, whereas clear, low-pitched, hollow sounds are heard in normal lung tissue.
![]()
- Because infants breathe primarily through the nose, nasal congestion can limit the amount of air getting into the lungs.
- Attempt to assess an infant’s respiratory rate while the infant is at rest and content rather than when the infant is crying. Counting respirations by observing abdominal breathing movements may be easier for the novice nurse than counting breath sounds, as it can be difficult to differentiate lung and heart sounds when auscultating newborns.
- Auscultation of lungs during crying is not a problem. It will enhance breath sounds.
- The older patient may have a weakening of muscles that support respiration and breathing. Therefore, the patient may report tiring easily during the assessment when taking deep breaths. Break up the assessment by listening to the anterior lung sounds and then the heart sounds and allowing the patient to rest before listening to the posterior lung sounds.
- Patients with end-stage COPD may have diminished lung sounds due to decreased air movement. This abnormal assessment finding may be the patient’s baseline or normal and might also include wheezes and fine crackles as a result of chronic excess secretions and/or bronchoconstriction.[175],[176]
Expected Versus Unexpected Findings
See Table 10.3b for a comparison of expected versus unexpected findings when assessing the respiratory system.[177]
Table 10.3b Expected Versus Unexpected Respiratory Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if a new finding*) |
|---|---|---|
| Inspection | Work of breathing effortless
Regular breathing pattern Respiratory rate within normal range for age Chest expansion symmetrical Absence of cyanosis or pallor Absence of accessory muscle use, retractions, and/or nasal flaring Anteroposterior: transverse diameter ratio 1:2 |
Labored breathing
Irregular rhythm Increased or decreased respiratory rate Accessory muscle use, pursed-lip breathing, nasal flaring (infants), and/or retractions Presence of cyanosis or pallor Asymmetrical chest expansion Clubbing of fingernails |
| Palpation | No pain or tenderness with palpation. Skin warm and dry; no crepitus or masses | Pain or tenderness with palpation, crepitus, palpable masses, or lumps |
| Percussion | Clear, low-pitched, hollow sound in normal lung tissue | Dull sounds heard with high-density areas, such as pneumonia or atelectasis |
| Auscultation | Bronchovesicular and vesicular sounds heard over appropriate areas
Absence of adventitious lung sounds |
Diminished lung sounds
Adventitious lung sounds, such as fine crackles/rales, wheezing, stridor, or pleural rub |
| *CRITICAL CONDITIONS to report immediately | Decreased oxygen saturation <92%[178]
Pain Worsening dyspnea Decreased level of consciousness, restlessness, anxiousness, and/or irritability |
Low-pitched, loud, continuous sounds frequently heard on expiration.
With an understanding of the basic structures and primary functions of the respiratory system, the nurse collects subjective and objective data to perform a focused respiratory assessment.
Subjective Assessment
Collect data using interview questions, paying particular attention to what the patient is reporting. The interview should include questions regarding any current and past history of respiratory health conditions or illnesses, medications, and reported symptoms. Consider the patient’s age, gender, family history, race, culture, environmental factors, and current health practices when gathering subjective data. The information discovered during the interview process guides the physical exam and subsequent patient education. See Table 10.3a for sample interview questions to use during a focused respiratory assessment.[179]
Table 10.3a Interview Questions for Subjective Assessment of the Respiratory System
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a respiratory condition, such as asthma, COPD, pneumonia, or allergies?
Do you use oxygen or peak flow meter? Do you use home respiratory equipment like CPAP, BiPAP, or nebulizer devices? |
Please describe the conditions and treatments. |
| Are you currently taking any medications, herbs, or supplements for respiratory concerns? | Please identify what you are taking and the purpose of each. |
| Have you had any feelings of breathlessness
(dyspnea)? |
Note: If the shortness of breath is severe or associated with chest pain, discontinue the interview and obtain emergency assistance.
Are you having any shortness of breath now? If yes, please rate the shortness of breath from 0-10 with "0" being none and "10" being severe? Does anything bring on the shortness of breath (such as activity, animals, food, or dust)? If activity causes the shortness of breath, how much exertion is required to bring on the shortness of breath? When did the shortness of breath start? Is the shortness of breath associated with chest pain or discomfort? How long does the shortness of breath last? What makes the shortness of breath go away? Is the shortness of breath related to a position, like lying down? Do you sleep in a recliner or upright in bed? Do you wake up at night feeling short of breath? How many pillows do you sleep on? How does the shortness of breath affect your daily activities? |
| Do you have a cough? | When you cough, do you bring up anything? What color is the phlegm?
Do you cough up any blood (hemoptysis)? Do you have any associated symptoms with the cough such as fever, chills, or night sweats? How long have you had the cough? Does anything bring on the cough (such as activity, dust, animals, or change in position)? What have you used to treat the cough? Has it been effective? |
| Do you smoke or vape? | What products do you smoke/vape? If cigarettes are smoked, how many packs a day do you smoke?
How long have you smoked/vaped? Have you ever tried to quit smoking/vaping? What strategies gave you the best success? Are you interested in quitting smoking/vaping? If the patient is ready to quit, the five successful interventions are the "5 A's": Ask, Advise, Assess, Assist, and Arrange. Ask - Identify and document smoking status for every patient at every visit. Advise - In a clear, strong, and personalized manner, urge every user to quit. Assess - Is the user willing to make a quitting attempt at this time? Assist - For the patient willing to make a quitting attempt, use counseling and pharmacotherapy to help them quit. Arrange - Schedule follow-up contact, in person or by telephone, preferably within the first week after the quit date.[180] |
Life Span Considerations
Depending on the age and capability of the child, subjective data may also need to be retrieved from a parent and/or legal guardian.
Pediatric
- Is your child up-to-date with recommended immunizations?
- Is your child experiencing any cold symptoms (such as runny nose, cough, or nasal congestion)?
- How is your child’s appetite? Is there any decrease or change recently in appetite or wet diapers?
- Does your child have any hospitalization history related to respiratory illness?
- Did your child have any history of frequent ear infections as an infant?
Older Adult
- Have you noticed a change in your breathing?
- Do you get short of breath with activities that you did not before?
- Can you describe your energy level? Is there any change from previous?
Objective Assessment
A focused respiratory objective assessment includes interpretation of vital signs; inspection of the patient’s breathing pattern, skin color, and respiratory status; palpation to identify abnormalities; and auscultation of lung sounds using a stethoscope. For more information regarding interpreting vital signs, see the “General Survey” chapter. The nurse must have an understanding of what is expected for the patient’s age, gender, development, race, culture, environmental factors, and current health condition to determine the meaning of the data that is being collected.
Evaluate Vital Signs
The vital signs may be taken by the nurse or delegated to unlicensed assistive personnel such as a nursing assistant or medical assistant. Evaluate the respiratory rate and pulse oximetry readings to verify the patient is stable before proceeding with the physical exam. The normal range of a respiratory rate for an adult is 12-20 breaths per minute at rest, and the normal range for oxygen saturation of the blood is 94–98% (SpO₂).[181] Bradypnea is less than 12 breaths per minute, and tachypnea is greater than 20 breaths per minute.
Inspection
Inspection during a focused respiratory assessment includes observation of level of consciousness, breathing rate, pattern and effort, skin color, chest configuration, and symmetry of expansion.
- Assess the level of consciousness. The patient should be alert and cooperative. Hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide) can cause a decreased level of consciousness, irritability, anxiousness, restlessness, or confusion.
- Obtain the respiratory rate over a full minute. The normal range for the respiratory rate of an adult is 12-20 breaths per minute.
- Observe the breathing pattern, including the rhythm, effort, and use of accessory muscles. Breathing effort should be nonlabored and in a regular rhythm. Observe the depth of respiration and note if the respiration is shallow or deep. Pursed-lip breathing, nasal flaring, audible breathing, intercostal retractions, anxiety, and use of accessory muscles are signs of respiratory difficulty. Inspiration should last half as long as expiration unless the patient is active, in which case the inspiration-expiration ratio increases to 1:1.
- Observe the pattern of expiration and patient position. Patients who experience difficulty expelling air, such as those with emphysema, may have prolonged expiration cycles. Some patients may experience difficulty with breathing specifically when lying down. This symptom is known as orthopnea. Additionally, patients who are experiencing significant breathing difficulty may experience most relief while in a “tripod” position. This can be achieved by having the patient sit at the side of the bed with legs dangling toward the floor. The patient can then rest their arms on an overbed table to allow for maximum lung expansion. This position mimics the same position you might take at the end of running a race when you lean over and place your hands on your knees to “catch your breath.”
- Observe the patient’s color in their lips, face, hands, and feet. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctivae, or inner aspect of the lower lip. Cyanosis is a bluish discoloration of the skin, lips, and nail beds, which may indicate decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes and usually the result of reduced blood flow, oxygenation, or decreased number of red blood cells.
- Inspect the chest for symmetry and configuration. The trachea should be midline, and the clavicles should be symmetrical. See Figure 10.2[182] for visual landmarks when inspecting the thorax anteriorly, posteriorly, and laterally. Note the location of the ribs, sternum, clavicle, and scapula, as well as the underlying lobes of the lungs.
- Chest movement should be symmetrical on inspiration and expiration.
- Observe the anterior-posterior diameter of the patient’s chest and compare to the transverse diameter. The expected anteroposterior-transverse ratio should be 1:2. A patient with a 1:1 ratio is described as barrel-chested. This ratio is often seen in patients with chronic obstructive pulmonary disease due to hyperinflation of the lungs. See Figure 10.3[183] for an image of a patient with a barrel chest.
- Older patients may have changes in their anatomy, such as kyphosis, an outward curvature of the spine.
- Inspect the fingers for clubbing if the patient has a history of chronic respiratory disease. Clubbing is a bulbous enlargement of the tips of the fingers due to chronic hypoxia. See Figure 10.4[184] for an image of clubbing.
