Chapter 3: Genetics, Prenatal Development, and Birth

Learning Objectives:
Upon completion of this chapter, you will be able to:
- Examine our essential genetic endowment and explain how human development can go awry
- Explain how the environment and genetics work together to determine human characteristics
- Determine which human characteristics are significantly affected by heredity
- Determine which human characteristics are significantly affected by the environment
- Recognize and express the prenatal stages of development
- Name the threats to the fetal environment and articulate what can be done about them
Louisiana Snapshot
The United States has the highest maternal mortality rate of any industrialized country. It is worse than it was 20 years ago. Maternal death is defined by the World Health Organization as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.” The maternal death rate has increased in the U.S. for several years. Women in the U.S. are ten or more times more likely to die from pregnancy-related causes than mothers in Poland, Spain, or Norway. Some of the worst mortality rates come out of the South, with Louisiana leading the U.S., where poverty, inadequate healthcare, and racial discrimination have historically put women and their babies at greater risk, as seen in this report from “60 Minutes,” on CBS News, 2023. This increase has significantly impacted minority women. According to the Centers for Disease Control and Prevention (Hoyert, 2020), in 2020, 861 women died of maternal causes in the United States, compared to 754 in 2019. The maternal mortality rate for 2020 was 23.8 deaths per 100,000 live births compared with a rate of 20.1 in 2019 (Figure 3.1). In 2020, the maternal mortality rate for non-Hispanic Black women was 55.3 deaths per 100,000 live births, 2.9 times the rate for non-Hispanic White women. The increases from 2019 to 2020 for non-Hispanic Black and Hispanic women were significant.
Research consistently shows that the maternal mortality rate index is influenced by social and economic factors such as limited access to health services, health literacy status, lack of access to quality emergency obstetric and delivery care, and household income (Shahin, Hardwick, Jeffery, Jordan, & Mase, 2020). Complications during pregnancy and childbirth are also other factors that increase MMR.
Racism is rarely explored through research as a cause for the disparity in maternal mortality rates. The term “miscommunication” (Shahin, Hardwick, Jeffery, Jordan, & Mase, 2020) has been used to explain why African American women feel unheard and receive erroneous diagnoses of health issues during pregnancy. However, according to Professor Jacelyn Johnson with American University, there are many anecdotal accounts of African American women from all social classes experiencing disrespect, procedures without consent, rough handling, and dismissiveness toward pain from doctors at all phases of their maternal journey. Tori Bowie, an Olympic athlete; Kira Johnson, whose husband was told that his wife was “not a priority right now;” Dr. Chaniece Wallace; and Shalon Irving are among the many African American women whose deaths were related to childbirth. Serena Williams and Laura Coates are among the women who successfully fought to be heard and get the care they needed. Multiple factors contribute to these disparities, such as variation in quality healthcare, underlying chronic conditions, structural racism, and implicit bias (CDC, Office of Health Equity, 2023).
Before moving on, think about what you have read here. Why does the United States have such high maternal mortality rates compared to other industrialized nations? Why does this issue worsen in one of the best nations for healthcare? While the unique challenges of African American mothers are highlighted here, this is an issue for all American mothers, regardless of income and education. What practices can we incorporate to turn this around?
This course takes a holistic approach to human development, emphasizing that it starts at conception and goes on till death. This chapter delves into some fundamental concepts related to birth and heredity. We look at how fetal development is diverse and cumulative, shaped by the genetic material that both biological parents provide. We also explore how evolution generally progresses and what causes congenital abnormalities. However, before we delve into these topics, we must stress the significance of the relationship between heredity and the environment. This chapter aids in comprehending the importance of parental health during conception and pregnancy, the benefits of social support and reduced stress to a developing fetus, and why we are who we are. As you reflect on some of your traits, such as height, weight, personality, or diabetes, ask yourself if these traits are due to heredity or environmental factors. You will most likely realize that both heredity and environmental factors such as lifestyle, diet, and others have shaped these traits.
Genetics
How Does Genetics Influence Development?
There are two types of sex cells or gametes involved in reproduction: the male gametes or sperm and the female gametes or ovum. The male gametes are produced in the testes in spermatogenesis, which begins at about 12 years of age. The female gametes or ova stored in the ovaries are present at birth but are immature. Each ovary contains about 250,000 (Rome, 1998), but only about 400 will become mature eggs (Mackon and Fauser, 2000). Beginning at puberty, one ovum ripens and is released about every 28 days, a process called oogenesis.
After the ovum or egg ripens and is released from the ovary, it is drawn into the fallopian tube and reaches the uterus in 3 to 4 days. When fertilized, the egg is typically fertilized in the fallopian tube and continues its journey to the uterus. At ejaculation, millions of sperm are released into the vagina, but only a few reach the egg, and typically, only one sperm fertilizes the one egg. Once a single sperm has entered the egg’s wall, the wall becomes hard and prevents other sperm from entering. The tail of the sperm that is inside the egg breaks off, and the head of the sperm, containing the genetic information from the father, unites with the nucleus of the egg. As a result, a new cell is formed. This cell, including the combined genetic information from both parents, is called a zygote.
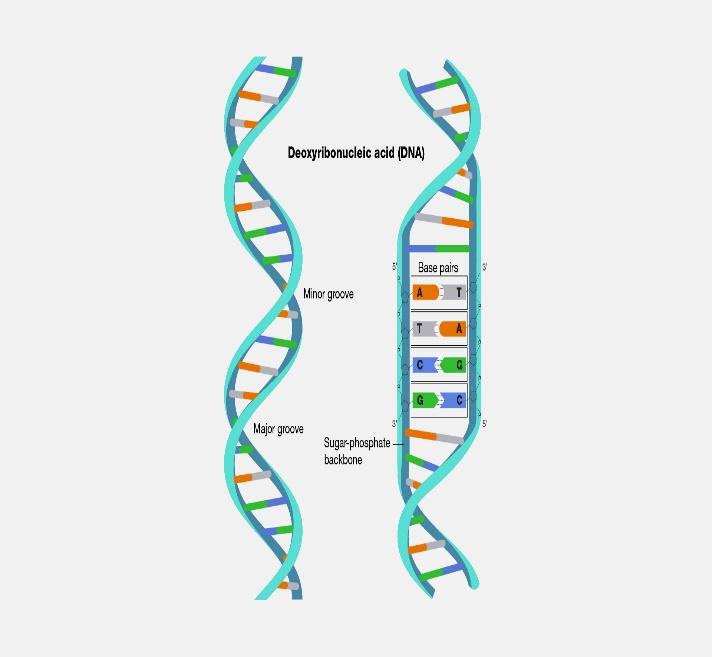
A zygote is a new single-celled organism formed through fertilization. This successful completion of this process marks the beginning of human life. A gene is a segment of DNA (deoxyribonucleic acid) that carries the instructions for building and functioning of living organisms. It is the fundamental unit of heredity and determines various traits and characteristics of an organism. There are an estimated 20,000 to 25,000 genes on each chromosome, a number far below the estimate of 100,000–150,000 held before the work of the Human Genome Project (National Human Genome Research Institute, 2022). Chromosomes contain genetic information from each parent. While other normal human cells have 46 chromosomes (or 23 pairs), gametes contain 23 chromosomes. In meiosis, segments of the chromosomes from each parent form pairs, and genetic segments are exchanged as determined by chance. Because of the unpredictability of this exchange, the likelihood of having genetically identical offspring (and not twins) is one in trillions (Gould, 1997).

