18.4 Breathing
Mary Ann Clark; Jung Choi; and Matthew Douglas
Learning Objectives
By the end of this section, you will be able to do the following:
- Describe how the structures of the lungs and thoracic cavity control the mechanics of breathing
- Explain the importance of compliance and resistance in the lungs
- Discuss problems that may arise due to a V/Q mismatch
Mammalian lungs are located in the thoracic cavity, where they are surrounded and protected by the rib cage, intercostal muscles, and bound by the chest wall. The bottom of the lungs is contained by the diaphragm, a skeletal muscle that facilitates breathing. Breathing requires the coordination of the lungs, the chest wall, and most importantly, the diaphragm.
Types of Breathing
Amphibians have evolved multiple ways of breathing. Young amphibians, like tadpoles, use gills to breathe, and they don’t leave the water. Some amphibians retain gills for life. As the tadpole grows, the gills disappear and lungs grow. These lungs are primitive and not as evolved as mammalian lungs. Adult amphibians lack or have a reduced diaphragm, so breathing via lungs is forced. The other means of breathing for amphibians is diffusion across the skin. To aid this diffusion, amphibian skin must remain moist.
Birds face a unique challenge with respect to breathing: they fly. Flying consumes a great amount of energy; therefore, birds require a lot of oxygen to aid their metabolic processes. Birds have evolved a respiratory system that supplies them with the oxygen needed to enable flying. Similar to mammals, birds have lungs, which are organs specialized for gas exchange. Oxygenated air, taken in during inhalation, diffuses across the surface of the lungs into the bloodstream, and carbon dioxide diffuses from the blood into the lungs and is expelled during exhalation. The details of breathing between birds and mammals differ substantially.
In addition to lungs, birds have air sacs inside their body. Air flows in one direction from the posterior air sacs to the lungs and out of the anterior air sacs. The flow of air is in the opposite direction from blood flow, and gas exchange takes place much more efficiently. This type of breathing enables birds to obtain the requisite oxygen, even at higher altitudes where the oxygen concentration is low. This directionality of airflow requires two cycles of air intake and exhalation to completely get the air out of the lungs.
Evolution Connection: Avian Respiration
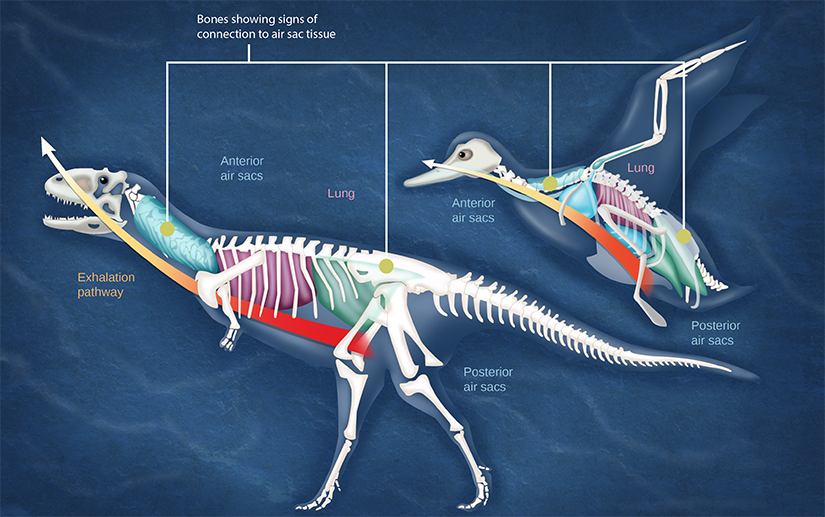
During inhalation in birds, air passes from the beak down the trachea to the posterior air sac located behind the lungs. From the posterior air sac, air enters the lungs, and the anterior air sac in front of the lungs. Air from both air sacs also enters hollows in bones. During exhalation air from hollows in the bones enters the air sacs, then the lungs, then the trachea, where it exits through the beaks. The above illustration compares a dinosaur and a bird. Both have anterior air sacs in front of the lungs, and posterior air sacs behind them. The air sacs connect to hollow openings in bones.
Most of us consider that dinosaurs are extinct. However, modern birds are descendants of avian dinosaurs. The respiratory system of modern birds has been evolving for hundreds of millions of years.