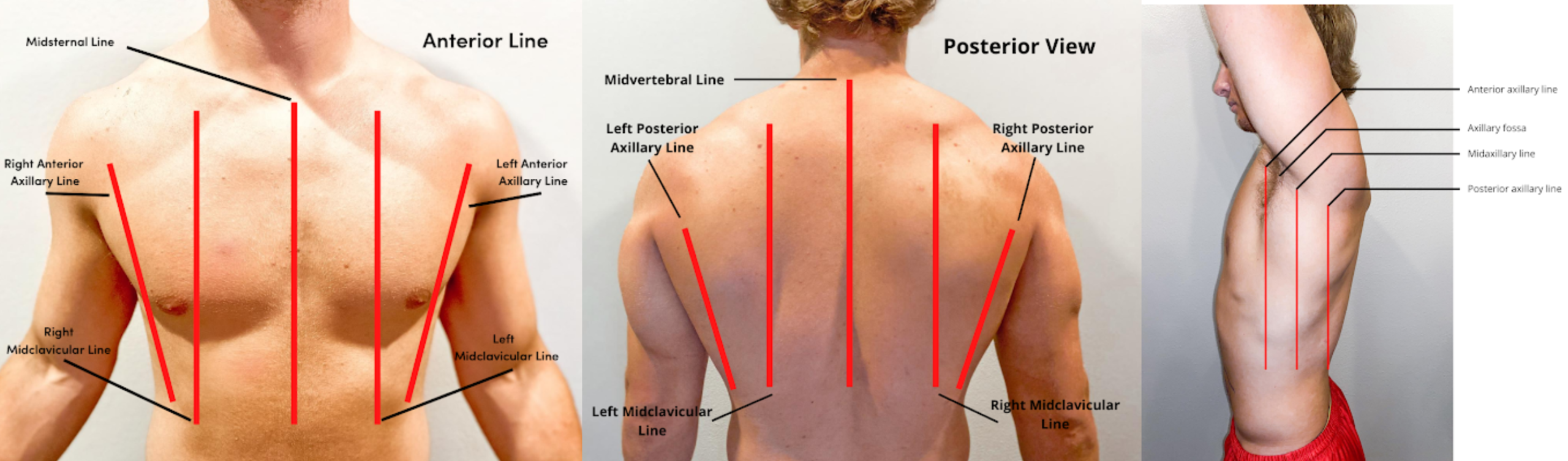


Palpation
- Palpation of the chest may be performed to investigate for areas of abnormality related to injury or procedural complications. For example, if a patient has a chest tube or has recently had one removed, the nurse may palpate near the tube insertion site to assess for areas of air leak or crepitus. Crepitus feels like a popping or crackling sensation when the skin is palpated and is a sign of air trapped under the subcutaneous tissues. If palpating the chest, use light pressure with the fingertips to examine the anterior and posterior chest wall. Chest palpation may be performed to assess specifically for growths, masses, crepitus, pain, or tenderness.
- Confirm symmetric chest expansion by placing your hands on the anterior or posterior chest at the same level, with thumbs over the sternum anteriorly or the spine posteriorly. As the patient inhales, your thumbs should move apart symmetrically. Unequal expansion can occur with pneumonia, thoracic trauma, such as fractured ribs, or pneumothorax.
Auscultation
Using the diaphragm of the stethoscope, listen to the movement of air through the airways during inspiration and expiration. Instruct the patient to take deep breaths through their mouth. Listen through the entire respiratory cycle because different sounds may be heard on inspiration and expiration. Allow the patient to rest between respiratory cycles, if needed, to avoid fatigue with deep breathing during auscultation. As you move across the different lung fields, the sounds produced by airflow vary depending on the area you are auscultating because the size of the airways change.
Correct placement of the stethoscope during auscultation of lung sounds is important to obtain a quality assessment. The stethoscope should not be placed over clothes or hair because these may create inaccurate sounds from friction. The best position to listen to lung sounds is with the patient sitting upright; however, if the patient is acutely ill or unable to sit upright, turn them side to side in a lying position. Avoid listening over bones, such as the scapulae or clavicles or over the female breasts to ensure you are hearing adequate sound transmission. Listen to sounds from side to side rather than down one side and then down the other side. This side-to-side pattern allows you to compare sounds in symmetrical lung fields. See Figures 10.5[185] and 10.6[186] for landmarks of stethoscope placement over the anterior and posterior chest wall.
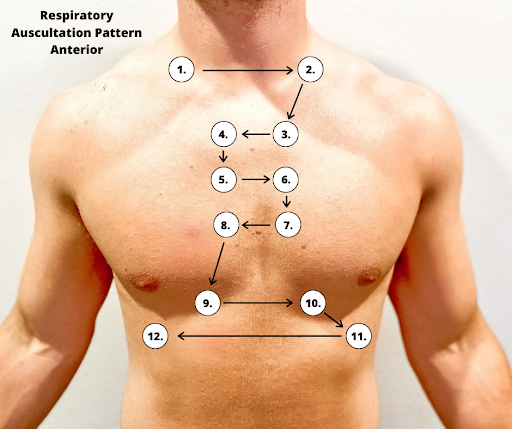
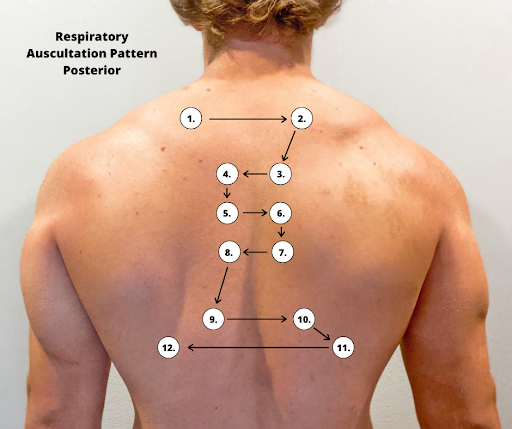
Expected Breath Sounds
It is important upon auscultation to have awareness of expected breath sounds in various anatomical locations.
- Bronchial breath sounds are heard over the trachea and larynx and are high-pitched and loud.
- Bronchovesicular sounds are medium-pitched and heard over the major bronchi.
- Vesicular breath sounds are heard over the lung surfaces, are lower-pitched, and often described as soft, rustling sounds.
Adventitious Lung Sounds
Adventitious lung sounds are sounds heard in addition to normal breath sounds. They most often indicate an airway problem or disease, such as accumulation of mucus or fluids in the airways, obstruction, inflammation, or infection. These sounds include rales/crackles, rhonchi/wheezes, stridor, and pleural rub:
- Coarse crackles, also called rhonchi, are low-pitched, loud, continuous sounds frequently heard on expiration. They are a sign of turbulent airflow through secretions in the large airways.
Rhonchi Lung Sounds on YouTube [187]
- Fine crackles, also called rales, are popping or crackling sounds heard on inspiration. They occur in association with conditions that cause fluid to accumulate within the alveolar and interstitial spaces, such as heart failure or pneumonia. Fine crackles are soft, high-pitched, and very brief. For this reason, it is essential to listen to lung sounds with the stethoscope placed on the patient's skin and not over their clothing or hospital gown. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling-type noises produced during expiration (and sometimes inspiration) when air is forced through airways narrowed by bronchoconstriction or associated mucosal edema. For example, patients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with mechanical obstruction at the level of the trachea/upper airway.
- Pleural rub may be heard on either inspiration or expiration and sounds like the rubbing together of leather. A pleural rub is heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other.[188]
Life Span Considerations
Children
There are various respiratory assessment considerations that should be noted with assessment of children.
- The respiratory rate in children less than 12 months of age can range from 30-60 breaths per minute, depending on whether the infant is asleep or active.
- Infants have irregular or periodic newborn breathing in the first few weeks of life; therefore, it is important to count the respirations for a full minute. During this time, you may notice periods of apnea lasting up to 10 seconds. This is not abnormal unless the infant is showing other signs of distress. Signs of respiratory distress in infants and children include nasal flaring and sternal or intercostal retractions.
- Up to three months of age, infants are considered “obligate” nose-breathers, meaning their breathing is primarily through the nose.
- The anteroposterior-transverse ratio is typically 1:1 until the thoracic muscles are fully developed around six years of age.
Older Adults
As the adult person ages, the cartilage and muscle support of the thorax becomes weakened and less flexible, resulting in a decrease in chest expansion. Older adults may also have weakened respiratory muscles, and breathing may become shallower. The anteroposterior-transverse ratio may be 1:1 if there is significant curvature of the spine (kyphosis).
Percussion
Percussion is an advanced respiratory assessment technique that is used by advanced practice nurses and other health care providers to gather additional data in the underlying lung tissue. By striking the fingers of one hand over the fingers of the other hand, a sound is produced over the lung fields that helps determine if fluid is present. Dull sounds are heard with high-density areas, such as pneumonia or atelectasis, whereas clear, low-pitched, hollow sounds are heard in normal lung tissue.
![]()
- Because infants breathe primarily through the nose, nasal congestion can limit the amount of air getting into the lungs.
- Attempt to assess an infant’s respiratory rate while the infant is at rest and content rather than when the infant is crying. Counting respirations by observing abdominal breathing movements may be easier for the novice nurse than counting breath sounds, as it can be difficult to differentiate lung and heart sounds when auscultating newborns.
- Auscultation of lungs during crying is not a problem. It will enhance breath sounds.
- The older patient may have a weakening of muscles that support respiration and breathing. Therefore, the patient may report tiring easily during the assessment when taking deep breaths. Break up the assessment by listening to the anterior lung sounds and then the heart sounds and allowing the patient to rest before listening to the posterior lung sounds.