What Is the Human Genome Project?
The Human Genome Project is an internationally funded effort to map the locations of human genes and understand the role these genes play in development, health, and illness (check out recent results at www.genome.gov). Genome is a fancy word for all your DNA. Each genome contains the information needed to build and maintain that organism throughout its life (National Human Genome Research Institute, 2022). Your genome is the operating manual containing all the instructions that helped you develop from a single cell into the person you are today. It guides your growth, helps your organs do their jobs, and repairs itself when damaged. Genomes are made of DNA and read like code. This code comprises four types of chemical building blocks, adenine, thymine, cytosine, and guanine, abbreviated with the letters A, T, C, and G. The order of the letters in this code allows DNA to function differently. Therefore, your genome is unique to you! The more you know about your genome and how it works, the more you’ll understand your health and make informed health decisions.
What is meant by Genotypes and Phenotypes?
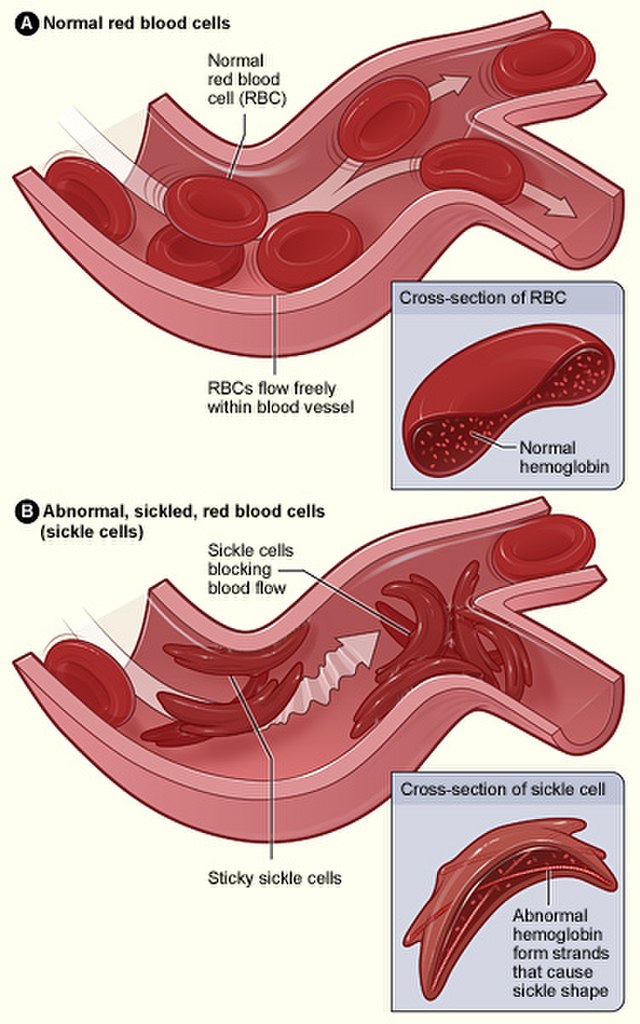
Genotype refers to the information about the genes that a person inherits. Phenotype refers to the features that are expressed. In other words, if you look in the mirror, what you see is your phenotype. The genetic information that encodes your skin color, hair type, or height is your genotype. When determining which genetic information is expressed, some features follow the additive pattern, meaning many genes contribute to an outcome (Berger, 2005). A gene might either be turned on or off, depending on the gene with which it is paired. Some genes are considered dominant because they will be expressed. Other genes, termed recessive, are only expressed without a dominant gene. Some characteristics once considered dominant-recessive, such as eye color, are now believed to result from the interaction between several genes (McKusick, 1998). Dominant traits include curly hair, facial dimples, normal vision, and dark hair. Recessive characteristics include red hair, pattern baldness, and nearsightedness. Huntington’s disease is a dominant disease; sickle cell anemia is a recessive disease. Some traits result from partial dominance or co-dominance in which both genes are influential. For example, if a person inherits recessive genes for sickle cell anemia from each parent, sickle cell anemia disease will occur. But suppose a person has only one recessive gene for the disease. In that case, the person may experience the effects of the disease only under certain circumstances like oxygen deprivation (Berk, 2004) or may never experience any symptoms. Genotype refers to what is coded into genes, but the environment can influence the phenotypic expression of that coding.
What is Epigenetics?
Epigenetics is the study of how your behaviors and environment can cause changes that affect the way your genes work. Gottlieb (1998, 2000, 2002) suggests an analytic framework for the nature/nurture debate that recognizes the interplay between the environment, behavior, and genetic expression. This bidirectional interplay indicates that the environment can affect the expression of genes just as genetic predispositions can impact a person’s potential. Environmental circumstances can trigger symptoms of a genetic disorder. For example, a person with sickle cell anemia, a recessive gene-linked disorder, can experience a sickle cell crisis under conditions of oxygen deprivation. Unlike genetic changes, epigenetic changes are reversible and do not change your DNA sequence but can change how your body reads a DNA sequence. Smoking can result in epigenetic changes. For example, at specific parts of the AHRR gene, smokers tend to have less DNA methylation than non-smokers. The difference is more significant for heavy smokers and long-term smokers. After quitting smoking, former smokers can have increased DNA methylation at this gene. Eventually, they can reach levels similar to those of non-smokers. In some cases, this can happen in under a year, but the length of time depends on how long and how much someone smoked before quitting (McCartney, Stevenson, Hillary, et al., 2018).
What is a Chromosomal Abnormality?