All mammals have lungs that are the main organs for breathing. Lung capacity has evolved to support the animal’s activities. During inhalation, the lungs expand with air, and oxygen diffuses across the lung’s surface and enters the bloodstream. During exhalation, the lungs expel air and lung volume decreases. In the next few sections, the process of human breathing will be explained.
The Mechanics of Human Breathing
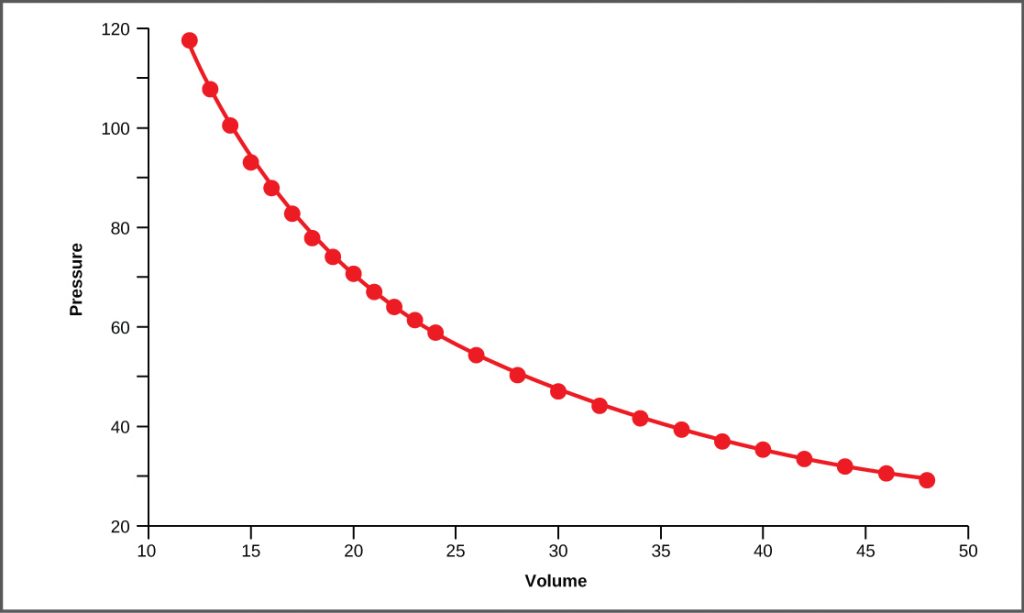
Boyle’s Law is the gas law that states that in a closed space, pressure and volume are inversely related. As volume decreases, pressure increases and vice versa (see figure below). The relationship between gas pressure and volume helps to explain the mechanics of breathing.
There is always a slightly negative pressure within the thoracic cavity, which aids in keeping the airways of the lungs open. During inhalation, volume increases as a result of contraction of the diaphragm, and pressure decreases (according to Boyle’s Law). This decrease of pressure in the thoracic cavity relative to the environment makes the cavity less than the atmosphere (see figure “a” below). Because of this drop in pressure, air rushes into the respiratory passages. To increase the volume of the lungs, the chest wall expands. This results from the contraction of the intercostal muscles, the muscles that are connected to the rib cage. Lung volume expands because the diaphragm contracts and the intercostal muscles contract, thus expanding the thoracic cavity. This increase in the volume of the thoracic cavity lowers pressure compared to the atmosphere, so air rushes into the lungs, thus increasing its volume. The resulting increase in volume is largely attributed to an increase in alveolar space, because the bronchioles and bronchi are stiff structures that do not change in size.
