22.5 Hormonal Control of Human Reproduction
Jung Choi; Mary Ann Clark; and Matthew Douglas
Learning Objectives
By the end of this chapter, you will be able to do the following:
- Describe the roles of male and female reproductive hormones
- Discuss the interplay of the ovarian and menstrual cycles
- Describe the process of menopause
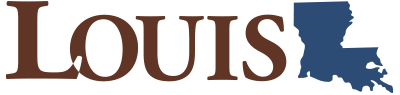
The human male and female reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. In both sexes, the hypothalamus monitors and causes the release of hormones from the pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. Note that the body must reach puberty in order for the adrenals to release the hormones that must be present for GnRH to be produced. Although FSH and LH are named after their functions in female reproduction, they are produced in both sexes and play important roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
Male Hormones
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells to begin facilitating spermatogenesis using negative feedback, as illustrated in the figure below. LH also enters the testes and stimulates the interstitial cells of Leydig to make and release testosterone into the testes and the blood.
Testosterone, the hormone responsible for the secondary sexual characteristics that develop in the male during adolescence, stimulates spermatogenesis. These secondary sex characteristics include a deepening of the voice, the growth of facial, axillary, and pubic hair, and the beginnings of the sex drive.
A negative feedback system occurs in the male with rising levels of testosterone acting on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH. The Sertoli cells produce the hormone inhibin, which is released into the blood when the sperm count is too high. This inhibits the release of GnRH and FSH, which will cause spermatogenesis to slow down. If the sperm count reaches 20 million/ml, the Sertoli cells cease the release of inhibin, and the sperm count increases.
Female Hormones
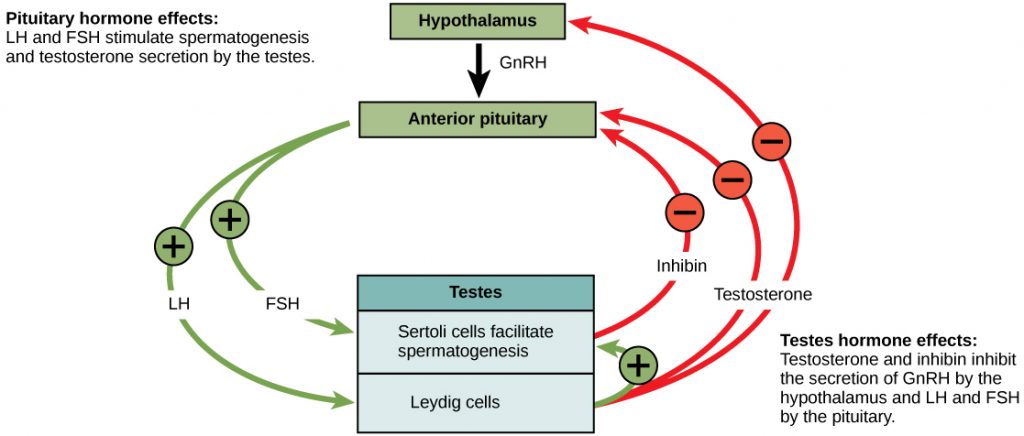
The control of reproduction in females is more complex. As with the male, the anterior pituitary hormones cause the release of the hormones FSH and LH. In addition, estrogens and progesterone are released from the developing follicles. Estrogen is the reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption; it is also responsible for the secondary sexual characteristics of females. These include breast development, flaring of the hips, and a shorter period necessary for bone maturation. Progesterone assists in endometrial regrowth and inhibition of FSH and LH release.
In females, FSH stimulates the development of egg cells called ova, which develop in structures called follicles. Follicle cells produce the hormone inhibin, which inhibits FSH production. LH also plays a role in the development of ova, induction of ovulation, and stimulation of estradiol and progesterone production by the ovaries. Estradiol and progesterone are steroid hormones that prepare the body for pregnancy. Estradiol produces secondary sex characteristics in females, while both estradiol and progesterone regulate the menstrual cycle.
The Ovarian Cycle and the Menstrual Cycle
The ovarian cycle governs the preparation of endocrine tissues and release of eggs, while the menstrual cycle governs the preparation and maintenance of the uterine lining. These cycles occur concurrently and are coordinated over a 22–32 day cycle, with an average length of 28 days.