- Patients with end-stage COPD may have diminished lung sounds due to decreased air movement. This abnormal assessment finding may be the patient’s baseline or normal and might also include wheezes and fine crackles as a result of chronic excess secretions and/or bronchoconstriction.[189],[190]
Expected Versus Unexpected Findings
See Table 10.3b for a comparison of expected versus unexpected findings when assessing the respiratory system.[191]
Table 10.3b Expected Versus Unexpected Respiratory Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if a new finding*) |
|---|---|---|
| Inspection | Work of breathing effortless
Regular breathing pattern Respiratory rate within normal range for age Chest expansion symmetrical Absence of cyanosis or pallor Absence of accessory muscle use, retractions, and/or nasal flaring Anteroposterior: transverse diameter ratio 1:2 |
Labored breathing
Irregular rhythm Increased or decreased respiratory rate Accessory muscle use, pursed-lip breathing, nasal flaring (infants), and/or retractions Presence of cyanosis or pallor Asymmetrical chest expansion Clubbing of fingernails |
| Palpation | No pain or tenderness with palpation. Skin warm and dry; no crepitus or masses | Pain or tenderness with palpation, crepitus, palpable masses, or lumps |
| Percussion | Clear, low-pitched, hollow sound in normal lung tissue | Dull sounds heard with high-density areas, such as pneumonia or atelectasis |
| Auscultation | Bronchovesicular and vesicular sounds heard over appropriate areas
Absence of adventitious lung sounds |
Diminished lung sounds
Adventitious lung sounds, such as fine crackles/rales, wheezing, stridor, or pleural rub |
| *CRITICAL CONDITIONS to report immediately | Decreased oxygen saturation <92%[192]
Pain Worsening dyspnea Decreased level of consciousness, restlessness, anxiousness, and/or irritability |
The gastrointestinal (GI) system is responsible for the ingestion of food and the absorption of nutrients. Additionally, the GI and genitourinary (GU) systems are responsible for the elimination of waste products.[193] Therefore, during assessment of these systems, the nurse collects subjective and objective data regarding the underlying structures of the abdomen, as well as the normal functioning of the GI and GU systems.
Subjective Assessment
A focused gastrointestinal and genitourinary subjective assessment collects data about the signs and symptoms of GI and GU diseases, including any digestive or nutritional issues, relevant medical or family history of GI and GU diseases, and any current treatment for related issues.[194] Table 12.3a outlines interview questions used to explore medical and surgical history, symptoms related to the gastrointestinal and genitourinary systems, and associated medications. Information gained from the interview process is used to tailor the subsequent physical assessment and create a plan for patient care and education.[195]
Table 12.3a Interview Questions for Subjective Assessment of GI and GU Systems
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a gastrointestinal (GI), kidney, or bladder condition? |
Please describe the conditions and treatments. |
| Have you ever had abdominal surgery? | Please describe the surgery and if you experienced any complications. |
| Are you currently taking any medications, herbs, or supplements? | Please describe. |
| Do you have any abdominal pain? | Are there any associated symptoms with the pain such as fever, nausea, vomiting, or change in bowel pattern?
Are you having bloody stools (hematochezia); dark, tarry stools (melena); abdominal distention; or vomiting of blood (hematemesis)? When did the pain start to occur? (Onset) Where is the pain? (Location) When it occurs, how long does the pain last? (Duration) Can you describe what the pain feels like? (Characteristics) What brings on the pain? (Aggravating factors) What relieves the pain? (Alleviating factors) Does the pain radiate anywhere? (Radiation) What have you used to treat the pain? (Treatment) What effect has the pain had on you? (Effects) How severe is the pain from 0-10 when it occurs? (Severity) |
| Have you had any issues with nausea, vomiting, food intolerance, heartburn, ulcers, change in appetite, or weight? | Please describe.
What treatment did you use for these symptoms? What is your typical diet in a 24-hour period? |
| Do you have any difficulty swallowing food or liquids (dysphagia)? | Please describe.
Have you ever been diagnosed with a stroke or transient ischemic attack (TIA)? |
| When was your last bowel movement? | Have there been any changes in pattern or consistency of your stool?
Are you passing any gas? |
| Have you had any issues with constipation or diarrhea? | Please describe.
How long have you had these issues? What treatment did you use for these symptoms? If constipation:
If diarrhea:
|
| Do you experience any pain or discomfort with urination (dysuria)? | Please describe.
If you have discomfort while urinating, is the discomfort internal or external? Do you use any treatment for these symptoms? |
| Do you experience frequent urination (urinary frequency)? | Please describe.
Does the frequency occur during daytime or nighttime hours? |
| Do you ever experience a strong urge to urinate that makes it difficult to reach the bathroom in time (urinary urgency)? | Does this strong urge ever result in a leakage of urine? Does the urge come and go or is it continuous? |
| Do you have any leakage of urine when you cough, sneeze, or jump (urinary incontinence)?
Do you have difficulty starting the flow of urine? |
Have you tried any treatment for this issue? |
Gastrointestinal
Pain is the most common complaint related to abdominal problems and can be attributed to multiple underlying etiologies. Because of the potential variability of contributing factors, a careful and thorough assessment of this chief complaint should occur. Additional associated questions include asking if bloody stools (hematochezia); dark, tarry stools ( melena); bloating (abdominal distention); or vomiting of blood (hematemesis) are occurring.
Nausea, vomiting, diarrhea, and constipation are common issues experienced by hospitalized patients due to adverse effects of medications or medical procedures. Read more details about commonly occurring gastrointestinal conditions in the "Elimination" chapter in Open RN Nursing Fundamentals. It is important to ask a hospitalized patient daily about the date of their last bowel movement and flatus so that a bowel management program can be initiated if necessary. If a patient is experiencing diarrhea, it is important to assess and monitor for signs of dehydration or electrolyte imbalances. Dehydration can be indicated by dry skin, dry mucous membranes, or sunken eyes. These symptoms may require contacting the health care provider for further treatment. Read additional information about fluid and electrolyte imbalances in the "Fluids and Electrolytes" chapter in Open RN Nursing Fundamentals.
Additional specialized assessments of GI system function can include examination of the oropharynx and esophagus. For example, patients who have experienced a cerebrovascular accident (CVA), also called a “stroke,” may experience difficulty swallowing (dysphagia). The nurse is often the first to notice these difficulties in patients who are swallowing pills, liquid, or food and can advocate for treatment to prevent complications, such as unintended weight loss or aspiration pneumonia.[196]
Genitourinary
The nursing assessment of the genitourinary system generally focuses on bladder function. Ask about urinary symptoms, including dysuria, urinary frequency, or urinary urgency. Dysuria is any discomfort associated with urination and often signifies a urinary tract infection. Patients with dysuria commonly experience burning, stinging, or itching sensation. In elderly patients, changes in mental status may be the presenting symptom of a urinary tract infection. In women with dysuria, asking whether the discomfort is internal or external is important because vaginal inflammation can also cause dysuria as urine passes by the inflamed labia.
Abnormally frequent urination (e.g., every hour or two) is termed urinary frequency. In older adults, urinary frequency often occurs at night and is termed nocturia. Frequency of normal urination varies considerably from individual to individual depending on personality traits, bladder capacity, or drinking habits. It can also be a symptom of a urinary tract infection, pregnancy in females, or prostate enlargement in males.
Urinary urgency is an abrupt, strong, and often overwhelming need to urinate. Urgency often causes urinary incontinence, a leakage of urine. When patients experience urinary urgency, the desire to urinate may be constant with only a few milliliters of urine eliminated with each voiding.[197] Read additional information about commonly occurring genitourinary system alterations in the "Elimination" chapter in Open RN Nursing Fundamentals.
Life Span Considerations
Infants
Eating and elimination patterns of infants require special consideration based on the stage of development.
- Ask parents about feeding habits. Is the baby being breastfed or formula fed? If formula fed, how does the child tolerate the formula?
- To assess for urine output in infants and toddlers, assess the frequency of wet diapers and the daily number of wet diapers. In hospitalized infants and toddlers, the diapers may be weighed for precise measurements of urine output.
- Note that the expected abdominal contour of an infant is called protuberant, which means bulging.
- Assess the umbilical cord; it should dry and fall off on its own within two weeks of life.
- Observe for respiratory movement in the abdomen of the infant.
Children
The expected abdominal contour of a child is protuberant until about the age of 4. Children often cannot provide more information than “my stomach hurts”; they may have symptoms of decreased school attendance due to abdominal discomfort.
Older Adults
Constipation may be more common in older adults due to decreased physical mobility and oral intake. Urinary urgency, urinary frequency, urinary retention, nocturia, and urinary incontinence are also common concerns for older adults. A common medical condition in males as they age is prostate hypertrophy (i.e., enlargement of the prostate gland), causing uncomfortable urinary symptoms such as urgency and frequency.
Objective Assessment
Physical examination of the abdomen includes inspection, auscultation, palpation, and percussion. Note that the order of physical assessment differs for the abdominal system compared to other systems. Palpation should occur after the auscultation of bowel sounds so that accurate, undisturbed bowel sounds can be assessed. The abdomen is roughly divided into four quadrants: right upper, right lower, left upper, and left lower (see Figure 12.3[198]). When assessing the abdomen, consider the organs located in the quadrant you are examining.