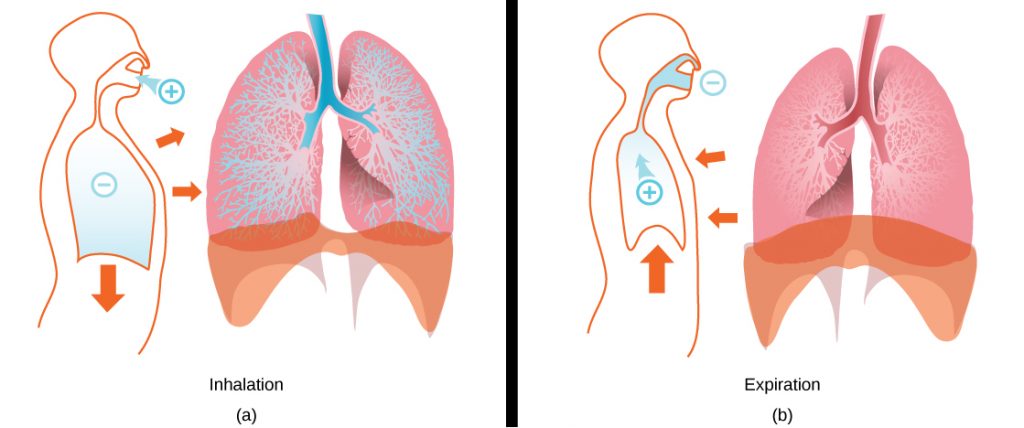
The chest wall expands out and away from the lungs. The lungs are elastic; therefore, when air fills the lungs, the elastic recoil within the tissues of the lung exerts pressure back toward the interior of the lungs. These outward and inward forces compete to inflate and deflate the lung with every breath. Upon exhalation, the lungs recoil to force the air out of the lungs, and the intercostal muscles relax, returning the chest wall back to its original position (see figure “b” below). The diaphragm also relaxes and moves higher into the thoracic cavity. This increases the pressure within the thoracic cavity relative to the environment, and air rushes out of the lungs. The movement of air out of the lungs is a passive event. No muscles are contracting to expel the air.
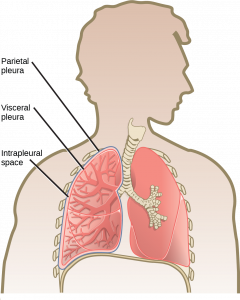
Each lung is surrounded by an invaginated sac. The layer of tissue that covers the lung and dips into spaces is called the visceral pleura. A second layer of parietal pleura lines the interior of the thorax (see figure below). The space between these layers, the intrapleural space, contains a small amount of fluid that protects the tissue and reduces the friction generated from rubbing the tissue layers together as the lungs contract and relax. Pleurisy results when these layers of tissue become inflamed; it is painful because the inflammation increases the pressure within the thoracic cavity and reduces the volume of the lung.
The Work of Breathing
The number of breaths per minute is the respiratory rate. On average, under non-exertion conditions, the human respiratory rate is 12–15 breaths/minute. The respiratory rate contributes to the alveolar ventilation, or how much air moves into and out of the alveoli. Alveolar ventilation prevents carbon dioxide buildup in the alveoli. There are two ways to keep the alveolar ventilation constant: increase the respiratory rate while decreasing the tidal volume of air per breath (shallow breathing), or decrease the respiratory rate while increasing the tidal volume per breath. In either case, the ventilation remains the same, but the work done and type of work needed are quite different. Both tidal volume and respiratory rate are closely regulated when oxygen demand increases.
There are two types of work conducted during respiration, flow-resistive and elastic work. Flow-resistive refers to the work of the alveoli and tissues in the lung, whereas elastic work refers to the work of the intercostal muscles, chest wall, and diaphragm. Increasing the respiration rate increases the flow-resistive work of the airways and decreases the elastic work of the muscles. Decreasing the respiratory rate reverses the type of work required.
Surfactant
The air-tissue/water interface of the alveoli has a high surface tension. This surface tension is similar to the surface tension of water at the liquid-air interface of a water droplet that results in the bonding of the water molecules together. Surfactant is a complex mixture of phospholipids and lipoproteins that works to reduce the surface tension that exists between the alveoli tissue and the air found within the alveoli. By lowering the surface tension of the alveolar fluid, it reduces the tendency of alveoli to collapse.
Surfactant works like a detergent to reduce the surface tension and allows for easier inflation of the airways. When a balloon is first inflated, it takes a large amount of effort to stretch the plastic and start to inflate the balloon. If a little bit of detergent was applied to the interior of the balloon, then the amount of effort or work needed to begin to inflate the balloon would decrease, and it would become much easier to start blowing up the balloon. This same principle applies to the airways. A small amount of surfactant to the airway tissues reduces the effort or work needed to inflate those airways. Babies born prematurely sometimes do not produce enough surfactant. As a result, they suffer from respiratory distress syndrome, because it requires more effort to inflate their lungs. Surfactant is also important for preventing collapse of small alveoli relative to large alveoli.
