Fertilization and Childbirth
Fertilization
Fertilization occurs when a sperm and an oocyte (egg) combine. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell is called a zygote. Most of the time, a woman releases a single egg during an ovulation cycle. In approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times. Less common, one zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins.
Stages of Childbirth
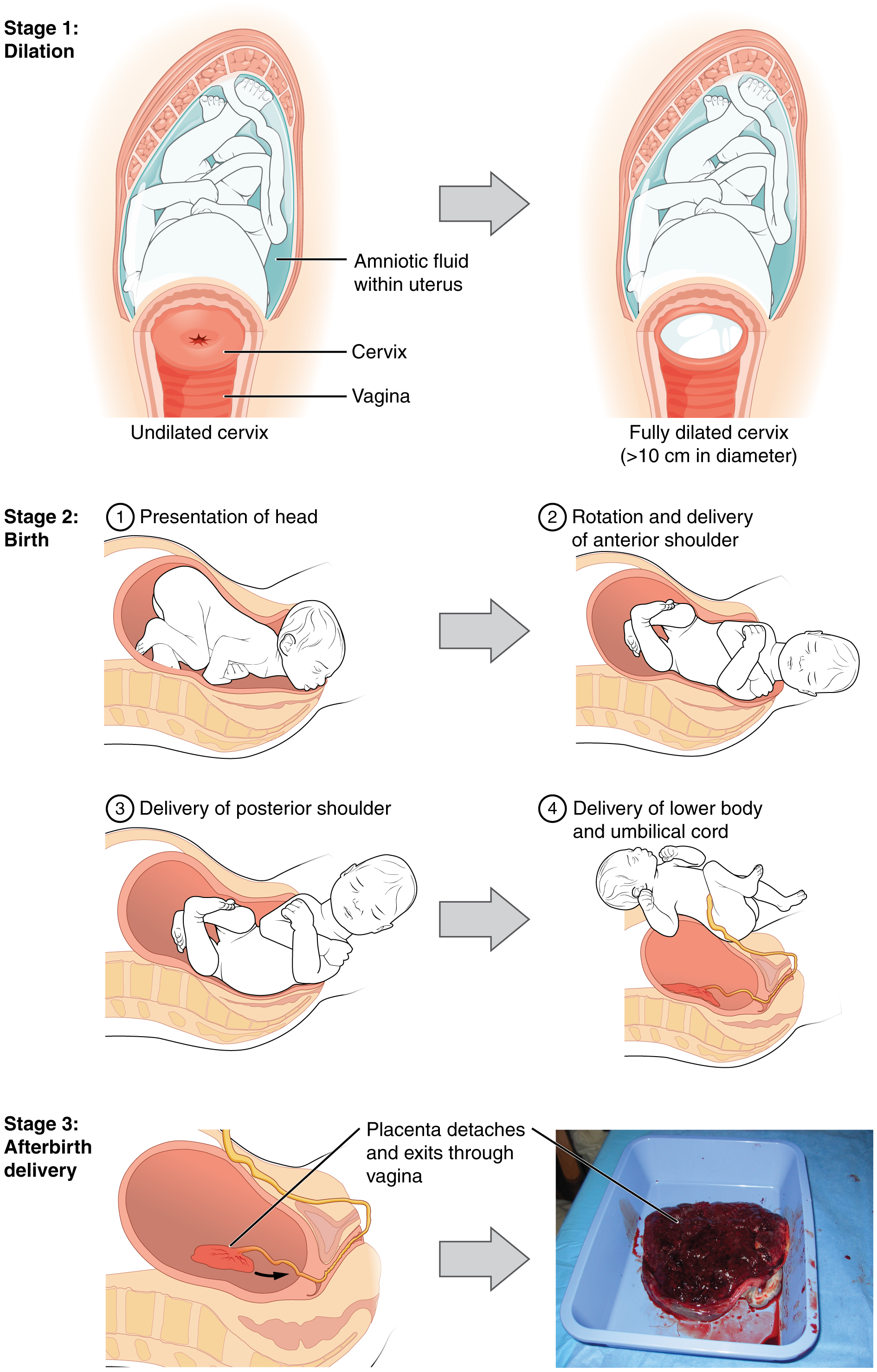
The process of childbirth can be divided into three stages (see Figure 16.2):
- Cervical dilation
- Expulsion of the newborn
- After birth
For vaginal birth to occur, the cervix must dilate fully to 10 cm in diameter, wide enough to deliver the newborn’s head. The dilation stage is the longest stage of labor and typically takes 6–12 hours. However, it varies widely and may take minutes, hours, or days, depending in part on whether the mother has given birth before. In each subsequent labor, this stage tends to be shorter.