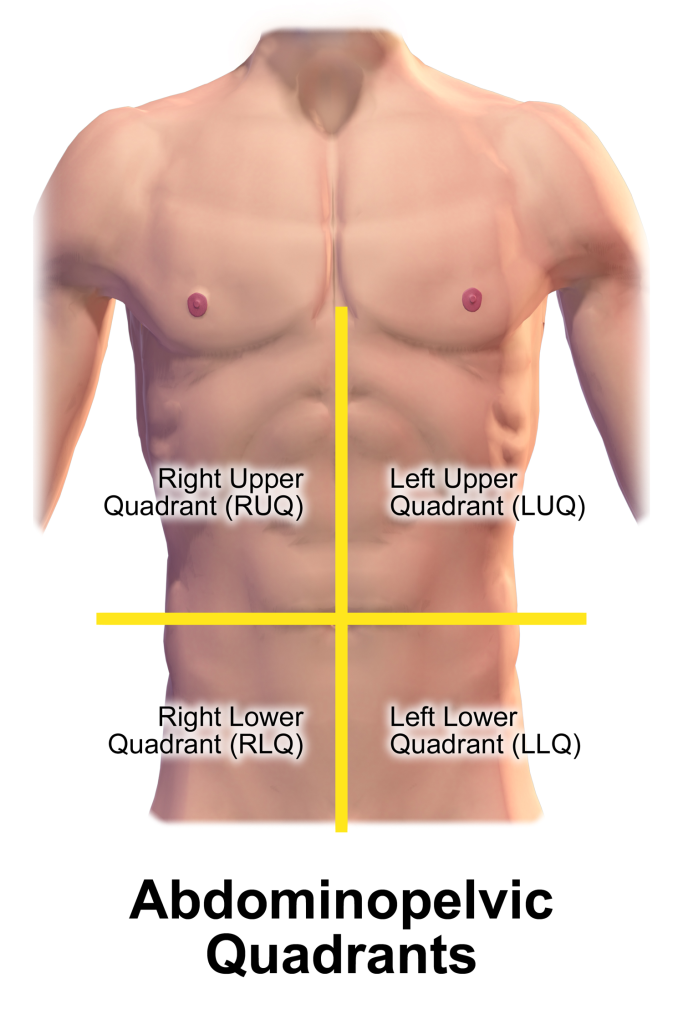
In preparation for the physical assessment, the nurse should create an environment in which the patient will be comfortable. Encourage the patient to empty their bladder prior to the assessment. Warm the room and stethoscope to decrease tensing during assessment.
Inspection
The abdomen is inspected by positioning the patient supine on an examining table or bed. The head and knees should be supported with small pillows or folded sheets for comfort and to relax the abdominal wall musculature. The patient's arms should be at their side and not folded behind the head, as this tenses the abdominal wall. Ensure the patient is covered adequately to maintain privacy, while still exposing the abdomen as needed for a thorough assessment. Visually examine the abdomen for overall shape, masses, skin abnormalities, and any abnormal movements.
- Observe the general contour and symmetry of the entire abdominal wall. The contour of the abdomen is often described as flat, rounded, scaphoid (sunken), or protuberant (convex or bulging).
- Assess for distention. Generalized distention of the abdomen can be caused by obesity, bowel distention from gas or liquid, or fluid buildup.
- Assess for masses or bulges, which may indicate structural deformities like hernias or related to disorders in abdominal organs.
- Assess the patient’s skin for uniformity of color, integrity, scarring, or striae. Striae are white or silvery elongated marks that occur when the skin stretches, especially during pregnancy or excessive weight gain.
- Note the shape of the umbilicus; it should be inverted and midline.
- Carefully note any scars and correlate these scars with the patient's recollection of previous surgeries or injury.
- Document any abnormal movement or pulsations. Visible intestinal peristalsis can be caused by intestinal obstruction. Pulsations may be seen in the epigastric area in patients who are especially thin, but otherwise should not be observed.[199],[200]
Auscultation
Auscultation, or the listening of the abdomen, follows inspection for more accurate assessment of bowel sounds. Use a warmed stethoscope to assess the frequency and characteristics of the patient’s bowel sounds, which are also referred to as peristaltic murmurs.
Begin your assessment by gently placing the diaphragm of your stethoscope on the skin in the right lower quadrant (RLQ), as bowel sounds are consistently heard in that area. Bowel sounds are generally high-pitched, gurgling sounds that are heard irregularly. Move your stethoscope to the next quadrant in a clockwise motion around the abdominal wall.
It is not recommended to count abdominal sounds because the activity of normal bowel sounds may cycle with peak-to-peak periods as long as 50 to 60 minutes.[201] The majority of peristaltic murmurs are produced by the stomach, with the remainder from the large intestine and a small contribution from the small intestine. Because the conduction of peristaltic murmur is heard throughout all parts of the abdomen, the source of peristaltic murmur is not always at the site where it is heard. If the conduction of peristaltic sounds is good, auscultation at a single location is considered adequate. [202]
Hyperactive bowel sounds may indicate bowel obstruction or gastroenteritis. Sometimes you may be able to hear a patient’s bowel sounds without a stethoscope, often described as “stomach growling” or borborygmus. This is a common example of hyperactive sounds. Hypoactive bowel sounds may be present with constipation, after abdominal surgery, peritonitis, or paralytic ileus. As you auscultate the abdomen, you should not hear vascular sounds. If heard, this finding should be reported to the health care provider.[203],[204]
Palpation
Palpation, or touching, of the abdomen involves using the flat of the hand and fingers (not the fingertips) to detect palpable organs, abnormal masses, or tenderness[205] (see Figure 12.4 [206]). When palpating the abdomen of a patient reporting abdominal pain, the nurse should palpate that area last. Light palpation is primarily used by bedside nurses to assess for musculature, abnormal masses, and tenderness. Deep palpation is a technique used by advanced practice clinicians to assess for enlarged organs. Lightly palpate the abdomen by pressing into the skin about 1 centimeter beginning in the RLQ. Continue to move around the abdomen in a clockwise manner.
Palpate the bladder for distention. Palpate gently from umbilicus down toward the pelvis feeling for a full bladder. The bladder is not normally palpable, but a distended bladder may reach the umbilicus. A full bladder presents as a pelvis mass, which is typically regular, smooth, firm, and oval-shaped. It arises in the midline. Note the patient response to palpation, such as pain, guarding, rigidity, or rebound tenderness. Voluntary guarding refers to voluntary contraction of the abdominal wall musculature, usually the result of fear, anxiety, or the touch of cold hands. Involuntary guarding is the reflexive contraction of overlying abdominal muscules as the result of peritoneal inflammation. Rigidity refers to involuntary contraction of the abdominal musculature in response to peritoneal inflammation, a reflex the patient cannot control.[207] Rebound tenderness is another sign of peritoneal inflammation or peritonitis. To elicit rebound tenderness, the clinician maintains pressure over an area of tenderness and then withdraws the hand abruptly. If the patient winces with pain upon withdrawal of the hand, the test is positive.[208],[209], [210]
Note: If the patient has a Foley catheter in place, additional assessments are included in the “Facilitation of Elimination” chapter.

Percussion
You may observe advanced practice nurses and other health care providers percussing the abdomen to obtain additional data. Percussing can be used to assess the liver and spleen or to determine if costovertebral angle (CVA) tenderness is present, which is related to inflammation of the kidney.
![]()
- Encourage the patient to empty their bladder prior to palpation.
- When palpating the abdomen, ask the patient to bend their knees when lying in a supine position to enhance relaxation of abdominal muscles.
See Table 12.3b for a comparison of expected versus unexpected findings when assessing the abdomen.
Table 12.3b Expected Versus Unexpected Gastrointestinal and Genitourinary Assessment Findings
| Assessment | Expected Findings |
Unexpected Findings (Document and notify the provider of any new findings*) |
|---|---|---|
| Inspection | Symmetry of shape and color
Flat or rounded contour (protuberant in children until age 4) No visible lesions Intact skin
|
Asymmetry
Distension Scars Wounds Skin breakdown Pulsations Visible peristalsis |
| Auscultation | Presence of normoactive bowel sounds | Hypoactive bowel sounds
Hyperactive bowel sounds Absent bowel sounds |
| Palpation | Absence of pain or tenderness
Absence of masses Voluntary guarding |
Pain on palpation
Involuntary guarding Rigidity Rebound tenderness Masses noted that are not previously documented |
| Genitourinary | Clear, pale yellow urine
Absence of pain, urgency, frequency, or retention Nondistended bladder |
Dark or bloody urine, foul odor, or sediment present
Dysuria Urinary frequency Urinary urgency Urinary retention, indicated by distended bladder and/or tenderness on palpation |
| *CRITICAL CONDITIONS to report immediately | New or worsening melena
Bloody stools Hematemesis Signs of dehydration associated with diarrhea and vomiting, such as <30mL urine/hour |
The reflexive contraction of overlying abdominal muscules as the result of peritoneal inflammation.
Skeleton
The skeleton is composed of 206 bones that provide the internal supporting structure of the body. See Figure 13.1[211] for an illustration of the major bones in the body. The bones of the lower limbs are adapted for weight-bearing support, stability, and walking. The upper limbs are highly mobile with large range of movements, along with the ability to easily manipulate objects with our hands and opposable thumbs.[212]
For additional information about the bones in the body, visit the OpenStax Anatomy and Physiology book.