Lung Resistance and Compliance
Pulmonary diseases reduce the rate of gas exchange into and out of the lungs. Two main causes of decreased gas exchange are compliance (how elastic the lung is) and resistance (how much obstruction exists in the airways). A change in either can dramatically alter breathing and the ability to take in oxygen and release carbon dioxide.
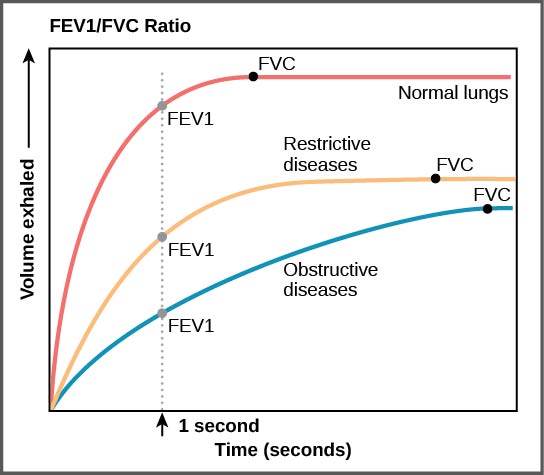
Examples of restrictive diseases are respiratory distress syndrome and pulmonary fibrosis. In both diseases, the airways are less compliant and they are stiff or fibrotic. There is a decrease in compliance because the lung tissue cannot bend and move. In these types of restrictive diseases, the intrapleural pressure is more positive and the airways collapse upon exhalation, which traps air in the lungs. Forced or functional vital capacity (FVC), which is the amount of air that can be forcibly exhaled after taking the deepest breath possible, is much lower than in normal patients, and the time it takes to exhale most of the air is greatly prolonged (see figure below). A patient suffering from these diseases cannot exhale the normal amount of air.
Obstructive diseases and conditions include emphysema, asthma, and pulmonary edema. In emphysema, which mostly arises from smoking tobacco, the walls of the alveoli are destroyed, decreasing the surface area for gas exchange. The overall compliance of the lungs is increased, because as the alveolar walls are damaged, lung elastic recoil decreases due to a loss of elastic fibers, and more air is trapped in the lungs at the end of exhalation. Asthma is a disease in which inflammation is triggered by environmental factors. Inflammation obstructs the airways. The obstruction may be due to edema (fluid accumulation), smooth muscle spasms in the walls of the bronchioles, increased mucus secretion, damage to the epithelia of the airways, or a combination of these events. Those with asthma or edema experience increased occlusion from increased inflammation of the airways. This tends to block the airways, preventing the proper movement of gases (see figure below). Those with obstructive diseases have large volumes of air trapped after exhalation and breathe at a very high lung volume to compensate for the lack of airway recruitment.
Dead Space: V/Q Mismatch
Pulmonary circulation pressure is very low compared to that of the systemic circulation. It is also independent of cardiac output. This is because of a phenomenon called recruitment, which is the process of opening airways that normally remain closed when cardiac output increases. As cardiac output increases, the number of capillaries and arteries that are perfused (filled with blood) increases. These capillaries and arteries are not always in use but are ready if needed. At times, however, there is a mismatch between the amount of air (ventilation, V) and the amount of blood (perfusion, Q) in the lungs. This is referred to as ventilation/perfusion (V/Q) mismatch.
There are two types of V/Q mismatch. Both produce dead space, regions of broken down or blocked lung tissue. Dead spaces can severely impact breathing, because they reduce the surface area available for gas diffusion. As a result, the amount of oxygen in the blood decreases, whereas the carbon dioxide level increases. Dead space is created when no ventilation and/or perfusion takes place. Anatomical dead space or anatomical shunt, arises from an anatomical failure, while physiological dead space or physiological shunt arises from a functional impairment of the lung or arteries.