The body is made up of individual units called cells. Your body has many cells, such as skin, liver, and blood. In the center of most cells is a structure called the nucleus. This is where chromosomes are located. A human cell’s typical number of chromosomes is 46: 23 pairs, with an estimated 20,000 to 25,000 genes. One set of 23 chromosomes is inherited from the biological mother (from the egg), and the other set is inherited from the birth father (from the sperm) (National Human Genome Research Institute, 2022).
Of the 23 pairs of chromosomes, the first 22 pairs are called “autosomes.” The final pair is called the “sex chromosomes.” Sex chromosomes determine an individual’s sex: females have two X chromosomes (XX), and males have an X and a Y chromosome (XY). The mother and father each contribute one set of 22 autosomes and one sex chromosome (National Human Genome Research Institute, 2022).
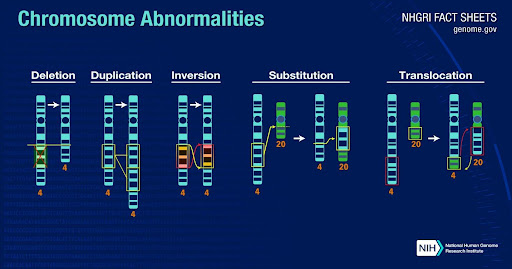
Human development sometimes deviates from the norm, resulting in a chromosomal abnormality. There are many types of chromosome abnormalities. However, these abnormalities are organized into two primary groups: numerical abnormalities and structural abnormalities (Figure 3.4).
Numerical abnormalities occur when an individual is born with too many or too few chromosomes. When an individual is missing one of the chromosomes from a pair, the condition is called monosomy. The condition is called trisomy when an individual has more than two chromosomes instead of a pair. An example of a condition caused by numerical abnormalities is Down syndrome, marked by mental disability, learning difficulties, a characteristic facial appearance, and poor muscle tone (hypotonia) in infancy. An individual with Down syndrome has three copies of chromosome 21 rather than two; for that reason, the condition is also known as Trisomy 21. Turner’s syndrome is an example of monosomy, where an individual lacks a chromosome. In Turner’s syndrome, a female is born with only one sex chromosome, an X, and is usually shorter than average and unable to have children, among other difficulties (National Human Genome Research Institute, 2022).

Structural abnormalities occur when a chromosome’s structure is altered in one of several ways:
- Deletions: A portion of the chromosome is missing or deleted.
- Duplications: A portion of the chromosome is duplicated, resulting in extra genetic material.
- Translocations: A portion of one chromosome is transferred to another chromosome. There are two main types of translocation. In a reciprocal translocation, segments from two different chromosomes have been exchanged. In a Robertsonian translocation, an entire chromosome is attached to another at the centromere.
- Inversions: A portion of the chromosome has broken off, turned upside down, and reattached. As a result, the genetic material is inverted (National Human Genome Research Institute, 2022).
Some chromosome abnormalities occur when there is an error in cell division, resulting in an inherited genetic disorder. Alternatively, genes can become physically damaged due to certain environmental factors such as x-rays or prolonged exposure to toxic substances or may break down due to wear and tear (Feldman, 2020).
The most common cause of chromosomal abnormalities is related to maternal age. A 20-year-old woman has a 1 in 800 chance of having a child with a chromosomal abnormality. Conversely, a 44-year-old woman has a one in 16 chance of having a child with a common chromosomal anomaly.
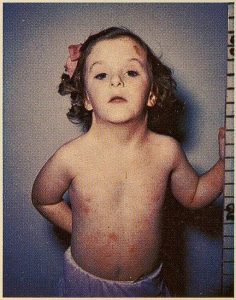
When the abnormality is on pair #23, the result is a sex-linked chromosomal abnormality. A person might have XXY, XYY, XXX, XO, or 45 or 47 chromosomes. Two more common sex-linked chromosomal disorders are Turner’s and Klinefelter’s. Turner’s syndrome occurs in 1 of every 2,500 live female births (Carroll, 2007) when a sperm with an X chromosome fertilizes an ovum without a chromosome. The resulting zygote has an XO composition. Fertilization by a Y sperm is not viable. Turner’s syndrome affects cognitive functioning and sexual maturation. The external genitalia appear normal, but breasts and ovaries do not fully develop, and the woman does not menstruate. Turner’s syndrome also results in short stature and other physical characteristics. Learn more from the Turner Syndrome Society.
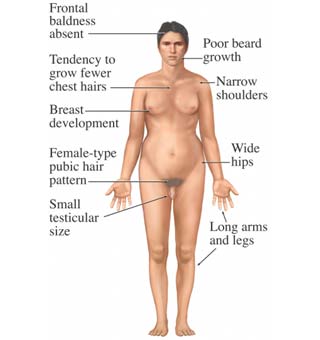
Klinefelter’s syndrome (XXY) occurs in 1 out of 700 live male births and results when a Y sperm fertilizes an ovum containing an extra X chromosome. The Y chromosome stimulates the growth of male genitalia, but the additional X chromosome inhibits this development. An individual with Klinefelter’s syndrome has some breast development, infertility, and low testosterone levels.
If genes inherited from each parent are the same, the child is homozygous for a particular trait and will inherit the trait. If the child inherits a gene from one parent but not the other, the child is heterozygous, and interaction between the genes will, in part, determine whether that trait is expressed (Berk, 2004). This is true for abnormal and typically developed genes.
Nature or Nurture?
For decades, scholars have debated what’s more important for human development, nature or nurture. So far in this chapter, we have focused on nature or the biological aspect of being. Those who argue nature argue that biology provides the blueprint for how you look and act and what you can do. They believe you are biologically predisposed to be an Olympic athlete or scientist. The thinking is that heredity plays the most crucial role in bringing about that feature. However, those who say that nurture is more critical believe that one’s environment is most significant in shaping the way we are. John Watson (1930) asserted if you “…give me a dozen healthy infants, well-formed, and my own specified world to bring them up in and I’ll guarantee to take anyone at random and train him to become any type of specialist I might select—doctor, lawyer, artist—regardless of his talents, penchants, tendencies, abilities, vocations, and race of his ancestors” (p. 104), suggesting that as long as there are no biological deficiencies, any person can be shaped into any person based on their environment. This debate continues with questions about what makes us masculine or feminine (Lippa, 2002), concerns about vision (Mutti, Kadnik, and Adams, 1996), and many other developmental issues. (Check out Google Scholar for over 20,000 entries for “current nature/nurture debates.”) Most scholars agree that there is a constant interplay between the two forces. It is difficult to isolate the root of any single behavior as a result solely of nature or nurture. Most scholars believe determining how much nature or nurture impacts a human feature is difficult to answer. Almost all human features are polygenic (a result of many genes) and multifactorial (a result of many genetic and environmental factors). It’s as if one’s genetic makeup sets up a range of possibilities, which may or may not be realized depending upon one’s environmental experiences. For instance, a person might be genetically predisposed to develop diabetes, but the person’s lifestyle may help bring about the disease.
