243 Nursing Copy / Paste
Learning Objectives
By the end of this section, you will be able to:
- Compare and contrast different forms of communication
- Define and describe the four levels of communication
Communication in health care is essential. The act of communication involves the sharing of ideas and thoughts among people, and it should be clear, honest, and confidential. For healthcare providers to offer care, they require information from the patient, and effective communication is the best way to obtain that information. Patients should feel comfortable sharing medical information with their healthcare providers, and they must never feel intimidated, fearful, or disrespected. This includes sharing trauma from life experiences, such as rape or previous medical incidents involving themselves or their family members. Healthcare communication also includes helping patients navigate the healthcare system, fill out forms, and make appointments.
Healthcare providers must consider the patient’s health and general literacy levels when engaging in communication. The ability of a patient to understand and use information to make health-related decisions is known as health literacy. For example, does the patient fully comprehend the benefits and drawbacks of a prescription, or does the patient understand the benefit of a follow-up appointment? When a patient has health literacy, they understand the health information being provided.
Healthcare providers should offer culturally competent care to the patient. Providing culturally competent care includes meeting and respecting a patient’s social, cultural, and linguistic needs while providing care. For example, to provide culturally competent care for a patient who is deaf, the nurse should include an interpreter who is fluent in American Sign Language, which meets the linguistic needs of the patient. When the healthcare provider does not prioritize culturally competent care, gaps in communication occur, and the health care provided may be deficient. Providing for the patient’s needs during communication challenges is paramount to patient-centered, high-quality care.
Healthcare providers need to communicate effectively with other members of the healthcare team while maintaining patient confidentiality. The healthcare team is considered interdisciplinary, or relating to more than one branch of knowledge, and interdisciplinary care includes team members from other healthcare professions, such as physical therapists or pharmacists. When multiple healthcare professionals from various disciplines collaborate on patient care, communication breakdowns may result. Inadequate or inappropriate communication can lead to errors, compromising patient care and outcomes.
Cultural Context
Healthcare Interpreters
Healthcare interpreters used in a healthcare setting should not be family members or healthcare staff members. Family members should not be used because they may not be familiar with medical terms, which may lead to incorrect translation. Healthcare staff members should not be used as interpreters because it can be a violation of patient privacy. Nurses should seek out healthcare interpreters who are certified by the National Board of Certification for Medical Interpreters. The legal requirements for medical interpreters (Title VI of the Civil Rights Act) require organizations that receive federal funds, including Medicare, Medicaid, and the Affordable Care Act, to provide a professional medical interpreter (Patient Engagement Hit, 2022). Healthcare facilities should have lists of preapproved medical interpreters for better communication with patients. Some facilities may use electronic means, such as video chat or a telephone, for interpretation (NCBMI, 2016).
Forms of Communication
Communication is the sharing of ideas and thoughts among people and the means of sending or receiving information. Communication requires a sender and a receiver. There are five forms of communication: verbal, nonverbal, written, visual, and electronic (Table 2.1). These forms may be used alone or in combination with another. Communication is better received and understood if more than one form is utilized (Mosaic Projects, n.d.). For example, when a nurse attends a verbal lecture on the latest medical equipment and has the opportunity to ask questions during the lecture, they are more likely to receive all the intended communication because more than one communication method was utilized: verbal and visual. Combining different forms of communication can make the message clearer for the receiver. To be most effective, nurses should ask the patient their preferred form of communication.
| Type of Communication | Example |
|---|---|
| Verbal | Spoken word |
| Nonverbal | Facial expressions and gestures |
| Written | Text messages |
| Visual | Emojis |
| Electronic | Electronic health record |
Verbal Communication
The term verbal communication can be defined as the production of spoken language to send to a listener. Verbal communication can include aspects of pitch, tone, volume, pace, clarity, pronunciation, and content. The pitch of verbal communication can be affected by the situation. For instance, a person who is communicating with an infant may use a higher pitch when talking so the infant can learn sound patterns to develop speech. The tone of the verbal communication can convey information to the listener. For example, an angry person may have a curt or rude tone, which may change the way the communication is received.
Content is important in verbal communication, especially among healthcare providers. When healthcare providers speak medical jargon to patients, much of the intended communication can be lost. Healthcare providers should carefully consider their words when communicating with patients.
Healthcare providers need to recognize that some patients have specific considerations for communication. For example, the patient may be a non-native speaker of the language the healthcare provider is speaking, making communication difficult. Or a patient could have a clinical condition that affects their ability to communicate verbally, such as a stroke or a cleft palate. In these instances, the healthcare provider should carefully consider their communication techniques and make appropriate accommodations when necessary. It is important for nurses to assess the patient’s level of health literacy, any medical condition impacting communication, or other barriers when first providing care.