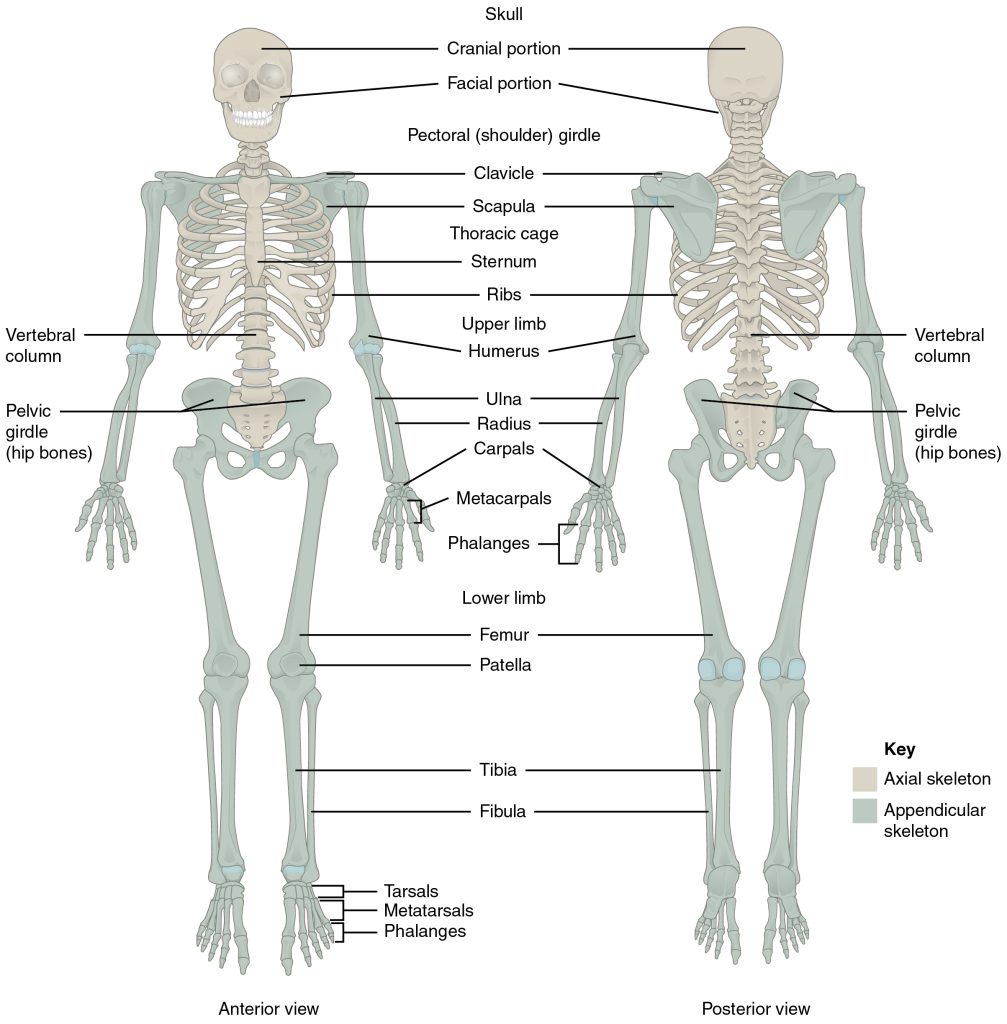
Many different bones are connected together by ligaments. Most bones of the skill are held together by sutures, a narrow fibrous joint. Ligaments are strong bands of fibrous connective tissue that strengthen and support the joint by anchoring the bones together and preventing their separation. Ligaments allow for normal movements of a joint while also limiting the range of these motions to prevent excessive or abnormal joint movements.[213]
Muscles
There are three types of muscle tissue: skeletal muscle, cardiac muscle, and smooth muscle. Skeletal muscles are attached to the skeleton and produce movement, assist in maintaining posture, protect internal organs, and generate body heat. Skeletal muscles are voluntary, meaning a person is able to consciously control them, but they also depend on signals from the nervous system to work properly. Other types of muscles are involuntary and are controlled by the autonomic nervous system, such as the smooth muscle within our bronchioles.[214] Cardiac muscles are located only in the heart and are involuntary muscles that the autonomic nervous system controls. Smooth muscle makes up the organs, blood vessels, digestive tract, skin, and other areas and is controlled by the autonomic nervous system.
See Figure 13.2[215] for an illustration of skeletal muscle.
To move the skeleton, the tension created by the contraction of the skeletal muscles is transferred to the tendons, strong bands of dense, regular connective tissue that connect muscles to bones.[216]
For additional information about skeletal muscles, visit the OpenStax Anatomy and Physiology book.
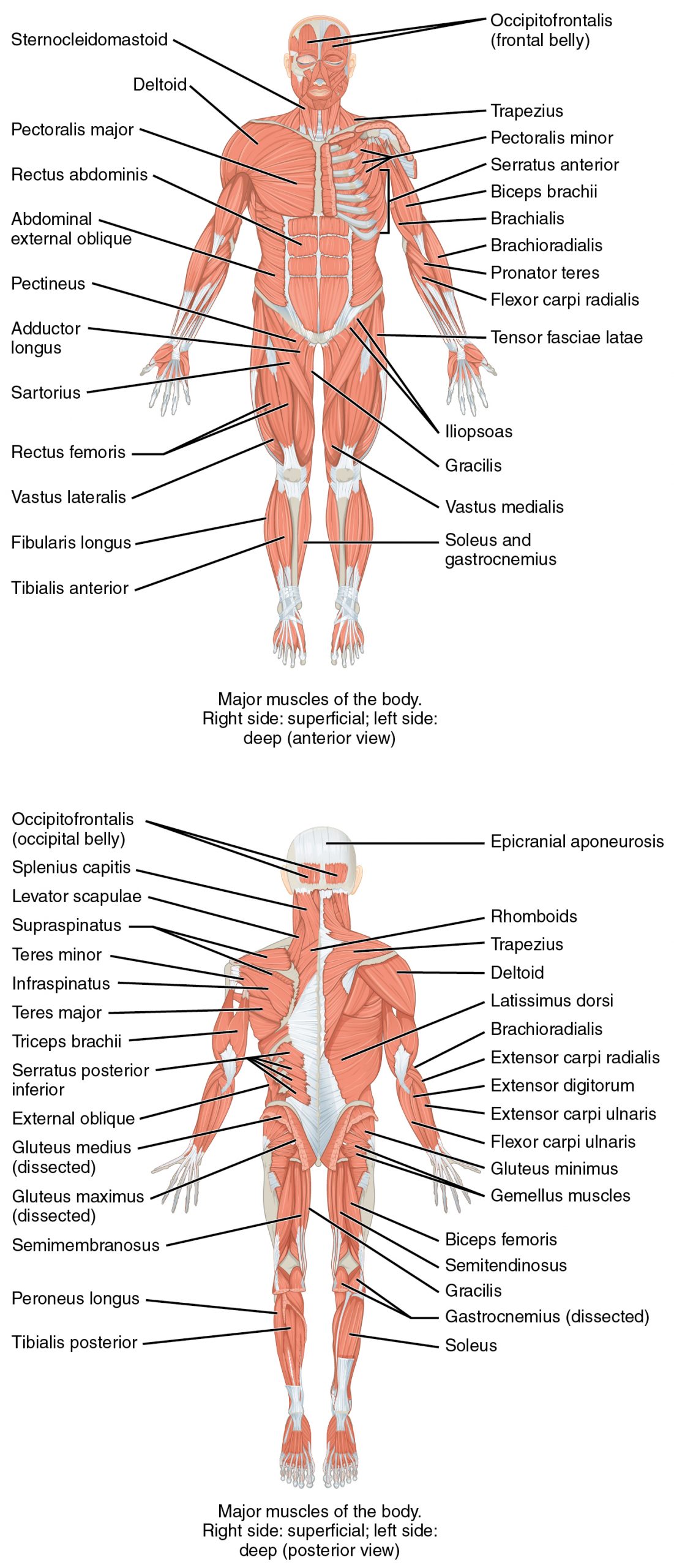
Muscle Atrophy
Muscle atrophy is the thinning or loss of muscle tissue. See Figure 13.3[217] for an image of muscle atrophy. There are three types of muscle atrophy: physiologic, pathologic, and neurogenic.
Physiologic atrophy is caused by not using the muscles and can often be reversed with exercise and improved nutrition. People who are most affected by physiologic atrophy are those who:
- Have seated jobs, health problems that limit movement, or decreased activity levels
- Are bedridden
- Cannot move their limbs because of stroke or other brain disease
- Are in a place that lacks gravity, such as during space flights
Pathologic atrophy is seen with aging, starvation, and adverse effects of long-term use of corticosteroids. Neurogenic atrophy is the most severe type of muscle atrophy. It can be from an injured or diseased nerve that connects to the muscle. Examples of neurogenic atrophy are spinal cord injuries and polio.[218]