The first half of the ovarian cycle is the follicular phase shown in the figure below. Slowly rising levels of FSH and LH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they begin releasing estrogens and a low level of progesterone. Progesterone maintains the endometrium to help ensure pregnancy. The trip through the fallopian tube takes about seven days. At this stage of development, called the morula, there are 30–60 cells. If pregnancy implantation does not occur, the lining is sloughed off. After about five days, estrogen levels rise and the menstrual cycle enters the proliferative phase. The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the end of the last cycle.
Visual Connection
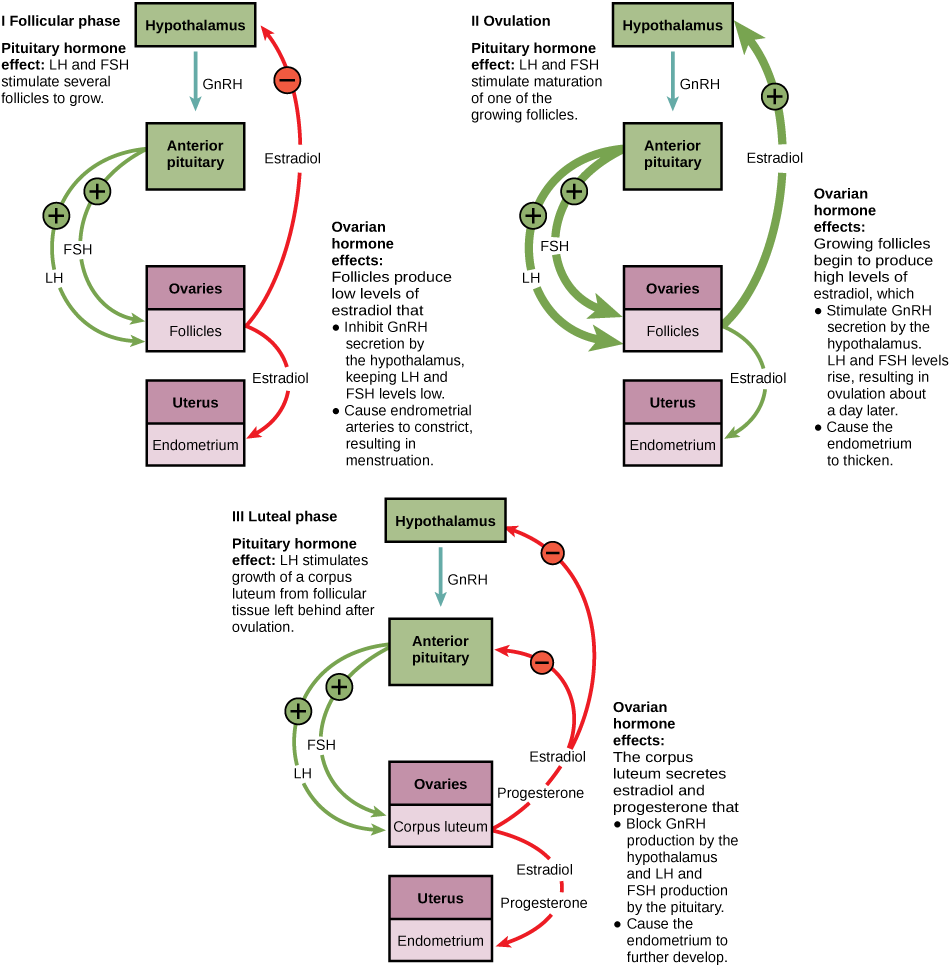
Just prior to the middle of the cycle (approximately day 14), the high level of estrogen causes FSH and especially LH to rise rapidly, then fall. The spike in LH causes ovulation: the most mature follicle, like that shown in the figure below, ruptures and releases its egg. The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.

Following ovulation, the ovarian cycle enters its luteal phase, illustrated in the figure below, and the menstrual cycle enters its secretory phase, both of which run from about day 15 to 28. The luteal and secretory phases refer to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a structure called a corpus luteum. The corpus luteum produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus is being prepared to accept a fertilized egg, should it occur during this cycle. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days.