There are specific standards that healthcare providers must respect when providing communication. The Health Insurance Portability and Accountability Act (HIPAA), a federal law creating the national standards to protect sensitive patient health information from being disclosed, describes the dangers of violating patient privacy with careless or unmonitored communication. The HIPAA laws govern not only verbal communication but also all other forms of communication. Healthcare providers need to be familiar with HIPAA laws so that they can assure the patient’s privacy and avoid violating the law. For instance, a patient has the right to specify who has access to their chart, and if it is discovered that this right has been violated by the healthcare provider, the healthcare provider can incur criminal penalty with possible fines or jail time (U.S. Department of Health and Human Services, n.d.).
Nonverbal Communication
The term nonverbal communication can be defined as all communication that is not spoken, including facial expressions, posture, eye contact, gestures, and physical touch. When a healthcare provider communicates with a patient, they should make their verbal and nonverbal communication congruent. When noncongruent messages are sent, the receiver is more likely to pay attention to the nonverbal communication than the verbal communication. Head nodding conveys acceptance, and the healthcare provider should use this nonverbal communication when agreeing verbally with the patient.
Eye contact is important for healthcare providers, especially when delivering verbal communication that is unpleasant. If the healthcare provider maintains eye contact throughout the communication, the healthcare provider is more likely to be viewed as respectful and honest (Baugh et al., 2020). Some patient conditions may rely heavily on nonverbal communication. For example, if a patient is blind, using nonverbal communication like touch is appropriate. The healthcare provider should use caution when communicating nonverbally, assessing the patient’s situation carefully (Bambaeeroo & Shokrpourm, 2017).
Healthcare providers should be attuned to diverse cultural norms in nonverbal communication. For example, in some cultures, eye contact is considered disrespectful. When providing culturally competent care, the nurse should ask the patient about their cultural beliefs and respect those beliefs. Healthcare providers can use touch to convey encouragement; however, the healthcare provider should respect the patient’s boundaries and cultural norms when using touch.
Unfolding Case Study
Unfolding Case Study #1: Part 1
The nurse is conducting the initial assessment on a 28-year-old patient who presents to the family walk-in clinic. The patient is accompanied by her 10-year-old son.
| Past Medical History | Patient is a mother of one, who cares for her child and older mother in a small apartment. The older mother is homebound and is not present at the appointment. The patient engages in housecleaning to financially support her family; however, the income is inconsistent. Patient has an eighth-grade education, is a native Spanish speaker, and does not speak English. Medical history includes seasonal allergies, sinusitis, and two episodes of COVID-19 in the past two years. Family history: Patient’s father is deceased, and patient’s mother has stage II Alzheimer disease. Patient’s son is in good health, talkative, and attentive to his mother. Social history: Patient is primary caregiver for older mother and son. No other support systems available. Patient has difficulty shopping and making doctor appointments due to lack of care for the mother. Patient has difficulty communicating in English, so the son translates for his mother. No current medications and no known allergies. |
| Nursing Notes | 1630: Triage Assessment Patient responds to gestures but speaks little English. Son provides translation for his Spanish-speaking mother. Patient reports frequent coughing episodes with production of large amounts of yellow sputum, which are exacerbated with activity. Patient is alert and cooperative, but son reports frequent periods of lethargy, sleepiness, and states “Momma feels hot and sweaty.” Patient holds the side of her head in her hands. Son reports patient has been complaining of an earache for three days. Patient intermittently grabs at ear and grimaces. |
| Flow Chart | 1630: Triage Assessment Blood pressure: 142/88 mmHg Heart rate: 100 beats/minute Respiratory rate: 24 breaths/minute Temperature: 101.1°F (38.4°C) Oxygen saturation: 95 percent on room air Pain: 8/10 (ear) |
| Lab Results | CBC: (Abnormal) WBC 17,000 WBCs per microliter (4.5 to 11.0 × 109/L). Rapid strep test: negative Rapid COVID test: negative |
Written Communication
Any written message, from formal letters to text messages, is considered written communication. Written communication may be thought of as the most prevalent form of communication; however, miscommunication can occur with written communication, dependent on the person’s learning style and ability to read (Vermeir et al., 2015). To create clear written communication, the healthcare provider should concentrate on providing good structure, clarity, and content. Using paragraphs, punctuation, and line breaks may help the reader better receive the written communication, as reading long paragraphs of text can increase miscommunication. Clarity and content are equally important, as is understanding the patient receiving the message. Written communication can be referred back to by patients for clarification after the encounter with the healthcare provider is over.
