21.5 Disruptions in the Immune System
Mary Ann Clark; Jung Choi; and Matthew Douglas
Learning Objectives
By the end of this section, you will be able to do the following:
- Describe hypersensitivity
- Define autoimmunity
A functioning immune system is essential for survival, but even the sophisticated cellular and molecular defenses of the mammalian immune response can be defeated by pathogens at virtually every step. In the competition between immune protection and pathogen evasion, pathogens have the advantage of more rapid evolution because of their shorter generation time and other characteristics. For instance, Streptococcus pneumoniae (bacterium that cause pneumonia and meningitis) surrounds itself with a capsule that inhibits phagocytes from engulfing it and displaying antigens to the adaptive immune system. Staphylococcus aureus (bacterium that can cause skin infections, abscesses, and meningitis) synthesizes a toxin called leukocidin that kills phagocytes after they engulf the bacterium. Other pathogens can also hinder the adaptive immune system. HIV infects TH cells via their CD4 surface molecules, gradually depleting the number of TH cells in the body; this inhibits the adaptive immune system’s capacity to generate sufficient responses to infection or tumors. As a result, HIV-infected individuals often suffer from infections that would not cause illness in people with healthy immune systems but which can cause devastating illness to immune-compromised individuals. Maladaptive responses of immune cells and molecules themselves can also disrupt the proper functioning of the entire system, leading to host cell damage that could become fatal.
Immunodeficiency
Failures, insufficiencies, or delays at any level of the immune response can allow pathogens or tumor cells to gain a foothold and replicate or proliferate to high enough levels that the immune system becomes overwhelmed. Immunodeficiency is the failure, insufficiency, or delay in the response of the immune system, which may be acquired or inherited. Immunodeficiency can be acquired as a result of infection with certain pathogens (such as HIV), chemical exposure (including certain medical treatments), malnutrition, or possibly by extreme stress. For instance, radiation exposure can destroy populations of lymphocytes and elevate an individual’s susceptibility to infections and cancer. Dozens of genetic disorders result in immunodeficiencies, including Severe Combined Immunodeficiency (SCID), Bare lymphocyte syndrome, and MHC II deficiencies. Rarely, primary immunodeficiencies that are present from birth may occur. Neutropenia is one form in which the immune system produces a below-average number of neutrophils, the body’s most abundant phagocytes. As a result, bacterial infections may go unrestricted in the blood, causing serious complications.
Hypersensitivities
Maladaptive immune responses toward harmless foreign substances or self-antigens that occur after tissue sensitization are termed hypersensitivities. The types of hypersensitivities include immediate, delayed, and autoimmunity. A large proportion of the population is affected by one or more types of hypersensitivity.
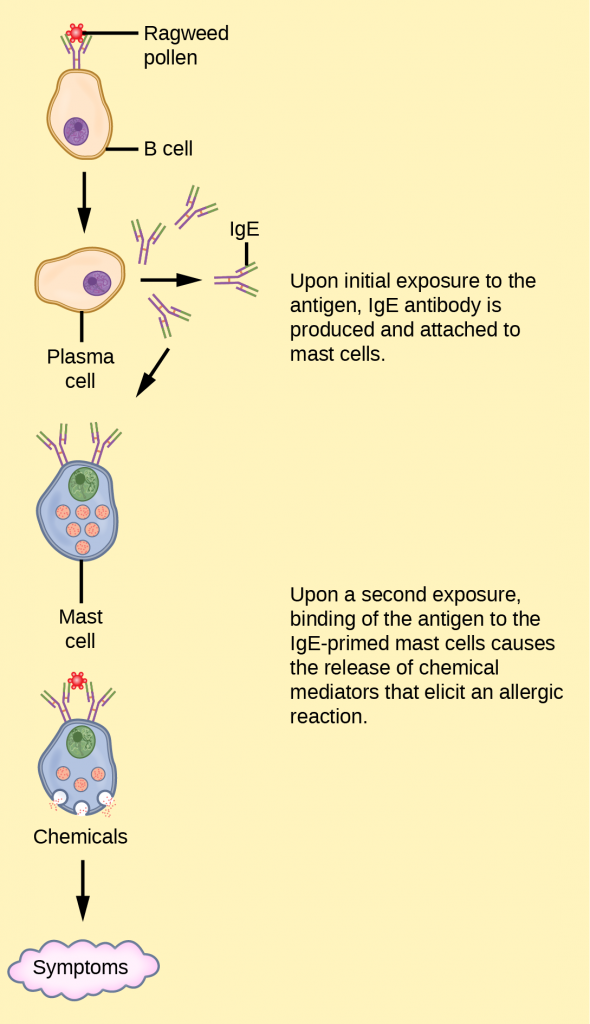
Allergies
The immune reaction that results from immediate hypersensitivities in which an antibody-mediated immune response occurs within minutes of exposure to a harmless antigen is called an allergy. In the United States, 20 percent of the population exhibits symptoms of allergy or asthma, whereas 55 percent test positive against one or more allergens. Upon initial exposure to a potential allergen, an allergic individual synthesizes antibodies of the IgE class via the typical process of APCs presenting processed antigen to TH cells that stimulate B cells to produce IgE. This class of antibodies also mediates the immune response to parasitic worms. The constant domain of the IgE molecules interacts with mast cells embedded in connective tissues. This process primes, or sensitizes, the tissue. Upon subsequent exposure to the same allergen, IgE molecules on mast cells bind the antigen via their variable domains and stimulate the mast cell to release the modified amino acids histamine and serotonin; these chemical mediators then recruit eosinophils, which mediate allergic responses. The figure below shows an example of an allergic response to ragweed pollen. The effects of an allergic reaction range from mild symptoms like sneezing and itchy, watery eyes to more severe or even life-threatening reactions involving intensely itchy welts or hives, airway contraction with severe respiratory distress, and plummeting blood pressure. This extreme reaction is known as anaphylactic shock. If not treated with epinephrine to counter the blood pressure and breathing effects, this condition can be fatal.