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates, and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again. The figure below visually compares the ovarian and uterine cycles as well as the commensurate hormone levels.
Visual Connection
Menopause
As women approach their mid-40s to mid-50s, their ovaries begin to lose their sensitivity to FSH and LH. Menstrual periods become less frequent and finally cease; this is menopause. There are still eggs and potential follicles on the ovaries, but without the stimulation of FSH and LH, they will not produce a viable egg to be released. The outcome of this is the inability to have children.
The side effects of menopause include hot flashes, heavy sweating (especially at night), headaches, some hair loss, muscle pain, vaginal dryness, insomnia, depression, weight gain, and mood swings. Estrogen is involved in calcium metabolism, and without it, blood levels of calcium decrease. To replenish the blood, calcium is lost from bone, which may decrease bone density and lead to osteoporosis. Supplementation of estrogen in the form of hormone replacement therapy (HRT) can prevent bone loss, but the therapy can have negative side effects. While HRT is thought to give some protection from colon cancer, osteoporosis, heart disease, macular degeneration, and possibly depression, its negative side effects include increased risk of stroke or heart attack, blood clots, breast cancer, ovarian cancer, endometrial cancer, gall bladder disease, and possibly dementia.
Career Connection
Reproductive Endocrinologist
A reproductive endocrinologist is a physician who treats a variety of hormonal disorders related to reproduction and infertility in both men and women. The disorders include menstrual problems, infertility, pregnancy loss, sexual dysfunction, and menopause. Doctors may use fertility drugs, surgery, or assisted reproductive techniques (ART) in their therapy. ART involves the use of procedures to manipulate the egg or sperm to facilitate reproduction, such as in vitro fertilization.
Reproductive endocrinologists undergo extensive medical training, first in a four-year residency in obstetrics and gynecology, then in a three-year fellowship in reproductive endocrinology. To be board certified in this area, the physician must pass written and oral exams in both areas.
Section Summary
The male and female reproductive cycles are controlled by hormones released from the hypothalamus and anterior pituitary as well as hormones from reproductive tissues and organs. The hypothalamus monitors the need for the FSH and LH hormones made and released from the anterior pituitary. FSH and LH affect reproductive structures to cause the formation of sperm and the preparation of eggs for release and possible fertilization. In the male, FSH and LH stimulate Sertoli cells and interstitial cells of Leydig in the testes to facilitate sperm production. The Leydig cells produce testosterone, which also is responsible for the secondary sexual characteristics of males. In females, FSH and LH cause estrogen and progesterone to be produced. They regulate the female reproductive system which is divided into the ovarian cycle and the menstrual cycle. Menopause occurs when the ovaries lose their sensitivity to FSH and LH and the female reproductive cycles slow to a stop.
Review Questions
Critical Thinking Questions
Glossary
- estrogen
- reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption
- follicle-stimulating hormone (FSH)
- reproductive hormone that causes sperm production in men and follicle development in women
- gonadotropin-releasing hormone (GnRH)
- hormone from the hypothalamus that causes the release of FSH and LH from the anterior pituitary
- inhibin
- hormone made by Sertoli cells; provides negative feedback to hypothalamus in control of FSH and GnRH release
- interstitial cell of Leydig
- cell in seminiferous tubules that makes testosterone
- luteinizing hormone (LH)
- reproductive hormone in both men and women, causes testosterone production in men and ovulation and lactation in women
- menopause
- loss of reproductive capacity in women due to decreased sensitivity of the ovaries to FSH and LH
- menstrual cycle
- cycle of the degradation and regrowth of the endometrium
- ovarian cycle
- cycle of preparation of egg for ovulation and the conversion of the follicle to the corpus luteum
- ovulation
- release of the egg by the most mature follicle
- progesterone
- reproductive hormone in women; assists in endometrial regrowth and inhibition of FSH and LH release
- Sertoli cell
- cell in seminiferous tubules that assists developing sperm and makes inhibin
- testosterone
- reproductive hormone in men that assists in sperm production and promoting secondary sexual characteristics