Because text messages are not secure, they should not be used for discussing protected health information with other providers. Text messaging is appropriate for providers to communicate with patients if the patient has provided written consent. Utilizing text messaging for patient communication should only be done by following the policies of the healthcare organization. Text messaging can also be used among providers, with secure electronic messaging, using either healthcare facility internal messaging or certain platforms recommended by the healthcare facility as secure, as unsecure communication between providers is more likely to violate HIPAA guidelines.
Visual Communication
In visual communication, visual elements are used to create the message for communication. Visual communication includes forms of communication that can be seen, such as charts, photographs, sketches, videos, models, graphs, and emojis. Healthcare providers rely on visual communication as it can help to explain complex concepts of health (Osbourne, 2006; Figure 2.2). When creating visual communication, choose images, fonts, and colors carefully, keeping in mind the audience. If the nurse is creating a visual presentation for patients who have visual challenges, such as a patient who has red-green color deficiency, attention to color, font, and background of the communication should be addressed. For example, a patient with visual challenges may have difficulty reading smaller font or distinguishing between colors for font and background.
Electronic Communication
All communication transmitted electronically is electronic communication. Electronic communication can include faxes and text messages that are broadcast, transmitted, stored, or viewed using electronic media like computers or cell phones. Electronic communication is growing in popularity in health care (Yang et al., 2022). Patient portals provide patient access to their own health information. Healthcare providers can readily access most patient records through electronic communication. Electronic communication may help healthcare providers treat patients more effectively, reduce medical errors, and improve patient safety (Rodiewicz et al., 2023). For instance, a healthcare provider could view imaging reports, lab values, or consult with a specialist all in one place to possibly avoid medical error. The electronic health record (EHR) and the electronic medical record (EMR) are the most common forms of electronic communication between patients and healthcare providers. An EHR is a digital format of a complete medical record of a patient that is able to be shared across multiple healthcare organizations. In contrast, EMRs capture the medical chart within a single healthcare organization and are not transferable to other settings. HIPAA laws govern this electronic information with the HIPAA Security Rule, a national standard to protect a patient’s electronic personal health information.
Listening
The ability to thoughtfully receive and interpret messages is called listening. The listener should be able to restate someone’s words after the speaker has finished. Listening can be active or passive. When someone listens by giving their full attention, listening to understand, and providing thoughtful input, they are active listening; when someone listens to simply hear the messages being sent but may not be mentally or emotionally present and does not engage in the communication process, they are passive listening. Healthcare providers should use active listening including both verbal and nonverbal communication. Passive listening includes nonverbal communication only, and if the listener speaks, then it is considered active listening.
Healthcare providers must be actively listening as patients are giving them information that helps them treat the patient safely and effectively. Nurses also need to recognize when the patient may not understand the messages received, even though the patient provided nonverbal communication like a head nod that they understood. For example, when the patient is asked to repeat the instructions received, the nurse may find that there are discrepancies. The nurse needs to ensure the listener understands, preventing discrepancies regarding the patient’s medical care.
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8[1] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports. Reports may be verbal (e.g., reports given in person, by telephone, or recorded) or written (e.g., reports provided electronically or by fax).

Reports to Health Care Team Members
Nurses routinely report information to other nurses and health care team members, as well as urgently contact health care providers to report changes in client status.
Standardized methods of communication have been developed to allow information to be exchanged between health care team members in a structured, concise, and accurate manner to ensure safe client care. One common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back or a simpler version called SBAR:
-
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the client’s name and location, why you are calling, recent vital signs, and the status of the client.
- Background: Provide pertinent background information about the client such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current client situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the client, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the client’s chart.