Although physiologic atrophy due to disuse can often be reversed with exercise, muscle atrophy caused by age is more complex. The effects of age-related atrophy are especially pronounced in people who are sedentary because the loss of muscle results in functional impairments such as trouble with walking, balance, and posture. These functional impairments can cause decreased quality of life and injuries due to falls.[219]
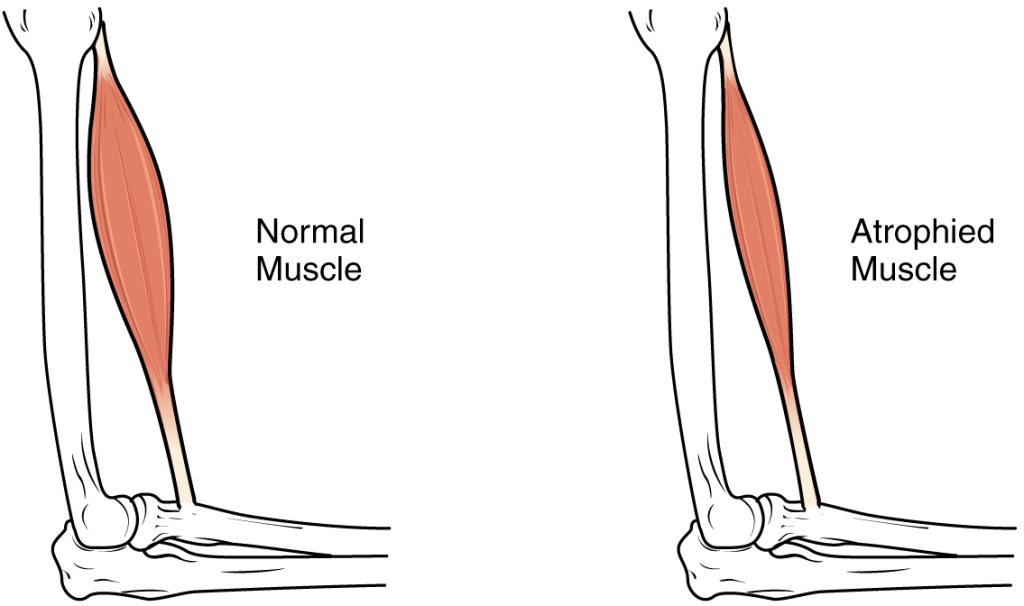
Joints
Joints are the location where bones come together. Many joints allow for movement between the bones. Synovial joints are the most common type of joint in the body. Synovial joints have a fluid-filled joint cavity where the articulating surfaces of the bones contact and move smoothly against each other. See Figure 13.4[220] for an illustration of a synovial joint. Articular cartilage is smooth, white tissue that covers the ends of bones where they come together and allows the bones to glide over each other with very little friction. Articular cartilage can be damaged by injury or normal wear and tear. Lining the inner surface of the articular capsule is a thin synovial membrane. The cells of this membrane secrete synovial fluid, a thick, slimy fluid that provides lubrication to further reduce friction between the bones of the joint.[221]
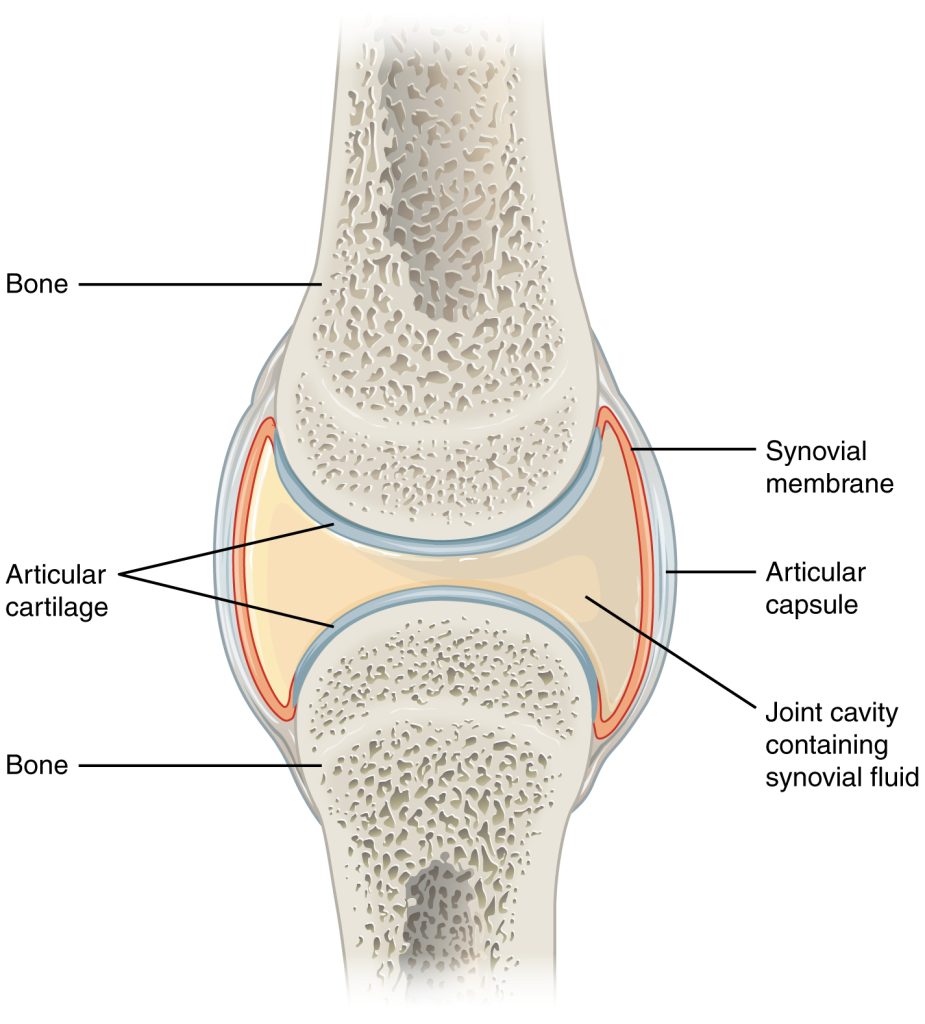
Types of Synovial Joints
There are six types of synovial joints. See Figure 13.5[222] for an illustration of the types of synovial joints. Some joints are relatively immobile but stable. Other joints have more freedom of movement but are at greater risk of injury. For example, the hinge joint of the knee allows flexion and extension, whereas the ball and socket joint of the hip and shoulder allows flexion, extension, abduction, adduction, and rotation. The knee, hip, and shoulder joints are commonly injured and are discussed in more detail in the following subsections.
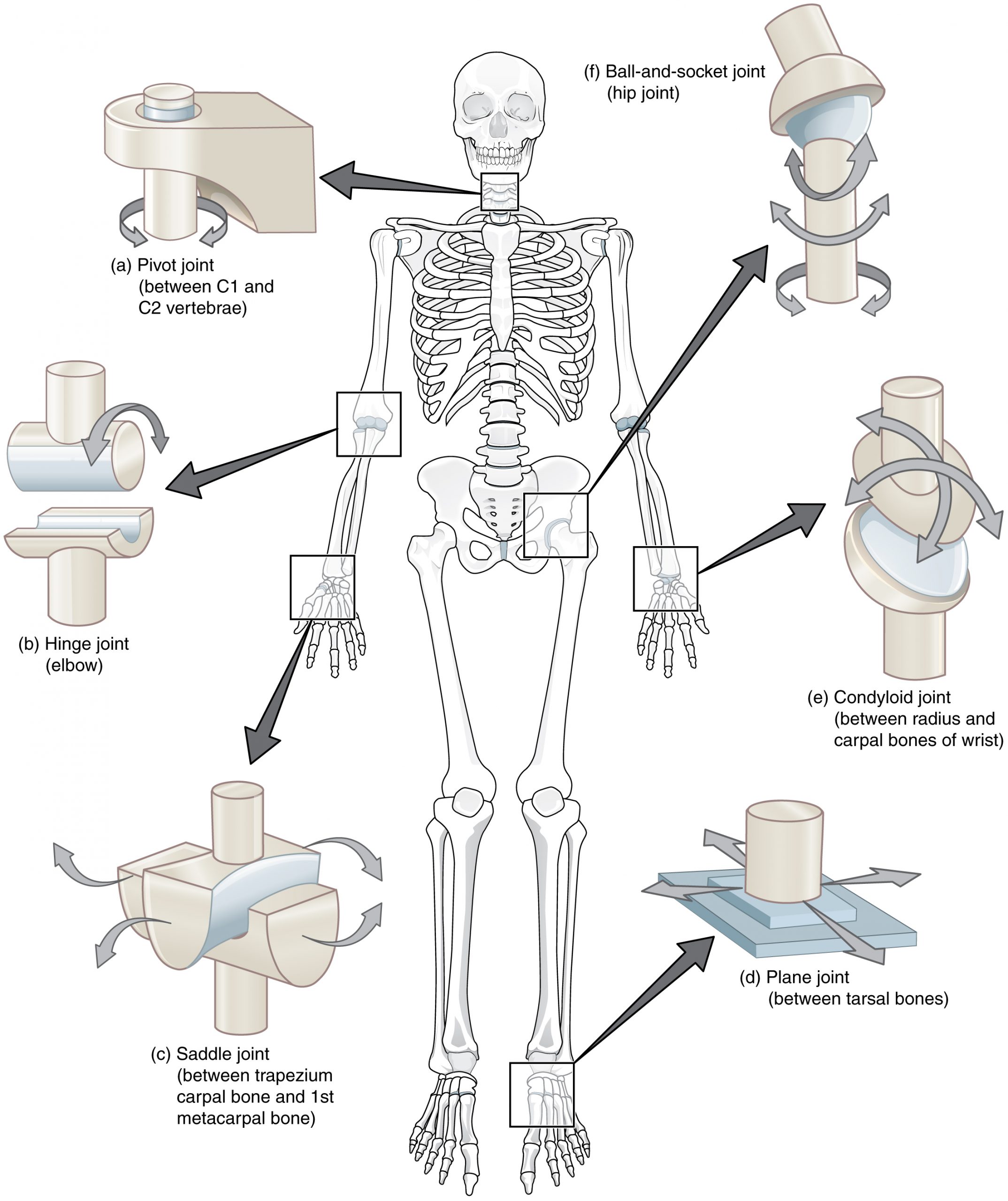
Shoulder Joint
The shoulder joint is a ball-and-socket joint formed by the articulation between the head of the humerus and the glenoid cavity of the scapula. This joint has the largest range of motion of any joint in the body. See Figure 13.6[223] to review the anatomy of the shoulder joint. Injuries to the shoulder joint are common, especially during repetitive abductive use of the upper limb such as during throwing, swimming, or racquet sports.[224]
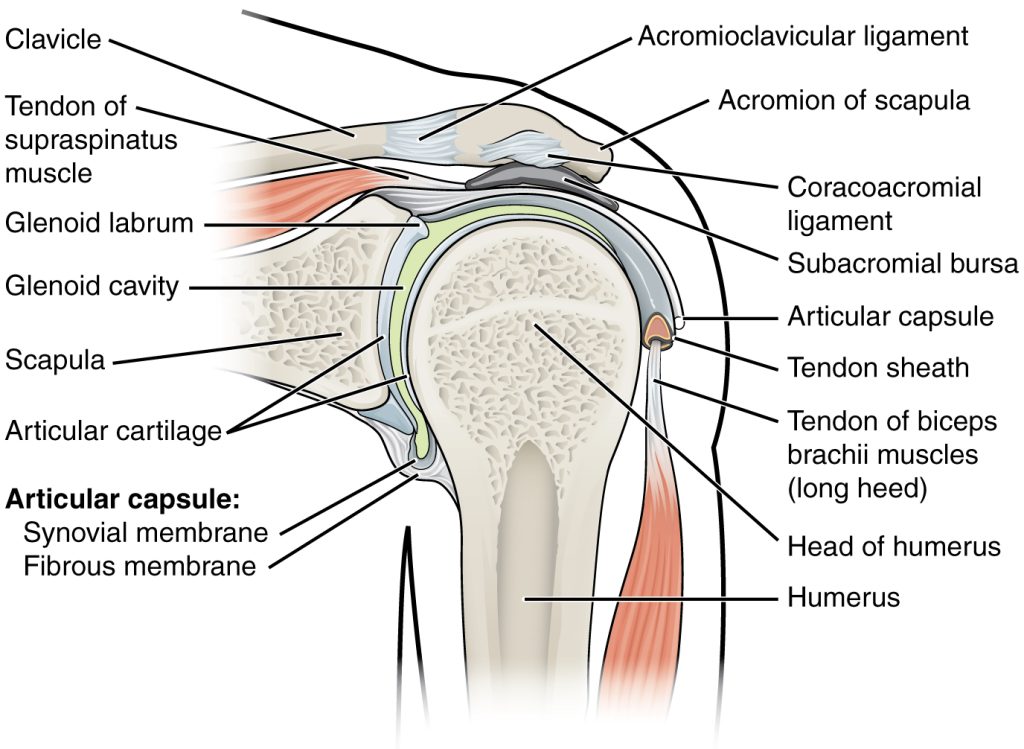
Hip Joint
The hip joint is a ball-and-socket joint between the head of the femur and the acetabulum of the hip bone. The hip carries the weight of the body and thus requires strength and stability during standing and walking.[225]
See Figure 13.7[226] for an illustration of the hip joint.