Delayed hypersensitivity is a cell-mediated immune response that takes approximately one to two days after secondary exposure for a maximal reaction to be observed. This type of hypersensitivity involves the TH1 cytokine-mediated inflammatory response and may manifest as local tissue lesions or contact dermatitis (rash or skin irritation). Delayed hypersensitivity occurs in some individuals in response to contact with certain types of jewelry or cosmetics. Delayed hypersensitivity facilitates the immune response to poison ivy and is also the reason why the skin test for tuberculosis results in a small region of inflammation in individuals who were previously exposed to Mycobacterium tuberculosis. That is also why cortisone is used to treat such responses: it will inhibit cytokine production.
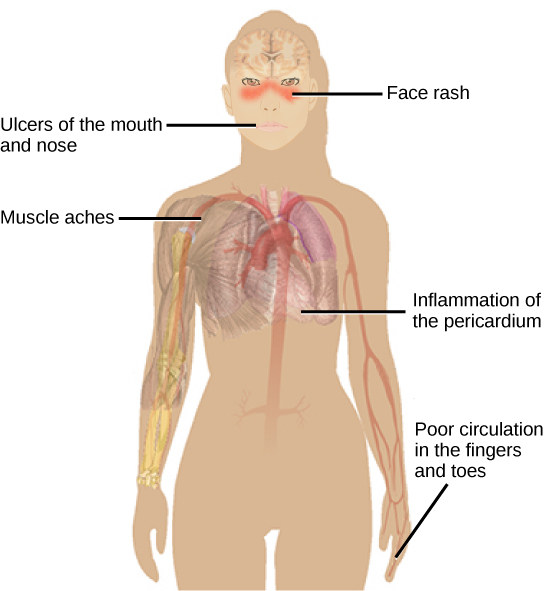
Autoimmunity
Autoimmunity is a type of hypersensitivity to self-antigens that affects approximately five percent of the population. Most types of autoimmunity involve the humoral immune response. Antibodies that inappropriately mark self components as foreign are termed autoantibodies. In patients with the autoimmune disease myasthenia gravis, muscle cell receptors that induce contraction in response to acetylcholine are targeted by antibodies. The result is muscle weakness that may include marked difficultly with fine and/or gross motor functions. In systemic lupus erythematosus, a diffuse autoantibody response to the individual’s own DNA and proteins results in various systemic diseases. As illustrated in the figure below, systemic lupus erythematosus may affect the heart, joints, lungs, skin, kidneys, central nervous system, or other tissues, causing tissue damage via antibody binding, complement recruitment, lysis, and inflammation.
Autoimmunity can develop with time, and its causes may be rooted in molecular mimicry. Antibodies and TCRs may bind self-antigens that are structurally similar to pathogen antigens, which the immune receptors first raised. As an example, infection with Streptococcus pyogenes (bacterium that causes strep throat) may generate antibodies or T cells that react with heart muscle, which has a similar structure to the surface of S. pyogenes. These antibodies can damage heart muscle with autoimmune attacks, leading to rheumatic fever. Insulin-dependent (Type 1) diabetes mellitus arises from a destructive inflammatory TH1 response against insulin-producing cells of the pancreas. Patients with this autoimmunity must be injected with insulin that originates from other sources.
Section Summary
Immune disruptions may involve insufficient immune responses or inappropriate immune targets. Immunodeficiency increases an individual’s susceptibility to infections and cancers. Hypersensitivities are misdirected responses either to harmless foreign particles, as in the case of allergies, or to host factors, as in the case of autoimmunity. Reactions to self components may be the result of molecular mimicry.
Review Questions
Glossary
- allergy
- immune reaction that results from immediate hypersensitivities in which an antibody-mediated immune response occurs within minutes of exposure to a harmless antigen
- autoantibody
- antibody that incorrectly marks “self” components as foreign and stimulates the immune response
- autoimmunity
- type of hypersensitivity to self-antigens
- hypersensitivities
- spectrum of maladaptive immune responses toward harmless foreign particles or self-antigens; occurs after tissue sensitization and includes immediate-type (allergy), delayed-type, and autoimmunity
- immunodeficiency
- failure, insufficiency, or delay at any level of the immune system, which may be acquired or inherited