What Are the Stages of Prenatal Development?
Prenatal development is divided into three stages: the germinal period, the embryonic period, and the fetal period. These stages vary in terms of length and developmental outcomes.
Watch It
Watch these videos from The Baby Center on YouTube to understand the developmental process.
Facts about Conception and Pregnancy
The videos below illustrate the developmental pathway from conception to birth. Please watch each video and note which organs appear at each phase.
Inside Pregnancy weeks 28-37 Mature Content warning.
Inside Pregnancy Labor & Birth Mature Content warning.
What Happens during the Germinal Stage of Prenatal Development?
The germinal period, about 14 days in length, is the shortest stage and lasts from conception to implantation of the zygote (fertilized egg) in the lining of the uterus. During this time, the organism begins cell division and growth. After the fourth doubling, differentiation of the cells also begins to occur. About 60 percent of natural conceptions are estimated to fail to implant in the uterus. The rate is higher for in vitro conceptions.
What Happens during the Embryonic Stage of Prenatal Development?
This period begins once the organism is implanted in the uterine wall. It lasts from the third through the eighth week after conception. During this period, cells continue to differentiate, and 22 days after conception, the neural tube forms, becoming the brain and spinal column. Growth during prenatal development occurs in two primary directions: from head to tail (cephalocaudal development) and from the midline outward (proximodistal development). This means that those structures nearest the head develop before those nearest the feet, and those nearest the torso develop before those away from the center of the body (such as hands and fingers). The head develops in the fourth week, and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. But by the end of this stage, they disappear, and the organism takes on a more human appearance. About 20 percent of organisms fail during embryonic development due to gross chromosomal abnormalities. As in the case of the germinal period, often the mother does not yet know that she is pregnant. During this stage, the major structures of the body take form, making the embryonic period the time when the organism is most vulnerable to the most significant damage if exposed to harmful substances. (We will look at this in the section on teratology below.) The embryo is approximately 1 inch long and weighs about 4 grams at the end of this period. The embryo can move and respond to touch at this time.
What Happens during the Fetal Stage of Prenatal Development?
From the ninth week until birth, the organism is called a fetus. During this stage, the major structures are continuing to develop. By the twelfth week, the fetus has all its body parts, including external genitalia. In the following weeks, the fetus will build hair, nails, and teeth, and the excretory and digestive systems will continue to develop. At the end of the twelfth week, the fetus is about 3 inches long and weighs about 28 grams.
During the fourth to sixth months, the eyes become more sensitive to light, and hearing develops. The respiratory system continues to grow. Reflexes such as sucking, swallowing, and hiccupping develop during the fifth month. Cycles of sleep and wakefulness are present at that time as well. The first chance of survival outside the womb, known as the age of viability, is reached at about 22 and 26 weeks (Moore & Persaud, 1998). Many practitioners hesitate to resuscitate before 24 weeks. Most neurons in the brain have developed by 24 weeks, although they are still rudimentary, and the glial or nurse cells that support neurons continue to grow. At 24 weeks, the fetus can feel pain (Royal College of Obstetricians and Gynecologists, 1997).
The fetus primarily prepares for birth between the seventh and ninth months. It is exercising its muscles; its lungs begin to expand and contract. It develops fat layers under the skin. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy, including a layer of fat accumulated during the eighth month. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
What Determines the Sex of the Fetus?
Twenty-two of those chromosomes from each parent are similar in length to a corresponding chromosome from the other parent. However, the remaining chromosome looks like an X or a Y; half of the male’s sperm contains a Y chromosome, and half contains an X. All ova have two X chromosomes. If the child receives the combination of XY, the child will be genetically male. If it gets the XX combination, the child will be genetically female.
Many potential parents prefer having a boy or a girl and would like to determine the sex of the child. These parents will often meet with a genetic counselor, who can assist with guiding their conception journey, which includes fertility treatments and understanding certain genetic features of the fetus. New technology makes it possible to isolate sperm containing either an X or a Y chromosome, depending on the preference, and use that sperm to fertilize an egg.
How Do We End Up with Twins?
The term zygosity reflects the number of fertilized ova. Monozygotic twins occur when a single zygote or fertilized egg splits apart in the first two weeks of development. The result is the creation of two separate but genetically identical offspring. Because they form from the same zygote, they are always the same sex. About one-third of twins are monozygotic (MZ) twins.
Sometimes, however, dizygotic twins occur when two eggs or ova are released and fertilized by two sperm. About two-thirds of twins are dizygotic (DZ) or fraternal. These two individuals share the same genetic material as children from the same mother and father. Older mothers are more likely to have dizygotic twins than younger mothers, and couples who use fertility drugs are also more likely to give birth to dizygotic twins. Consequently, there has been an increase in fraternal twins in recent years (Bortolus et al., 1999).
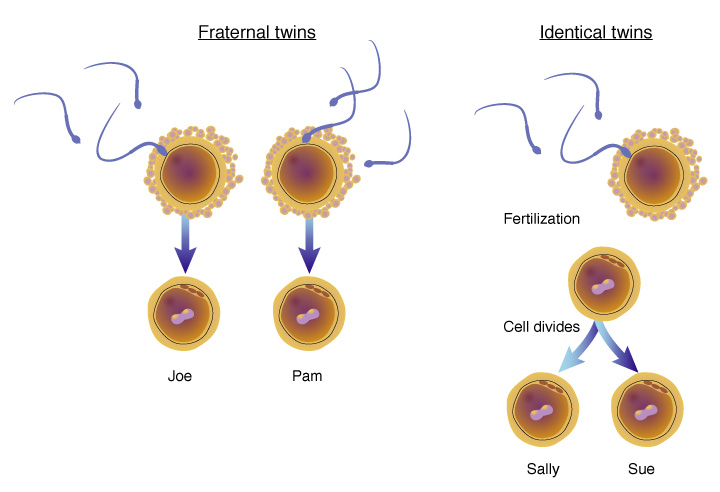
Twins can further discriminate by chorionicity, which refers to the type of placentation and the moment of splitting fertilized ova. DZ twins always have two chorionic (DC=dichorionic) membranes and two placentas. These DZ DC placentas can be separated, connected by membranes, or fused. In the latter case, they will macroscopically appear as one placental mass. In contrast, for MZ twins, chorionicity and the number of placentas depend on the moment of splitting of the fertilized ovum. One-third of the ova split before day four after conception; in such cases, each twin will have its fetal membranes (MZ DC twins) and two separate placentas, as in DZ twins. Two-thirds of the MZ ova split after day four after conception, leading to a single placenta and chorionic membrane (MZ monochorionic [MC] twins) (Gielen, 2007; Derom, Derom, & Vlietinck, 1995). If splitting occurs after day eight (3% of MC twins), twins will have only one amniotic membrane. If splitting takes place after day twelve, conjoined twinning can occur (Gielen, 2007; Machin, 2005).