A common hip injury in older adults, often referred to as a “broken hip,” is actually a fracture of the head of the femur. Hip fractures are commonly caused by falls.[227]
See more information about hip fractures under the “Common Musculoskeletal Conditions” section.
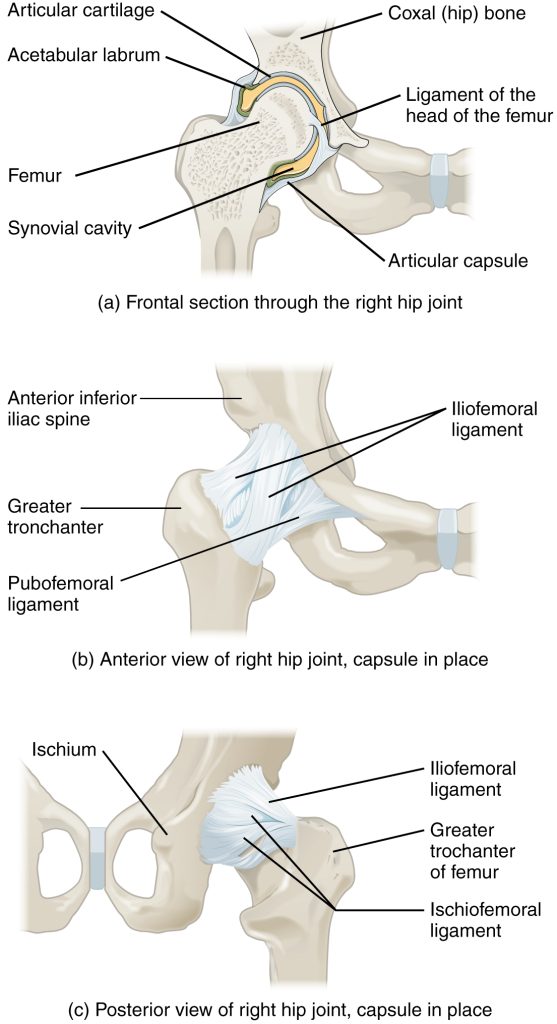
Knee Joint
The knee functions as a hinge joint that allows flexion and extension of the leg. In addition, some rotation of the leg is available. See Figure 13.8[228] for an illustration of the knee joint. The knee is vulnerable to injuries associated with hyperextension, twisting, or blows to the medial or lateral side of the joint, particularly while weight-bearing.[229]
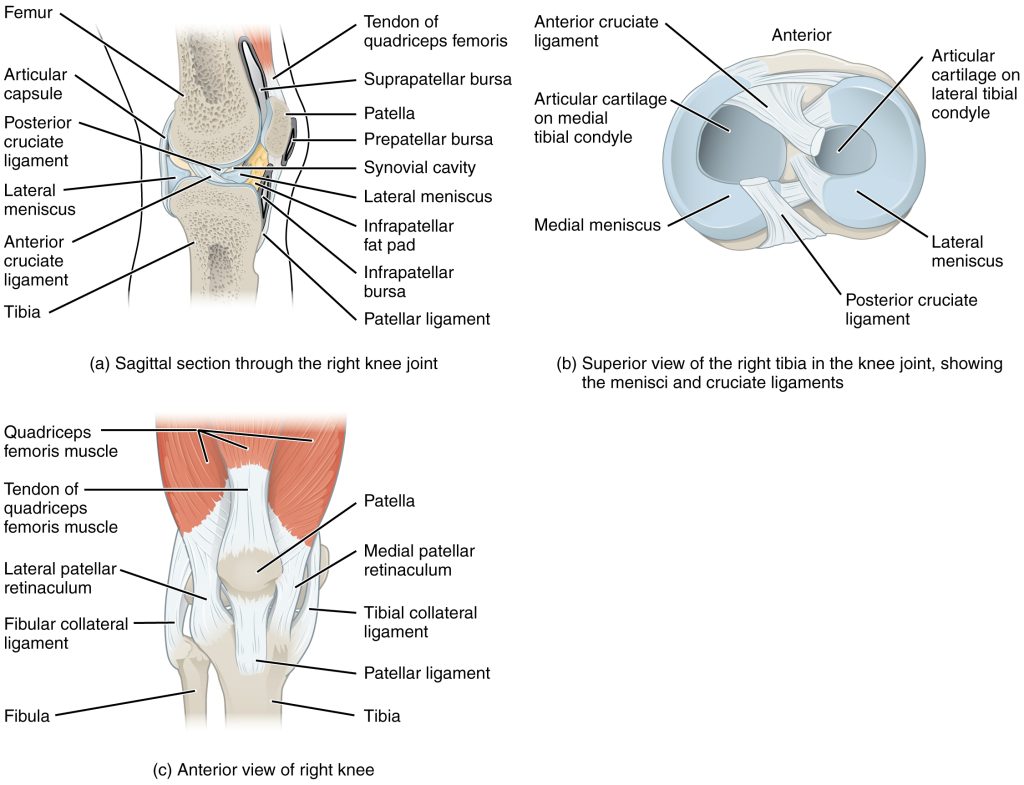
The knee joint has multiple ligaments that provide support, especially in the extended position. On the outside of the knee joint are the lateral collateral, medial collateral, and tibial collateral ligaments. The lateral collateral ligament is on the lateral side of the knee and spans from the lateral side of the femur to the head of the fibula. The medial collateral ligament runs from the medial side of the femur to the medial tibia. The tibial collateral ligament crosses the knee and is attached to the articular capsule and to the medial meniscus. In the fully extended knee position, both collateral ligaments are taut and stabilize the knee by preventing side-to-side or rotational motions between the femur and tibia.[230]
Inside the knee joint are the anterior cruciate ligament and posterior cruciate ligament. These ligaments are anchored inferiorly to the tibia and run diagonally upward to attach to the inner aspect of a femoral condyle. The posterior cruciate ligament supports the knee when it is flexed and weight-bearing such as when walking downhill. The anterior cruciate ligament becomes tight when the knee is extended and resists hyperextension.[231]
The patella is a bone incorporated into the tendon of the quadriceps muscle, the large muscle of the anterior thigh. The patella protects the quadriceps tendon from friction against the distal femur. Continuing from the patella to the anterior tibia just below the knee is the patellar ligament. Acting via the patella and patellar ligament, the quadriceps is a powerful muscle that extends the leg at the knee and provides support and stabilization for the knee joint.
Located between the articulating surfaces of the femur and tibia are two articular discs, the medial meniscus and lateral meniscus. Each meniscus is a C-shaped fibrocartilage that provides padding between the bones.[232]
Joint Movements
Several movements may be performed by synovial joints. Abduction is the movement away from the midline of the body. Adduction is the movement toward the middle line of the body. Extension is the straightening of limbs (increase in angle) at a joint. Flexion is bending the limbs (reduction of angle) at a joint. Rotation is a circular movement around a fixed point. See Figures 13.9[233] and 13.10[234] for images of the types of movements of different joints in the body.