Homeostasis in the Newborn: Apgar Score
In the minutes following birth, a newborn must undergo dramatic systemic changes to be able to survive outside the womb. An obstetrician, midwife, or nurse can estimate how well a newborn is doing by obtaining an Apgar score. The Apgar score was introduced in 1952 by the anesthesiologist Dr. Virginia Apgar as a method to assess the effects on the newborn of anesthesia given to the laboring mother. Health care providers now use it to assess the general well-being of the newborn, whether or not analgesics or anesthetics were used.
The five criteria—skin color, heart rate, reflex, muscle tone, and respiration—are assessed, and each criterion is assigned a score of 0, 1, or 2. Scores are taken at 1 minute after birth and again at 5 minutes after birth. Each time scores are taken, the five scores are added together. High scores (out of a possible 10) indicate the baby has made the transition from the womb well, whereas lower scores indicate that the baby may be in distress.
The technique for determining an Apgar score is quick and easy, is painless for the newborn, and does not require any instruments except for a stethoscope. A convenient way to remember the five scoring criteria is to apply the mnemonic APGAR:
- Appearance (skin color)
- Pulse (heart rate)
- Grimace (reflex)
- Activity (muscle tone)
- Respiration
Of the five Apgar criteria, heart rate and respiration are the most critical. Poor scores for either of these measurements may indicate the need for immediate medical attention to resuscitate or stabilize the newborn. In general, any score lower than 7 at the 5-minute mark indicates that medical assistance may be needed. A total score below 5 indicates an emergency situation. Normally, a newborn will get an intermediate score of 1 for some of the Apgar criteria and will progress to a 2 by the 5-minute assessment. Scores of 8 or above are normal.
Image Descriptions
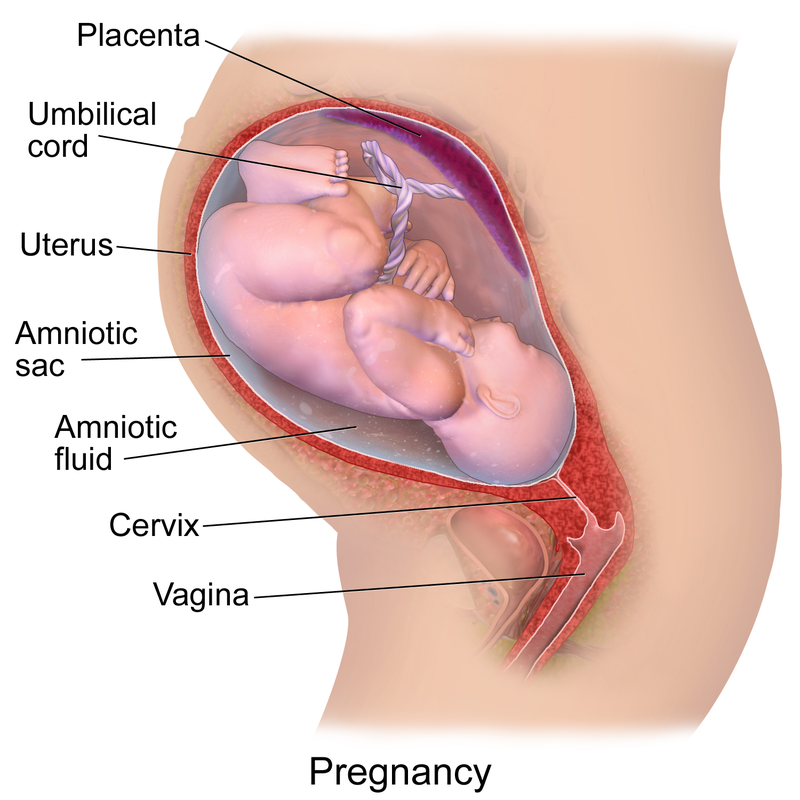
Figure 16.1 image description: This figure shows a gravid uterus and fetus during the last trimester of pregnancy. It shows the placenta, umbilical cord, uterus, amniotic sac, amniotic fluid, cervix, and vagina. [Return to Figure 16.1].
Figure 16.2 image description: This multi-part figure shows the different stages of childbirth. The top panel shows dilation of the cervix (undilated vs. fully dilated), the middle panel shows birth (presentation of the head, rotation and delivery of anterior shoulder, delivery of posterior shoulder, delivery of lower body and umbilical cord), and the bottom panel shows afterbirth delivery. [Return to Figure 16.2].