What Are My Options for Delivery?
People approach childbirth in different ways, depending on their personalities. Some people read everything they can get their hands on, while others are easier-going and rely primarily on what their elders tell them. Ultimately, an informed parent, through their research or by sharing traditional antidotes, is the best parent for the child. Prepared childbirth refers to being physically healthy and as stress-free as possible. Knowing more about what to expect helps them form more realistic images, thus making the adjustment easier. Let’s explore some of the options for childbirth.
The Dick-Read Method of Natural Childbirth: Grantley Dick-Read was an English obstetrician and pioneer of prepared childbirth in the 1930s. In his book Childbirth Without Fear, he suggests that the fear of childbirth increases tension and makes the process of child-bearing more painful. He believed that if mothers were educated, the fear and stress would be reduced, and the need for medication could frequently be eliminated. The Dick-Read method emphasized the use of relaxation and proper breathing with contractions, as well as family support and education. (For more current information on this method, go to Hypno Birthing.) This method influenced the most commonly taught method in the U.S. today, the Lamaze Method.
The Lamaze Method originated in Russia and was brought to the United States in the 1950s by Fernand Lamaze. The emphasis of this method is on teaching the woman to be in control of the process of delivery. It includes learning muscle relaxation, breathing through contractions, having a focal point to look at during contractions, and having a support person who goes through the training process with the mother and serves as a coach during delivery.
Birthing Centers/Birthing Rooms: A birthing room is a hospital room that looks more like a suite in a hotel equipped with a bed that can be converted for delivery. These rooms are also equipped with a bed and monitoring systems for the newborn. The intent is to create a warm environment that is similar to a home but located in the hospital if an emergency arises. These rooms tend to be larger, allowing more family and friends to join in the experience, and stocked with the items the newborn may need.
The Leboyer Method: The Leboyer Method of “Gentle Birthing” incorporates birthing chairs, which use gravity to assist the woman in giving birth. This method involves giving birth in a quiet, dimly lit room and allowing the newborn to lie on the mother’s stomach with the umbilical cord intact for several minutes while being given a warm bath.
Home Birth and Nurse-Midwives: Historically, in the United States, most babies were born under the care of lay midwives. In the 1920s, middle-class women increasingly used doctors to assist with childbirth but lay midwives still helped rural women. The nursing profession began educating nurse-midwives to help these women. Nurse-midwives continued to assist most rural women with delivery until the 1970s and 1980s when their growth was thought to have threatened the medical profession (Weitz, 2007). Since then, nurse-midwives have found sustaining practices with high malpractice insurance costs more challenging. (Many physicians have also changed areas of specialization in response to these costs.) Women at low risk for birth complications can successfully deliver under nurse-midwives care. Because one out of every 20 births involves a complication, most medical professionals recommend that delivery occur in a hospital. However, some couples choose to have their baby at home. About 1 percent of births occur outside a hospital in the United States. Two-thirds of these are homebirths, and midwives assist more than half. Midwives are trained and licensed to assist in delivery and are far less expensive than the cost of a hospital delivery. One-third of out-of-hospital births occur in freestanding clinics, birthing centers, physicians’ offices, or other locations. In the United States, women who have had previous children, who are over 25, and who are White are more likely to have out-of-hospital births (MacDorman et al., 2010).

What Are the Stages of Labor?
The process of childbirth, also known as labor, is typically divided into three stages:
Stage 1 of childbirth is typically the longest and has 3 phases. They are early labor, active labor, and transition. Early labor begins with uterine contractions that may initially last about 30 seconds and be spaced 15 to 20 minutes apart. These increase in duration and frequency to more than a minute in length and about 3 to 4 minutes apart. Typically, doctors advise that they be called when contractions are coming about every 5 minutes. Some women experience false labor or Braxton-Hicks contractions, especially with the first child. These may come and go. They tend to diminish when the mother begins walking around. This stage can last for hours or even days. Real labor pains tend to increase with walking.
Active labor may also be signaled by a bloody discharge expelled from the cervix. In one out of 8 pregnancies, the amniotic sac or water in which the fetus is suspended may break before labor begins. In such cases, the physician may induce labor with medication if it does not start independently. This is done to reduce the risk of infection. In this stage, the cervix dilates more rapidly, and contractions become stronger, longer, and more frequent. The woman may experience intense pain and discomfort. The active labor stage usually lasts a few hours to around 8-12 hours. The final phase of this stage is called transition. During this stage, the cervix or opening to the uterus dilates to 10 centimeters or just under 4 inches. Contractions are intense and frequent, and the woman may experience various emotions, including fatigue, restlessness, and heightened intensity. Transition is often the most challenging and intense part of labor, but it is relatively short, lasting about 30 minutes to 2 hours.
Stage 2 is called pushing and birth. This stage begins when the cervix is fully dilated. The second stage involves the passage of the baby through the birth canal. This stage takes about 10-40 minutes. Contractions usually come about every 2-3 minutes and assist with pushing the baby through the birth canal. Typically, the head is delivered first. The baby is then rotated so that one shoulder can come through and the other. The rest of the baby quickly passes through. At this stage, an episiotomy may be performed to avoid tearing the tissue of the back of the vaginal opening. The baby’s mouth and nose are suctioned out. The umbilical cord is clamped and cut.
Stage 3 is called delivery of the placenta. After the baby is born, the uterus continues to contract to detach and expel the placenta (afterbirth). The placenta or afterbirth is delivered. This typically comes within 20 minutes after delivery. If an episiotomy is performed, it is stitched up during this stage. Medical professionals monitor the mother for any signs of excessive bleeding or complications during this stage.