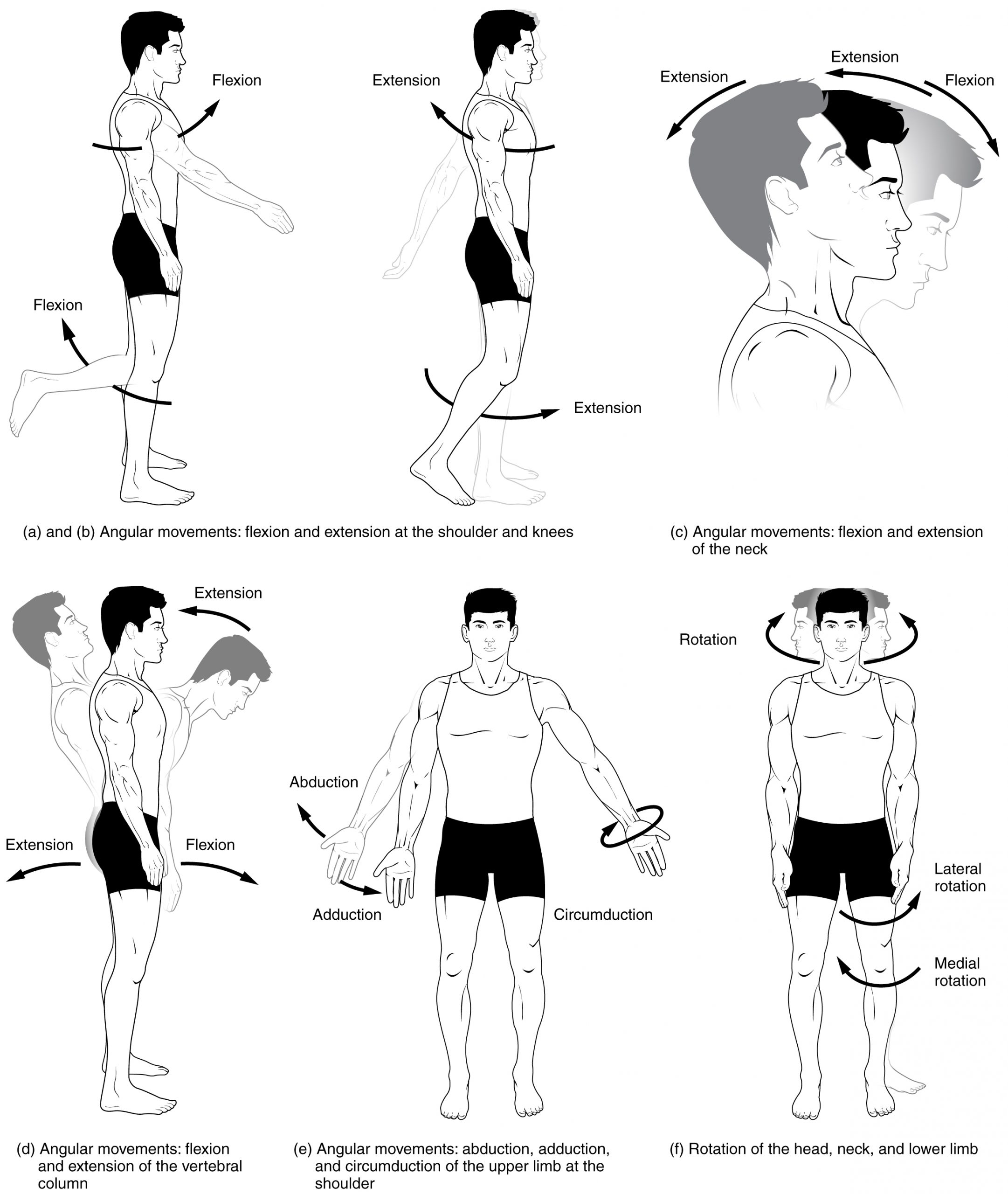
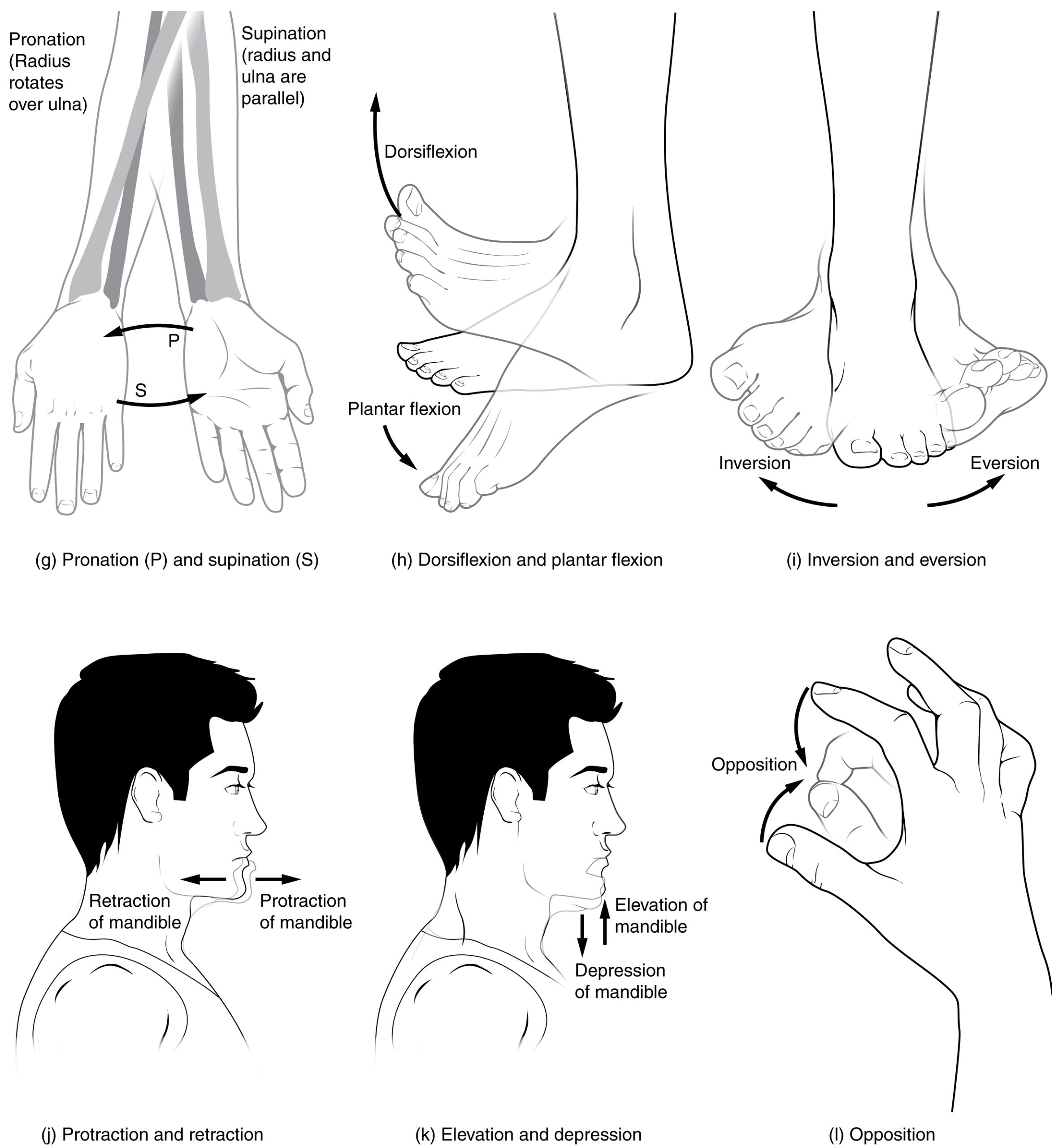
Joint Sounds
Sounds that occur as joints are moving are often referred to as crepitus. There are many different types of sounds that can occur as a joint moves, and patients may describe these sounds as popping, snapping, catching, clicking, crunching, cracking, crackling, creaking, grinding, grating, and clunking. There are several potential causes of these noises such as bursting of tiny bubbles in the synovial fluid, snapping of ligaments, or a disease condition. While assessing joints, be aware that joint noises are common during activity and are usually painless and harmless, but if they are associated with an injury or are accompanied by pain or swelling, they should be reported to the health care provider for follow-up.[235]
View a supplementary video from Physitutors called Why Your Knees Crack | Joint Crepitations.[236]
Voluntary muscle that produces movement, assists in maintaining posture, protects internal organs, and generates body heat.
The thinning or loss of muscle tissue that can be caused by disuse, aging, or neurological damage.
The location where bones come together.
A fluid-filled joint cavity where the articulating surfaces of the bones contact and move smoothly against each other. The elbow and knee are examples of synovial joints.
Smooth, white tissue that covers the ends of bones where they come together at joints, allowing them to glide over each other with very little friction. Articular cartilage can be damaged by injury or normal wear and tear.
A thick fluid that provides lubrication in joints to reduce friction between the bones.
Joint movement away from the midline of the body.
Joint movement toward the middle line of the body.
Joint movement causing the straightening of limbs (increase in angle) at a joint.
Collection of blood.
Angiogenesis: The development of new capillaries in a wound base.
Arterial ulcers: Ulcers caused by lack of blood flow and oxygenation to tissues and typically occur in the distal areas of the body such as the feet, heels, and toes.
Debridement: The removal of nonviable tissue in a wound.
Dehiscence: The separation of the edges of a surgical wound.
Diabetic ulcers: Ulcers that typically develop on the plantar aspect of the feet and toes of patients with diabetes due to lack of sensation of pressure or injury.
Ecchymosis: Bruising that occurs when small veins and capillaries under the skin break.
Edema: Swelling.
Epithelialization: The development of new epidermis and granulation tissue.
Erythema: Redness.
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in a wound base that must be removed for healing to occur.
Exudate: Fluid that oozes out of a wound; also commonly called pus.
Granulation tissue: New connective tissue in a wound base with fragile, thin-walled capillaries that must be protected.
Hematoma: An area of blood that collects outside of larger blood vessels.
Hemosiderin staining: Dark-colored discoloration of the lower legs due to blood pooling.
Hemostasis phase: The first phase of wound healing that occurs immediately after skin injury. Blood vessels constrict and clotting factors are activated.
Induration: Area of hardened tissue.
Inflammatory phase: The second phase of wound healing when vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed.
Maceration: The softening and wasting away of skin due to excess fluid.
Maturation phase: The final phase of wound healing as collagen continues to be created to strengthen the wound, causing scar tissue.
Necrotic: Black tissue color due to tissue death from lack of oxygenation to the area.
Nonblanchable erythema: Skin redness that does not turn white when pressure is applied.
Osteomyelitis: Bone infection.
Peripheral neuropathy: A condition that causes decreased sensation of pain and pressure, typically in the lower extremities.
Periwound: The skin around the outer edges of a wound.
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.[237]
Primary intention: Wound healing that occurs with surgical incisions or clean-edged lacerations that are closed with sutures, staples, or surgical glue.
Proliferative phase: The third phase of wound healing that includes epithelialization, angiogenesis, collagen formation, and contraction.
Purulent drainage: Wound exudate that is thick and opaque and can be tan, yellow, green, or brown in color. It is never considered normal in a wound, and new purulent drainage should always be reported to the health care provider.
Sanguineous drainage: Wound drainage that is fresh bleeding.
Secondary intention: Wound healing that occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries.
Serosanguinous drainage: Wound exudate contains serous drainage with small amounts of blood present.
Serous drainage: Wound drainage that is clear, thin, watery plasma. It is considered normal in minimal amounts during the inflammatory stage of wound healing.
Shear: A mechanical force that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Skin tears: Wounds caused by mechanical forces, typically in the nonelastic skin of older adults.
Slough: Inflammatory exudate that is light yellow, soft, and moist and must be removed for wound healing to occur.
Tertiary intention: Wound healing that occurs when a wound must remain open or has been reopened, often due to severe infection.
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns.
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge.
Unstageable: Occurs when slough or eschar obscures the wound so that tissue loss cannot be assessed.
Venous insufficiency: A medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs that can cause venous ulcers.
Venous ulcers: Ulcers caused by the pooling of fluid in the veins of the lower legs when the valves are not working properly, causing fluid to seep out, macerate the skin, and cause an ulcer.
Wound vac: A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing.
Circular movement of a joint around a fixed point.