Read an example of an ISBARR report in the following box. Information is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. The client has no known allergies and is a full code. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site, and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear, and her heart rate is regular. I am concerned her incision site may be becoming infected and that she will have difficulty with therapy if her pain remains uncontrolled.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of client care responsibility achieved through effective communication. It is a real-time process of passing client specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the client’s care.”[2] In 2017, The Joint Commission issued a critical alert about inadequate handoff communication that has resulted in client harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase client safety, as well as client and nurse satisfaction, by effectively communicating current, accurate client information in real time.[3] See Figure 2.9[4] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the client, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the client’s bedside. HIPAA rules must be kept in mind if visitors are present, or the room is not a private room. Family members may be included with the client’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10.[5] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
![]"618721604-huge" by Rido is used under license from Shutterstock.com. Image showing two nurses discussing a chart both are holding](https://louis.pressbooks.pub/app/uploads/sites/2/2024/10/618721604-huge-scaled-1.jpg)
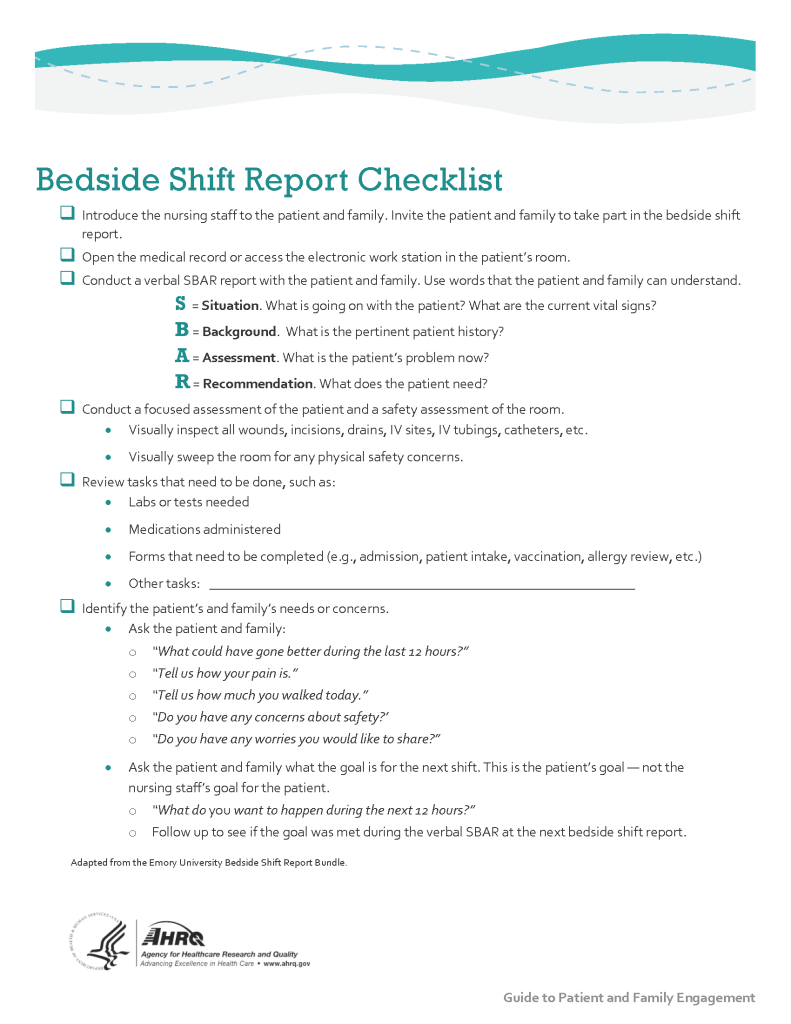
Print a copy of the AHRQ Bedside Shift Report Checklist.
View a video on creating shift reports.[6]
Transfer Reports
Transfer reports are provided by nurses when transferring a client to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports but are even more detailed when the client is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
Conflict in the Workplace
Nurses encounter conflict in their daily work environment, such as misunderstandings or disagreements among staff, clients, providers, family members, or other individuals. Nurses must learn communication methods that lessen conflict and enhance interactions that lead to a better work environment.
Read additional information about “Conflict Resolution” in Open RN Nursing Health Alterations.
Media Attributions
- Strat3_Tool_2_Nurse_Chklst_508
- “1322557028-huge.jpg” by LightField Studios is used under license from Shutterstock.com ↵
- The Joint Commission. (n.d.). Sentinel event alert 58: Inadequate hand-off reports. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-alert-newsletters/sentinel-event-alert-58-inadequate-hand-off-communication/ ↵
- Dorvil, B. (2018). The secrets to successful nurse bedside shift report implementation and sustainability. Nursing Management, 49(6), 20-25. https://doi.org/10.1097/01.NUMA.0000533770.12758.44 ↵
- “618721604-huge” by Rido is used under license from Shutterstock.com. ↵
- “Strat3_Tool_2_Nurse_Chklst_508.pdf” by AHRQ is licensed under CC0 ↵
- RegisteredNurseRN. (2015, May 23). Nursing shift report sheet templates | How to give a nursing shift report [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/X76iKFQhPNw ↵