Assessing the Neonate
There are several ways to assess the condition of the newborn. The Neonatal Behavioral Assessment Scale (NBAS), developed by T. Berry Brazelton, is the most widely used tool. This tool has been used worldwide to help parents learn about their infants and compare infants in different cultures (Brazelton & Nugent, 1995). The baby’s motor development, muscle tone, and stress response are assessed. The Apgar is conducted one minute and five minutes after birth. This is a rapid way to evaluate the newborn’s overall condition. Five measures are assessed: the heart rate, respiration, muscle tone (quickly evaluated by a skilled nurse when the baby is handed to them or by touching the baby’s palm), reflex response (the Babinski reflex is tested), and color. A score of 0 to 2 is given on each feature examined. An Apgar of 5 or less is cause for concern. The second Apgar should indicate improvement with a higher score.
Problems of the Newborn
Low birth weight: A child is considered low birth weight if they weigh less than 5.8 pounds (2500 grams). About 8.2 percent of babies born in the United States have low birth weight (Centers for Disease Control, 2010). A low birth weight baby has difficulty maintaining adequate body temperature because it lacks the fat that would otherwise provide insulation. Such a baby is also at more risk for infection. And 67 percent of these babies are also preterm, making them more at risk for respiratory disease. Low birth weight babies (2 pounds or less) are more likely to develop cerebral palsy. However, many causes of low birth weight are preventable with proper prenatal care.
Premature birth: A child might also have a low birth weight if born at less than 37 weeks gestation (which qualifies it as a preterm baby). Early birth can be triggered by anything that disrupts the mother’s system. For instance, vaginal infections or gum disease can lead to premature birth because such infection causes the mother to release anti-inflammatory chemicals, which, in turn, can trigger contractions. Smoking and the use of other teratogens can lead to preterm birth.

Anoxia: Anoxia is a temporary lack of oxygen to the brain. Difficulty during delivery may lead to anoxia, resulting in brain damage or, in severe cases, death. Babies who suffer both low birth weight and anoxia are more likely to suffer learning disabilities later in life as well.
How Can the Environment Influence Prenatal Development?
Teratology is a branch of the biological sciences dealing with the causes, development, description, and classification of congenital malformations in plants and animals and with the experimental production, in some instances, of these malformations (Britannica, 2023). Congenital malformations arise from an interruption in the early development of the organism. The developing fetus is most at risk during the first three months. Unfortunately, this is a time when many mothers are unaware they are pregnant. Teratogens can contribute to congenital disabilities, including maternal diseases, pollutants, drugs, and alcohol.
There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Berger, 2004). These include:
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, the ears and arms reach their critical periods about six weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed.
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
- Genetics: Genetic makeup also influences a teratogen’s impact on the child. This is suggested by fraternal twin studies exposed to the same prenatal environment yet not experiencing the same teratogenic effect. A mother’s other genetic makeup can also have an effect; some mothers may be more resistant to the teratogenic impacts than others.
- Being male or female: Males are more likely to experience damage due to teratogens than females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.
What are some teratogens?
Parental Drug Use: One of the most commonly used teratogens is alcohol, and because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control or when pregnant (Surgeon General’s Advisory on Alcohol Use During Pregnancy, 2005). Alcohol consumption, particularly during the second month of prenatal development but at any point during pregnancy, may lead to neurocognitive and behavioral difficulties that can last a lifetime. Binge drinking (5 or more on a single occasion) or seven or more drinks during a week puts a child at risk. In extreme cases, alcohol consumption can lead to fetal death. Still, more frequently, it can result in fetal alcohol spectrum disorders (FASD). (This terminology is now used when looking at the effects of exposure and replaces the term fetal alcohol syndrome. It is preferred because it recognizes that symptoms occur on a spectrum and that not all individuals have the same characteristics.) Children with FASD share certain physical features such as flattened noses, small eye holes, small heads, intellectual developmental delay, and behavioral problems. Those with FASD are more at risk for lifelong problems such as criminal behavior, psychiatric issues, and unemployment (CDC, 2006). The terms alcohol-related neurological disorder (ARND) and alcohol-related congenital disabilities (ARCD) have replaced the term fetal alcohol effects to refer to those with less extreme symptoms of FASD. ARCD includes kidney, bone, and heart problems.
Tobacco is the second most widely used teratogen, and the number of adolescent females who smoke is increasing. In fact, among adolescents, females are just as likely to smoke as males. Tobacco use during preconception by either the mother or father (Klonoff-Cohen & Lam-Kruglick, 2001) and during pregnancy has been associated with low birth weight, placenta previa, preterm delivery, fetal growth restriction, and sudden infant death syndrome (Center for Disease Control, 2004).
Illicit drugs, as well as prescribed medications, can have serious teratogenic effects. Opioids are drugs that manage pain but have serious risks, such as addiction. Opioids can be defined as illicit (Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, 2022). Heroin is an illegal opioid. Fentanyl is a prescription opioid that can be used to treat severe pain; it may also be used illicitly. Opioid use disorder among pregnant women is a significant public health concern in the United States. According to 2019 self-reported data, about 7% of women reported using prescription opioid pain relievers during pregnancy. Of those, 1 in 5 reported misuse of prescription opioids. Women with opioid-related diagnoses documented at delivery increased by 131% from 2010 to 2017. Opioid use disorder during pregnancy has been linked with severe adverse health outcomes for pregnant women and developing babies, including preterm birth, stillbirth, maternal mortality, and neonatal abstinence syndrome (NAS). NAS is a group of withdrawal symptoms that most commonly occurs in newborns after exposure to opioids during pregnancy.
Often, women ingest illicit drugs and engage with multiple types of drugs. The use of substances during pregnancy has been well documented. Engaging in cocaine use is connected with low birth weight, stillbirths, and spontaneous abortion. Heavy marijuana use is associated with brain damage, and mothers addicted to heroin often pass that addiction to their children. Many medications do not include adequate information on the risks posed if taken during pregnancy (Centers for Disease Control, 2004).
Paternal lifestyle during sperm development can have an impact on fetal development as well. Use of cannabis and cocaine close to pregnancy seems closely linked to other risk factors (Munch, Skurtveit, Handal, & Skovlund, 2020), including SIDS (Klonoff-Cohen & Lam-Kruglick, 2001). Paternal cocaine use preconception is associated with increased abnormalities in the fetus (Yazigi, Odem, & Polakoski, 1991).
Pollutants: Some environmental contaminants of major concern include lead poisoning, which relates to low birth weight and slowed neurological development. Children who live in older housing where lead-based paints have been used have been known to eat peeling paint chips, thus being exposed to lead. The chemicals in certain herbicides are also potentially damaging. Radiation is another environmental hazard. The child may suffer congenital deformities if a mother is exposed to radiation, particularly during the first three months of pregnancy. There is also an increased risk of miscarriage and stillbirth. Mercury leads to physical deformities and mental retardation (Dietrich, 1999).