An example of an anatomical shunt is the effect of gravity on the lungs. The lung is particularly susceptible to changes in the magnitude and direction of gravitational forces. When someone is standing or sitting upright, the pleural pressure gradient leads to increased ventilation further down in the lung. As a result, the intrapleural pressure is more negative at the base of the lung than at the top, and more air fills the bottom of the lung than the top. Likewise, it takes less energy to pump blood to the bottom of the lung than to the top when in a prone position. Perfusion of the lung is not uniform while standing or sitting. This is a result of hydrostatic forces combined with the effect of airway pressure. An anatomical shunt develops because the ventilation of the airways does not match the perfusion of the arteries surrounding those airways. As a result, the rate of gas exchange is reduced. Note that this does not occur when lying down, because in this position, gravity does not preferentially pull the bottom of the lung down.
A physiological shunt can develop if there is infection or edema in the lung that obstructs an area. This will decrease ventilation but not affect perfusion; therefore, the V/Q ratio changes and gas exchange is affected.
The lung can compensate for these mismatches in ventilation and perfusion. If ventilation is greater than perfusion, the arterioles dilate and the bronchioles constrict. This increases perfusion and reduces ventilation. Likewise, if ventilation is less than perfusion, the arterioles constrict and the bronchioles dilate to correct the imbalance.
Link to Learning
Section Summary
The structure of the lungs and thoracic cavity control the mechanics of breathing. Upon inspiration, the diaphragm contracts and lowers. The intercostal muscles contract and expand the chest wall outward. The intrapleural pressure drops, the lungs expand, and air is drawn into the airways. When exhaling, the intercostal muscles and diaphragm relax, returning the intrapleural pressure back to the resting state. The lungs recoil and airways close. The air passively exits the lung. There is high surface tension at the air-airway interface in the lung. Surfactant, a mixture of phospholipids and lipoproteins, acts like a detergent in the airways to reduce surface tension and allow for opening of the alveoli.
Breathing and gas exchange are both altered by changes in the compliance and resistance of the lung. If the compliance of the lung decreases, as occurs in restrictive diseases like fibrosis, the airways stiffen and collapse upon exhalation. Air becomes trapped in the lungs, making breathing more difficult. If resistance increases, as happens with asthma or emphysema, the airways become obstructed, trapping air in the lungs and causing breathing to become difficult. Alterations in the ventilation of the airways or perfusion of the arteries can affect gas exchange. These changes in ventilation and perfusion, called V/Q mismatch, can arise from anatomical or physiological changes.
Review Questions
Critical Thinking Questions
Glossary
- alveolar ventilation
- how much air is in the alveoli
- anatomical dead space
- (also, anatomical shunt) region of the lung that lacks proper ventilation/perfusion due to an anatomical block
- compliance
- measurement of the elasticity of the lung
- dead space
- area in the lung that lacks proper ventilation or perfusion
- elastic recoil
- property of the lung that drives the lung tissue inward
- elastic work
- work conducted by the intercostal muscles, chest wall, and diaphragm
- flow-resistive
- work of breathing performed by the alveoli and tissues in the lung
- functional vital capacity (FVC)
- amount of air that can be forcibly exhaled after taking the deepest breath possible
- intercostal muscle
- muscle connected to the rib cage that contracts upon inspiration
- intrapleural space
- space between the layers of pleura
- obstructive disease
- disease (such as emphysema and asthma) that arises from obstruction of the airways; compliance increases in these diseases
- physiological dead space
- (also, physiological shunt) region of the lung that lacks proper ventilation/perfusion due to a physiological change in the lung (like inflammation or edema)
- pleura
- tissue layer that surrounds the lungs and lines the interior of the thoracic cavity
- pleurisy
- painful inflammation of the pleural tissue layers
- recruitment
- process of opening airways that normally remain closed when the cardiac output increases
- resistance
- measurement of lung obstruction
- respiratory distress syndrome
- disease that arises from a deficient amount of surfactant
- respiratory rate
- number of breaths per minute
- restrictive disease
- disease that results from a restriction and decreased compliance of the alveoli; respiratory distress syndrome and pulmonary fibrosis are examples
- surfactant
- detergent-like liquid in the airways that lowers the surface tension of the alveoli to allow for expansion
- ventilation/perfusion (V/Q) mismatch
- region of the lung that lacks proper alveolar ventilation (V) and/or arterial perfusion (Q)