10.4 Current Issues: Transcarceration
Brandon Hamann and Kate McLean
Transcarceration or “Reinstitutionalization”
One prominent social justice campaign of the mid-twentieth century that is less remembered today is the anti-psychiatry movement. This movement questioned the science behind psychiatry, the evidence underlying different mental health diagnoses, and the function of psychiatry as an effective form of social control (sometimes leveraged against political dissidents around the world.) Among other goals, the movement sought to reduce the use of involuntary commitment, particularly within state-run hospitals, where “treatment” was sometimes indistinguishable from incarceration. (An important, if disturbing, documentary from 1967, The Titicut Follies, reveals in gruesome detail how patients at the Bridgewater State Hospital in Massachusetts were dehumanized by staff.) Deinstitutionalization of individuals with no income, and no other caretakers, may have remained an impossible target, were it not for the advent of the first powerful neurotropic drugs in the 1950s, most notably thorazine – an antipsychotic used to treat schizophrenia.
The Community Mental Health Act (CMHA) of 1963 was the last piece of legislation signed by John F. Kennedy Jr. before his assassination less than one month later. The law sought to provide funding for a vast network of outpatient mental health centers “in the community,” thus allowing for the release of thousands of inpatients from state psychiatric hospitals. Unfortunately, while the latter institutions began rapidly shedding patients – and closing – in the years that followed, over half of the promised community centers never materialized. In turn, many individuals with severe mental illness found themselves precariously housed, homeless, and then sometimes incarcerated. Having few choices of where to go, many individuals with severe mental illness became destitute and/or destitute. Ultimately, some wound up in America’s jails and prisons, after committing offenses to support themselves, violating anti-homeless ordinances, or acting in ways deemed violent or dangerous by law enforcement. This phenomenon is referred to as “Transcarceration” or “Transinstitutionalization,” as individuals simply moved from one facility of involuntary confinement to another. At the dawn of the 1960s, the rate of confinement within state psychiatric hospitals was over 800 individuals per 100,000 population, while the incarceration rate was barely over 200 per 100,000; by the new millennium, these rates had flipped, with the population in prisons and jails exceeding 800 per 10,000 populations, and the rate of psychiatric hospital less than 500 per 100,000. (These trajectories are reflected in some stunning charts produced by the scholar Bernard Harcourt in the article Reducing Mass Incarceration: Lessons from the Deinstitutionalization of Mental Hospitals in the 1960s.)
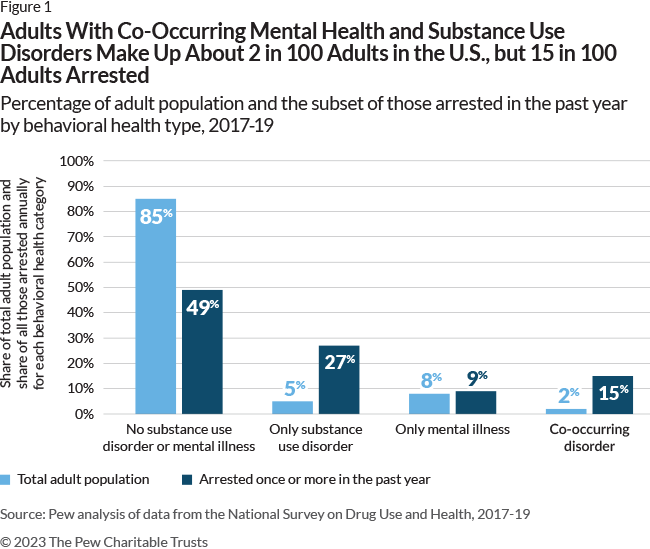
Today, many might argue that – whatever the deficiencies of state psychiatric hospitals – prisons and jails are more traumatizing institutions that are ill-equipped to treat complicated mental illnesses. It may surprise and shock many to learn that the largest “mental health providers” in the United States are, in order, the Los Angeles County Jail, the Cook County Jail (Chicago), and Rikers Island Jail in New York City, a reality that has had tragic consequences for both mentally-ill inmates as well as those without a diagnosis. Yet, as detailed by Alisa Roth in her 2018 book Insane: America’s Criminal Treatment of Mental Illness, America’s jails are among the few institutions filling in disastrous gaps in outpatient mental health care nationwide. Now, nearly 60 years after President Kennedy signed the CMHA, the question of how to treat homeless individuals with severe mental illness remains pressing and unresolved. Unfortunately, many cities continue to seek ways to arrest and incarcerate such individuals on a larger scale rather than address their underlying diagnoses and risk factors.
Mental Health in Louisiana
There is a stark difference in the science from the 1960s and today regarding mental health and the criminal justice system. Medical science has made significant developments in the diagnoses and treatments of mental health issues in people from every walks of life. However, the criminal justice system as a whole has been unable to keep up with the science in legislating comprehensive relief treatments that are equitable in dealing with individuals who display a need for alternative measures because they are mentally disabled, having either been previously diagnosed or in need of specialized care from an undiagnosed condition. Likewise, research has shown that in some instances, institutionalization of offenders can lead to the development of mental health concerns from lack of adequate care within jails and prisons.
Louisiana ranks 30th nationally, according to one study in mental health well-being, with 23.01% of respondents reporting that they have a mental illness, and 5.72% having a serious mental illness (Masterson & Metz, 2023). Another study found that 1 in 4 Louisianans with a serious mental health illness have been arrested within their lifetime. It is estimated that 40% of the current prison population in Louisiana could have a mental illness, and 7 in 10 incarcerated youth have a mental illness (NAMI, 2023).
To find out more on state rankings for mental health and the NAMI fact sheet, click the links below.
In the News: A Return to Involuntary Commitment?
In November 2022, New York City Mayor Eric Adams directed police and EMS personnel to remove homeless individuals who exhibit “unawareness or delusional misapprehension of surroundings” or “delusional misapprehension of physical condition or health” from the streets, for potential hospitalization against their will. Importantly, the directive did not require police to determine that such individuals were violent, or a threat to the public safety.
How effective do you think this new policy will be in: Reducing homelessness? Addressing crimes committed by and against individuals with mental illness? Improving access to mental health treatment?
Then, compare that to the findings: What the Data Shows about Mayor Adams’ Involuntary Removal Policy.
the transfer of prisoners or persons institutionalized for mental illness from one facility to another of the same type.