Abortions: Things often do not go as planned during a pregnancy. The section above discussed environmental causes for the fetus developing an abnormality. This can leave the parents in a precarious situation. Often, a child is born with challenges ranging from mild to severe. However, sometimes, that pregnancy ends through either a miscarriage or abortion. A miscarriage, also known as spontaneous abortion, refers to the natural loss of a pregnancy before the twentieth week of gestation. Miscarriages typically occur due to fetal abnormalities or issues with the pregnancy itself, such as chromosomal abnormalities, hormonal problems, maternal health conditions, or uterine abnormalities. Miscarriages are usually unplanned and occur without any intentional intervention.
Spontaneous abortion is experienced in an estimated 20-40 percent of undiagnosed pregnancies and another 10 percent of diagnosed pregnancies, usually occurring before the twelfth week of pregnancy. Cramping and bleeding result, and regular periods return after several months. Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems, but miscarriage can also result from defective sperm (Carrell et al., 2003).
Conversely, abortion is the deliberate termination of a pregnancy. It can be performed by taking medication prescribed by a licensed doctor or by surgical procedures, and it is typically a planned decision made by the woman or couple involved. Abortions can be elective, meaning they are chosen for personal or medical reasons. In some cases, abortions may also be performed for clinical reasons, such as when the continuation of the pregnancy poses a risk to the mother’s life or health or if the fetus has severe abnormalities incompatible with life.
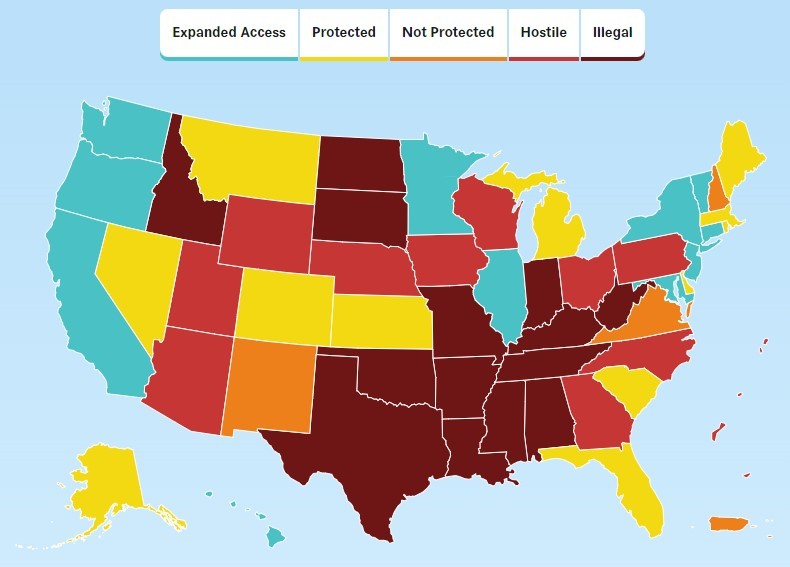
Abortion was legal in the United States for 49 years due to a decision made by the Supreme Court, often referred to as Roe v. Wade. However, the 2021 U.S. Supreme Court overturned the ruling giving access to abortion care. Laws vary by state and are constantly changing. See the map below provided by the Center for Reproductive Rights that shows where states stand on abortion access as of July 2023.
References
Berk, L. (2004). Development through the lifespan(3rd ed.). Boston: Allyn and Bacon.
Berger, K. S. (2005). The developing person through the lifespan(6th ed.). New York: Worth.
Bortolus, R., Parazzini, F., Chatenoud, L., Benzi, G., Bianchi, M. M., & Marini, A. (1999). The epidemiology of multiple births. Human Reproduction Update, 5, 179-187.
Brazelton, T. B., & Nugent, J. K. (1995). Neonatal behavioral assessment scale. London: Mac Keith Press.
Carroll, J. L. (2007). Sexuality now: Embracing diversity (2nd ed.). Belmont, CA: Thomson.
Carrell, D. T., Wilcox, A. L., Lowry, L., Peterson, C. M., Jones, K. P., & Erikson, L. (2003). Elevated sperm chromosome aneuploidy and apoptosis in patients with unexplained recurrent pregnancy loss. Obstetrics and Gynecology, 101(6), 1229–1235.
CDC/ National Center for Health Statistics. (2022). https://www.cdc.gov/nchs/pressroom/sosmap/infant_mortality_rates/infant_mortality.htm
Derom, R., Derom, C., & Vlietinck, R. (1995). Placentation. In Keith, L. G., Papiernik, E., Keith, D. M., Luke, B. (eds.) Multiple pregnancy: Epidemiology, Gestation & Perinatal outcome. The Parthenon Publishing Group, New York, pp 113-128.
Feldman, R. S. (2020). Development across the Lifespan (9th Edition). Upper Saddle River, New Jersey: Pearson/Prentice Hall.
Gielen, M. J. F. (2007). Aspects of prenatal growth and further development in twins. [Doctoral Thesis, Maastricht University]. Ponsen & Looijen B. V. https://doi.org/10.26481/dis.20071011mg
Gould, J. L. (1997). Biological science. New York: Norton.
Gottlieb, G. (1998). Normally occurring environmental and behavioral influences on gene activity: From central dogma to probabilistic epigenesis. Psychological Review, 105, 792-802.
Gottlieb, G. (2000). Environmental and behavioral influences on gene activity. Current Directions in Psychological Science, 9, 93-97.
Gottlieb, G. (2002). Individual development and evolution: The genesis of novel behavior. New York: Oxford University Press.
Hoyert, D. L. (2022). Maternal mortality rates in the United States, 2020. NCHS Health E-Stats. 2022. DOI: https://dx.doi.org/10.15620/cdc:113967
Klonoff-Cohen, H., & Lam-Kruglick, P. (2001). Maternal and Paternal Recreational Drug Use and Sudden Infant Death Syndrome. Archives of Pediatrics & Adolescent Medicine, 155(7), 765. https://doi.org/10.1001/archpedi.155.7. Louisiana’s healthcare deserts put women babies at risk, advocates and doctors say | 60 Minutes – CBS News, retrieved 8/23/2023.
McCartney, D., Stevenson, A., Hillary, R., et al. (2018). Epigenetic signatures of starting and stopping smoking. EBioMedicine 2018; 37:214-220
MacDorman, M., Menacker, F., & Declercq, E. (2010, August 30). Trends and Characteristics of Home and Other Hospital Births in the United States, 1990–2006 (United States, Center for Disease Control). Retrieved December 22, 2010, from http://www.cdc.gov/nchs/data/nvsr/nvsr58;nvsr58_11.PDF
Machin, G. A. (1996). Some causes of genotypic and phenotypic discordance in monozygotic twin pairs. Am J Med Genet 61:216-228.
Mackon, N., & Fauser, B. (2000). Aspects of ovarian follicle development throughout life. Hormone Research, 52, 161-170.
McKusick, V. A. (1998). Mendelian inheritance in man: A catalog of human genes and genetic disorders. Baltimore, MD: Johns Hopkins University Press.
Munch, E. L., Skurtveit, S., Handal, M., & Skovlund, E. (2019). Pre-conception use of cannabis and cocaine among men with pregnant partners. Nordic Studies on Alcohol and Drugs, 37(1), 43–53. https://doi.org/10.1177/1455072519879564
Rome, E. (1998). Anatomy and physiology of sexuality and reproduction. In The New Our Bodies, Ourselves (pp. 241-258). Carmichael, CA: Touchstone Books.
Shahin, Z., Hardwick, I., Jeffery, N., Jordan, J., & Mase, W. (2020). Maternal Mortality among African American Women in the State of Georgia, Causes, Policy, and Ethical Considerations. Journal of the Georgia Public Health Association, 8(1). https://doi.org/10.20429/jgpha.2020.080104
United States Center for Disease Control. (n.d.). The Health Consequences of Smoking: 2004 Report of the Surgeon General. Retrieved August 14, 2004, from http://www.cdc.gov/tobacco/sqr/sqr_2004
U.S. Department of Health & Human Services. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, 2022. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/substance-abuse/substance-abuse-during-pregnancy.htm
Yazigi, R. A., Odem, R. R., & Polakoski, K. L. (1991). Demonstration of specific binding of cocaine to human spermatozoa. JAMA, 266(14), 1956–1959.
Attribution
Portions of this chapter were adapted by Dr. Cynthia Thomas from select chapters in Lumen Learning’s Lifespan Development, authored by Martha Lally and Suzanne Valentine-French, available under a Creative Commons Attribution-NonCommercial-ShareAlike license, and Waymaker Lifespan Development, written by Sarah Carter for Lumen Learning and available under a Creative Commons Attribution license. Some selections from Lumen Learning were adapted from previously shared content from Laura Overstreet’s Lifespan Psychology course (PSYC 2000) and Wikipedia.
Cynthia Thomas, PhD contributed the following changes to this chapter:
- The cultural opener that focuses on the state of maternal health in the US. Includes statistics and comparison to other industrialized countries, as well as highlighting Louisiana has the highest maternal mortality rate in the US as well has the highest rate for African American women.
- Revised the section on conception.
- Extended the section on the Human Genome Project to include a description of the project, links to the project’s website, a video to aid in understanding.
- Extended the section on chromosomal abnormalities to include a description of different classifications of abnormalities.
- Refined the sections that focus on the different stages of pregnancy. Provided an illustration on the development of MZ and DZ twins.
- Expanded the section on environmental impacts to pregnancy to include a definition of teratology and examples of different teratogens. Highlighted research that focuses on paternal drug use, disease, and work-related toxins.
- Updated information related to the overturning of Roe v/s Wade.
Media Attributions
- Newborn baby feet © Picnoi Photos is licensed under a CC BY (Attribution) license
- Figure 3-1 maternal mortality © National Center for Health Statistics, National Vital Statistics System, Mortality. is licensed under a Public Domain license
- junior-reis-6jaucC4h0Aw-unsplash © Junior REIS is licensed under a CC BY (Attribution) license
- DNA strand © National Human Genome Research Institute is licensed under a Public Domain license
- 640px-Sickle_cell_01 © The National Heart, Lung, and Blood Institute (NHLBI) is licensed under a Public Domain license
- Figure 3.3 Chromosome Abnormalities © NIH/ National Human Genome Research Institute is licensed under a Public Domain license
- Down_Syndrome_Child © NadineLive is licensed under a CC BY-SA (Attribution ShareAlike) license
- Turner_Syndrome_3 © Sydney S. Gellis and Murray Feingold is licensed under a Public Domain license
- Klinefelter’s_syndrome © Unknown is licensed under a CC BY-SA (Attribution ShareAlike) license
- Identical_twins_lg © National Human Genome Research Institute is licensed under a Public Domain license
- 1024px-Midwife_home_appointment © Eyeliam is licensed under a CC BY (Attribution) license
- Premature_infant_with_ventilator © Ceejayoz is licensed under a CC BY (Attribution) license
- Figure 3.8. Abortion in United States © Center for Reproductive Rights is licensed under a CC BY (Attribution) license
Maternal death - the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
A zygote is a new single-celled organism formed through fertilization.
A gene is a segment of DNA (deoxyribonucleic acid) that carries the instructions for building and functioning of living organisms. It is the fundamental unit of heredity and determines various traits and characteristics of an organism.
Genome refers to all your DNA. Each genome contains the information needed to build and maintain that organism throughout its life.
Genotype refers to the information about the genes that a person inherits.
Phenotype refers to the features that are expressed.
Epigenetics is the study of how your behaviors and environment can cause changes that affect the way your genes work.
Numerical abnormalities occur when an individual is born with too many or too few chromosomes.
Structural abnormalities occur when a chromosome's structure is altered.
Turner’s syndrome (TS) is a genetic disorder caused by a sex chromosome monosomy; compared to the two sex chromosomes (XX or XY) in most people, it only affects women. Signs and symptoms vary among those affected. Turner’s syndrome has several physical and psychological impacts, including short stature, heart defects, neck webbing, delayed or absent puberty, and infertility.
Klinefelter’s syndrome (KS) is a genetic disorder predominantly found in those assigned male at birth. People with KS have an additional copy of the X chromosome. The primary features are infertility and small, poorly functioning testicles (if present). Symptoms are often noticed only at puberty.
Monozygotic twins occur when a single zygote or fertilized egg splits apart in the first two weeks of development.
Dizygotic twins occur when two eggs or ova are released and fertilized by two sperm.
Teratology is a branch of the biological sciences dealing with the causes, development, description, and classification of congenital malformations in plants and animals and with the experimental production, in some instances, of these malformations (Britannica, 2023).
Teratogens can contribute to birth defects, including maternal diseases, pollutants, drugs, and alcohol.
Miscarriage, also known as spontaneous abortion, refers to the natural loss of a pregnancy before the 20th week of gestation.
Abortion is the deliberate termination of a pregnancy.

